Anterior myocardial pseudoinfarction in a patient with diabetic ketoacidosis
2018-05-23JoseRuizMoralesCatarinaCanhaFarahAlSaffarSaifIbrahim
Jose Ruiz-Morales, Catarina Canha, Farah Al-Saffar, Saif Ibrahim
1Internal medicine department, University of Florida, Jacksonville, FL, USA
2Cardiology Department, Mayo Clinic, Scottsdale, AZ, USA
3Cardiology Department, University of Florida, Jacksonville, FL, USA
Diabetic ketoacidosis remains one of the most serious complications of diabetes mellitus. Among its precipitating factors is myocardial ischemia, responsible for 1% of the cases of diabetic ketoacidosis.[1]Diabetic ketoacidosis both with and without hyperkalemia has been reported to mimic a myocardial infarction pattern on ECG with ST segment elevation, described as pseudoinfarction pattern.[1–3]Thus, it is important to raise awareness among physicians, as subjecting patients to invasive medical management can be avoided. We present a case of a 47-year-old female with diabetic ketoacidosis and hyperkalemia with initial ECG findings of ST segment elevation, but an urgent left heart catheterization revealed non-obstructive coronary disease.
A 47-year old female with diabetes mellitus type 2 presented to the hospital with a three-day course of polydipsia,nausea, vomiting and abdominal pain. The patient had been non-compliant with her insulin regimen for the past three days but otherwise history was unremarkable. Specifically,no history of cardiac disease or anginal symptoms were present. Initial assessment revealed a body temperature of 35.6 °C, blood pressure of 128/62, regular pulse with rate of 124 bpm and respiratory rate of 28 breaths/min. Except for poor skin turgor and tenderness upon abdominal palpation,the remainder of the findings of the physical exam were unremarkable. An ECG (Figure1) demonstrated sinus rhythm with ST-segment elevation in leads V1–V3 concerning for anterior myocardial infarction. The patient underwent emergent left heart catheterization which demonstrated non-obstructive coronary artery disease. Left ventricular end-diastolic pressure concerning for severe dehydration and left vetriculogram noted preserved ejection fraction. During the procedure, laboratory data revealed a white blood cell count of 40.46 × 103cells/µL, hemoglobin level of 13.3 g/dL and a platelet count of 539 × 103platelets/µL.Blood chemistry examination revealed a urea nitrogen value of 46 mg/dL, creatinine level of 2.04 mg/dL, creatinine kinase level of 140 U/L, CK-MB level of 5.7 ng/mL. Troponin I and Troponin T negative. Otherwise, she had a serum glucose level of 985 mg/dL, beta-hydroxybutyrate level> 45 mg/dL, sodium level of 118 mmol/L, potassium level of 6.7 mmol/L, bicarbonate 4 mmol/L, anion gap 40 mmol/L.The diagnosis of diabetic ketoacidosis was made, and the patient was transferred to the intensive care unit for medical management. She was administered Lactated Ringer’s solution and continuous insulin infusion (0.1 units/Kg/hr). One hour after starting the treatment for ketoacidosis, the following results were obtained: serum glucose 613 mg/dL,potassium 4.6, bicarbonate 5 mmol/L. The ECG was repeated (Figure 2), and it was observed that the ST segments were in isoelectric line. Cardiac enzymes remained negative,the patient never presented any cardiac complaint. She was transferred to a general medical ward and eventually discharged home.
