Association between preoperative high sensitive troponin I levels and cardiovascular events after hip fracture surgery in the elderly
2018-05-23BumSungKimTaeHoonKimJeongHwanOhChangHeeKwonSungHeaKimHyunJoongKimHeungKonHwangSangManChung
Bum Sung Kim, Tae-Hoon Kim, Jeong-Hwan Oh, Chang Hee Kwon, Sung Hea Kim, Hyun-Joong Kim,Heung Kon Hwang, Sang-Man Chung
1Division of Cardiology, Department of Medicine, Konkuk University Medical Center, 120–1 Neungdong-ro, Hwayang-dong, Gwangjin-gu, Seoul, Republic of Korea
2Department of Orthopedic surgery, Konkuk University Medical Center, 120–1 Neungdong-ro, Hwayang-dong, Gwangjin-gu, Seoul, Republic of Korea
1 Introduction
Perioperative cardiovascular complications are a cause of morbidity and mortality in the > 200 million patients who undergo non-cardiac surgery worldwide each year.[1]Although orthopedic procedures have historically been thought to confer only an intermediate risk of death and nonfatal myocardial infarction (MI), perioperative cardiovascular events are not uncommon.[2,3]Among orthopedic injuries,hip fracture occurs frequently in elderly populations with a number of co-morbidities and functional disabilities, and following hip fracture surgery (HFS) is associated with postoperative complications, including adverse cardiac events.[4,5]The recent introduction of highly sensitive assays to detect the troponin has increased the early diagnosis of myocardial infarction and allowed the detection of previously undetectable levels of cardiac troponin in various patient groups who do not exhibit acute cardiac injury.[6–10]Several studies have since shown that even minimal increases in cardiac troponin are associated with unfavorable outcomes in various patient groups, including those undergoing non-cardiac surgery.[11]However, few studies have explored whether preoperative levels of troponin predict the cardiovascular course following HFS. Therefore, we used high sensitive troponin I (hs-TnI) and clinical parameters to identify preoperative risk factors associated with major adverse cardiac event in elderly hip fracture patients.
2 Methods
2.1 Study population
The study population was selected from the Cardiology-Orthopedics Consultation registry of Konkuk Medical Center, Seoul, South Korea. Between August 2014 and November 2016, 575 patients with hip fracture were enrolled in this single center registry, and 435 patients underwent hip fracture surgery. For the purpose of this analysis, we used inclusion and exclusion criteria. The inclusion criteria for the present study were as follows: (1) consecutive patients 18 years of age or older and (2) patients who underwent HFS and were preoperatively evaluated for hs-TnI. The exclusion criteria were the following: (1) patients with acute coronary syndrome or acute decompensated heart failure(HF) preoperatively, (2) patients with documented atrial fibrillation (AF)/flutter in a preoperative evaluation and (3)patients with insufficient preoperative clinical or laboratory data. A total of 262 patients were included in the final analysis. We separated the study population into a major adverse cardiac event (MACE) group and a non-MACE group according to the occurrence of MACE over a 90-day postoperative follow-up period. Clinical, laboratory, and outcome data were collected by a trained study coordinator who used a standardized case report form and protocol. The Institutional Review Board at Konkuk Medical Center approved the study protocol (KUH1010848) and waived the requirement for informed consent.
2.2 Perioperative evaluation and management
All patients underwent a complete baseline history survey,physical examination, 12-lead electrocardiogram (ECG),and laboratory exam during a preoperative cardiology consultation. Whether to perform a preoperative evaluation of biomarkers was left to the discretion of the cardiology consultation physician. Cardiac troponin-I was assessed using the ARCHITECT STAT High Sensitive Troponin-I immunoassay on an ARCHITECT i2000SR immunoassay analyzer (Abbott Diagnostics, USA). The limit of detection was 1.9 ng/L. The 99th percentile cut-off values were defined as 20.7 ng/L for men and 16.1 ng/L for women. Renal insufficiency was defined as an estimated glomerular filtration rate(eGFR) lower than 60 mL/min/1.73 m2(using the Modified Diet in Renal Disease equation) at initial presentation. The revised cardiac risk index (RCRI) was calculated for each patient. The RCRI relies on the presence or absence of the following 6 identifiable predictive factors: high-risk surgery(intrathoracic, intraperitoneal, or suprainguinal vascular surgery), ischemic heart disease, congestive heart failure, cerebrovascular disease, insulin therapy with diabetes mellitus,and renal dysfunction (serum creatinine level > 2.0 mg/dL).[12]Each of these predictors was assigned 1 point.Echocardiographic profiles were measured at an echocardiographic laboratory (Konkuk University Medical Center,Seoul, Korea) according to the protocol established by the American Society of Echocardiography. In postoperative management, the use of intravenous diuretics and transfusion was left to the discretion of the attending physician during postoperative care.
2.3 Study outcomes and definitions
The primary outcome was MACE. MACE was defined as the composite of all-cause deaths, postoperative HF, postoperative AF, postoperative MI and cardiovascular re-hospitalization that occurred within 90 days postoperative. Postoperative heart failure was defined as the appearance of appropriate clinical symptoms and signs of heart failure that required diuretics or postoperative ventilation. Postoperative AF was defined as evidence on a rhythm strip or 12-lead ECG showing AF or atrial flutter of any duration during the postoperative period. Postoperative MI was defined as creatine kinase MB isoform (CK-MB) levels that increased to >2 times the upper limit of normal in association with at least one of the following: new Q wave on ECG (≥ 30 ms in 2 continuous leads), persistent significant ST elevation or depression on ECG, or a new regional wall motion abnormality on ECG. Cardiovascular re-hospitalization was defined as readmission with a primary diagnosis of HF, AF or MI after discharge within 90 days postoperative. The secondary outcomes were the individual components of the primary outcome, including all-cause deaths, postoperative HF, postoperative AF, postoperative MI and cardiovascular re-hospitalization.
2.4 Statistical analysis
Continuous variables were compared using Student’s t-test or the Wilcoxon rank-sum test when applicable and are presented as the mean ± standard deviation (SD) or median with interquartile range (IQR). Categorical data were analyzed using the Chi-square test. A receiver-operating characteristic curve analysis was performed to estimate the hs-TnI or N-terminal pro-brain natriuretic peptide (NT-pro-BNP) values that predicated the development of MACE based on an estimated area under the curve (AUC). With respect for clinical outcomes predicted according to hs-TnI levels, cumulative event rates were estimated by the Kaplan- Meier method and compared using log-rank tests. The effects of putative risk factors on the development of MACE were analyzed using a Cox proportional hazard model. Crude HR was computed by introducing the risk factors into the model in a stepwise manner. To assess which variables were independent risk factors for the development of MACE at the time of implantation, we constructed a multivariate Cox proportional hazard model by adding the variables that were previously found to be significant (P< 0.05) in the univariate models. Adjusted hazard rates were compared by a Cox proportional hazard model based on an age of > 80 years old at the time of surgery, renal insufficiency, prior heart failure, ejection fraction(EF) < 50%, hs-TnI ≥ 6.5 ng/L, NT-proBNP ≥ 135 pg/dL,use of beta blockers and RCRI ≥ 1 point. We started with the variable that showed the strongest association first. All statistical analyses were performed with SPSS 20.0 (SAS Institute Inc., Cary, NC, USA). All tests were two-tailed,andP-values < 0.05 were considered statistically significant.
3 Results
3.1 Baseline characteristics
A total of 575 patients with hip fracture were enrolled in the registry. Of these, 435 patients underwent HFS, and of these, 173 patients were excluded (18 patients for preoperative acute coronary syndrome or acute decompensated heart failure, 17 for documented AF/flutter in a preoperative evaluation and 138 for insufficient preoperative clinical or laboratory data). The remaining 262 patients were classified into two groups, a MACE group (n= 197) and a non- MACE group(n= 65), according to whether they developed MACE within 90 days postoperative. The baseline characteristics of the two groups are shown in Table 1. The prevalence of old age,renal insufficiency, prior heart failure, low left ventricular ejection fraction, and the use of beta- blockers were higher;the preoperative values of creatinine, hs-TnI, CK-MB, NT-proBNP and RCRI were higher; and hemoglobin levels were lower in the MACE group than in the non-MACE group.