Hyperkalemia is frequently seen in patients with diabetic ketoacidosis even though the total body potassium is depleted, this is due to acidosis, insulin deficiency and renal impairment.[1]Hyperkalemia can cause several characteristic ECG abnormalities that have been well described. Initially, the T wave becomes tall, symmetrically peaked, and tented and there is occasional QT interval shortening. Reduction of P wave amplitude and eventual disappearance is also seen. Widening of the QRS complex with various forms of intraventricular conduction delay then occurs. Further progression of hyperkalemia leads to a sine wave appearance of the ECG and eventual asystole. Rarely, ST-segment elevation mimicking myocardial infarction, described as a“pseudoinfarction” pattern, is present.[3,4]
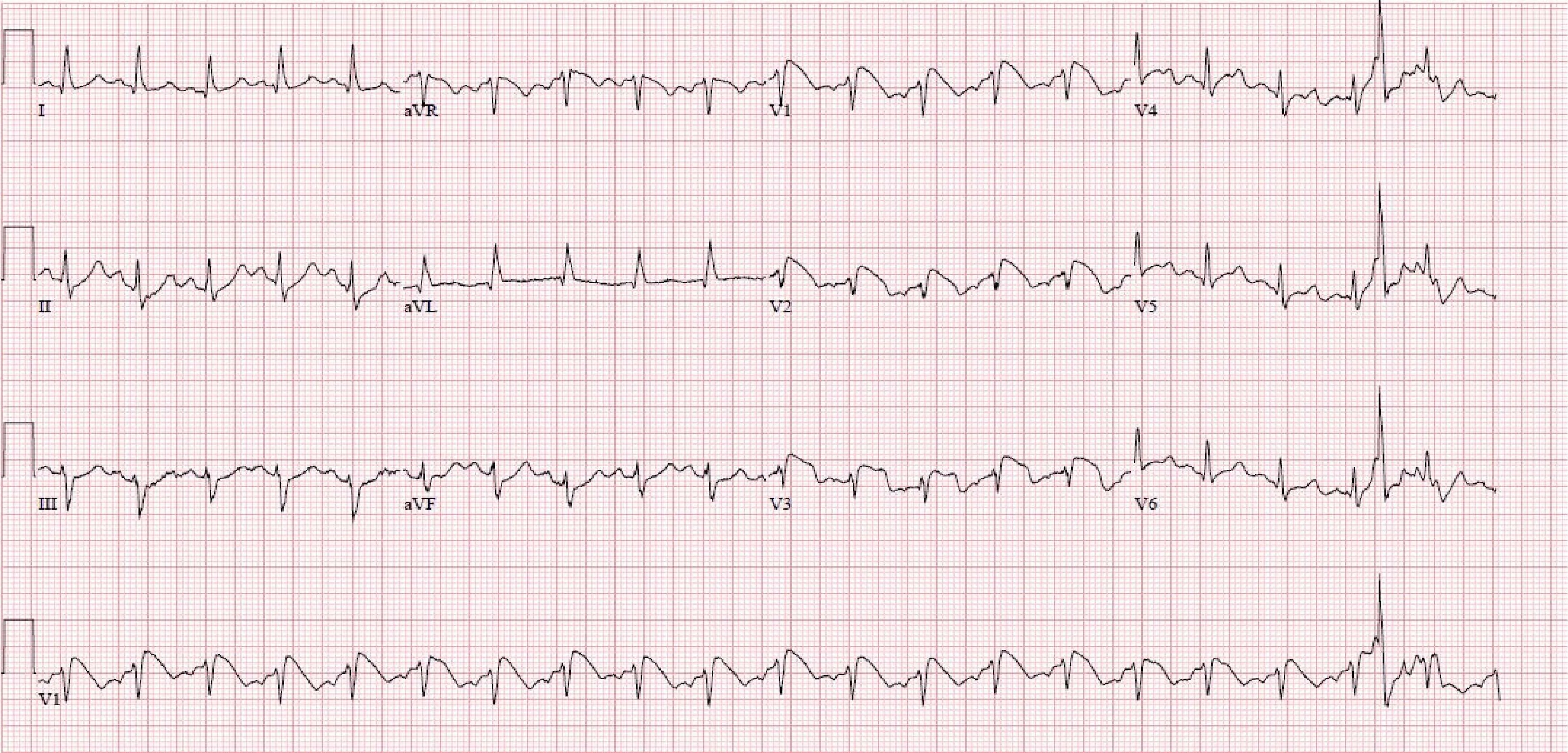
Figure 1. ECG on presentation demonstrating ST elevations on anterior leads V1–V3.
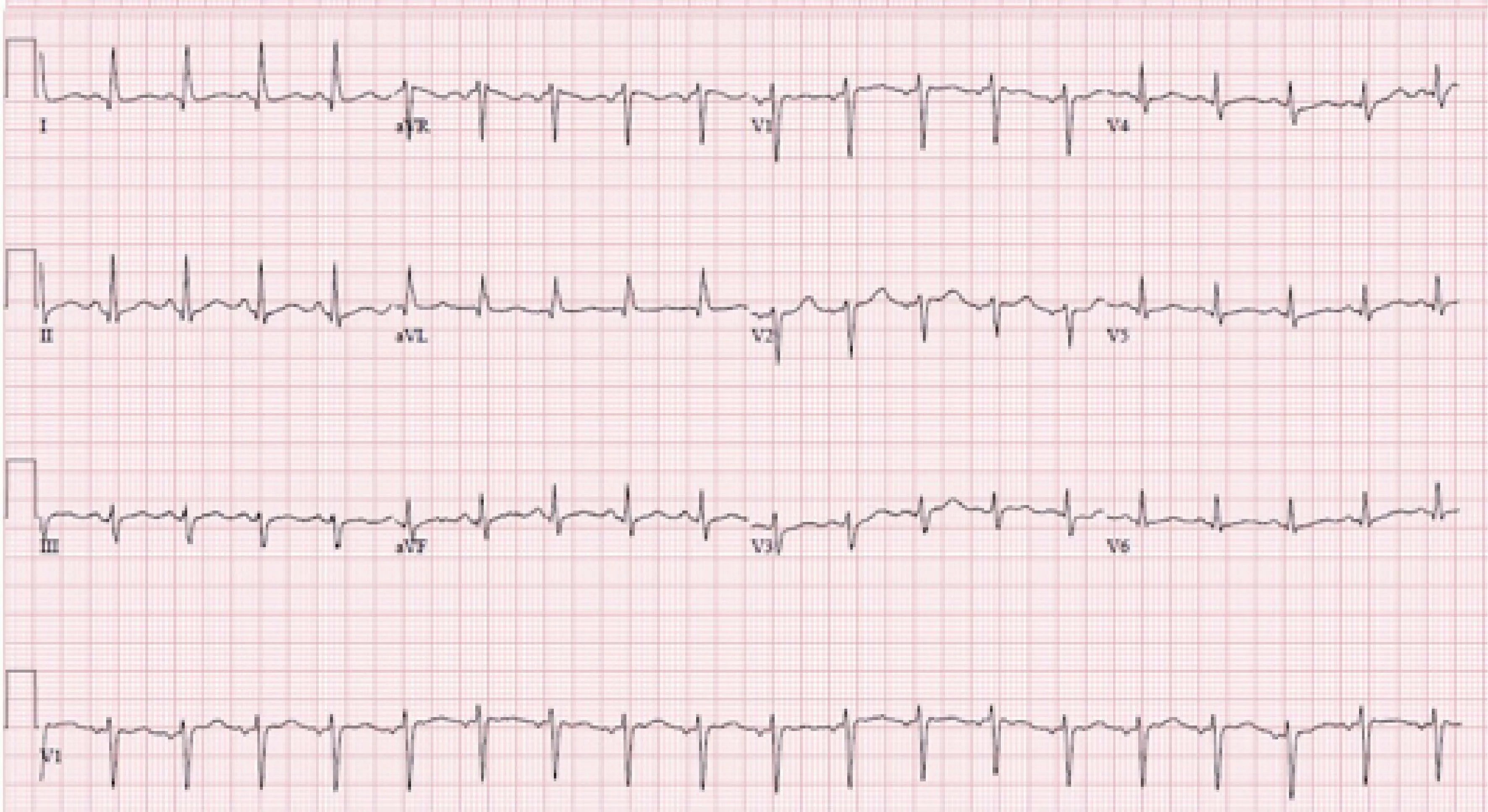
Figure 2. ECG demonstrating normalization of ST changes after fluid and DKA management. DKA: Diabetic Ketoacidosis.
The pseudoinfarction pattern has been reported mostly in association with hyperkalemia associated with Diabetic Ketoacidosis (DKA) as well as in patients with end stage renal disease.[5]Furthermore, this abnormality is uncommon in hyperkalemia alone[4]and a case of pseudoinfarction in DKA with normokalemia has also been reported.[2]Which raises the question on whether hyperkalemia is solely responsible for this pattern or metabolic acidosis/other metabolic abnormalities are implicated in this finding.
In addition, myocardial infarction occurs when the atheromatous process prevents blood flow through the coronary artery.[6]Furthermore, according to Poiseuille’s law,blood viscosity is inversely related to flow.[7]Therefore, if blood viscosity is elevated, this could reduce myocardial perfusion and consequently lead to the observed ST elevation noted on the ECG. This is of interest because blood viscosity seems to be increased in patients with diabetes mellitus. The reasons remain unclear but it is believed that the increase in osmolarity causes increased capillary permeability and,consequently, increased hematocrit and viscosity. It has also been suggested that the osmotic diuresis, consequence of hyperglycemia, could contribute to reduce plasma volume and increase hematocrit.[8]
This case report illustrates an unusual reversible ECG finding in a patient with diabetic ketoacidosis, hyperkalemia and hyperosmolarity capable of mimicking a myocardial infarction (pseudoinfarction pattern). Because myocardial infarction may precipitate DKA and because many diabetic patients present with silent myocardial infarction, a ST segment elevation finding on ECG can prompt immediate and unnecessary actions. Therefore, it is important for the physician to be familiarized with cases such as this to avoid unnecessary drug treatment, coronary angiography and its attendant risks.
References
1 Moulik PK, Nethaji C, Khaleeli AA,et al. Misleading electrocardiographic results in patient with hyperkalaemia and diabetic ketoacidosis.BMJ2002; 325: 1346–1347.
2 Aksakal E, Duman H, Ulus T,et al. Acute inferior pseudoinfarction pattern in a patient with normokalemia and diabetic ketoacidosis.Am J Emerg Med2009; 27: 251.e3–e5.
3 Sims DB, Sperling LS. Images in cardiovascular medicine.ST-segment elevation resulting from hyperkalemia.Circulation2005; 111: e295–e296.
4 LEVINE HD, WANZER SH, MERRILL JP,et al. Dialyzable currents of injury in potassium intoxication resembling acute myocardial infarction or pericarditis.Circulation1956; 13:29–36.
5 Sweterlitsch EM, Murphy GW. Acute electrocardiographic pseudoinfarction pattern in the setting of diabetic ketoacidosis and severe hyperkalemia.Am Heart J1996; 132: 1086–1089.
6 Hansson G. Inflammation, atherosclerosis, and coronary artery disease.N Engl J Med2005; 352: 1685–1695.
7 Guyton A, Hall J.Textbook of Medical Physiology. 10thedition;Philadelphia, PA, WB Saunders Company, 2000; 212–213.
8 Irace C, Carallo C, Scavelli F,et al. Blood viscosity in subjects with normoglycemia and prediabetes.Diabetes Car e2014; 37: 488–492.
杂志排行
Journal of Geriatric Cardiology的其它文章
- The contribution of gender and age on early and late mortality following ST-segment elevation myocardial infarction: results from the Korean Acute Myocardial Infarction National Registry with Registries
- Association between preoperative high sensitive troponin I levels and cardiovascular events after hip fracture surgery in the elderly
- The subcutaneous implantable cardioverter defibrillator––review of the recent data
- Should atrial fibrillation patients with hypertension as an additional risk factor of the CHA2DS2-VASc score receive oral anticoagulation?
- Successful conservative management of Class III iatrogenic aortic dissection
- Simultaneous multiple coronary arteries thrombosis in patients with STEMI