Table 1. Preoperative baseline characteristics in patients undergoing hip fracture surgery.
3.2 Predictive cut-off levels of preoperative biomarkers and clinical outcomes
On the basis of a receiver-operating characteristic analysis, the optimal preoperative hs-TnI and NT-proBNP cut-off levels for predicting the development of MACE in patients who undergo HFS were 6.5 ng/L and 135.2 pg/dL, respectively. hs-TnI had an AUC of 0.77 (95% CI: 0.70–0.83;P <0.001) with a sensitivity of 73.9% and a specificity of 68.5%, and NT-proBNP had an AUC of 0.69 (95% CI:0.62–0.78;P <0.001) with a sensitivity of 83.1% and a specificity of 39.1% (Supplement 1).
Overall, 155 of the 262 (59.2%) included patients had hs-TnI < 6.5 ng/L, and 107 (40.8%) patients had hs-TnI ≥6.5 ng/L. The baseline clinical characteristics are shown in supplement 2 according to the preoperative cut-off value for hs-TnI that predicted MACE development (hs-TnI > 6.5 ng/Lvs. hs-TnI ≤ 6.5 ng/L). Figure 1 and Table 2 demonstrate the clinical outcomes observed in the study population and a comparison of the unadjusted and adjusted hazard ratios between patients with hs-TnI ≥ 6.5 ng/L and those with hs-TnI < 6.5 ng/L. There was a higher risk of postoperative heart failure (adjusted HR: 2.32; 95% CI: 1.14–4.73;P< 0.02), postoperative atrial fibrillation (adjusted HR: 5.06;95% CI: 1.69–15.13;P= 0.004) and MACE (adjusted HR:3.42; 95% CI: 1.85–6.32;P< 0.001) in patients with hs-TnI≥ 6.5 ng/L than in those with hs-TnI < 6.5 ng/L. There was no significant difference between patients with hs-TnI ≥ 6.5 ng/L and those with hs-TnI < 6.5 ng/L with regard for the incidences of all-cause death, postoperative MI and cardiovascular re-hospitalization.

Table 2. Postoperative clinical outcome according to preoperative hs-TnI cut-off value.

Figure 1. Kaplan-Meier curve of major adverse cardiovascular events in all population according to hs-TnI cutoff value.hs-TnI: high sensitive troponin I; MACE: major adverse cardiovascular event.
3.3 Clinical outcomes according to RCRI subgroup
Figure 2 presents the risk of developing MACE according to hs-TnI levels in the subgroups with an RCRI of 0 and an RCRI of 1or more. In the RCRI 0 subgroup, MACE developed in 36 (18.5%) patients, 14 (7.2%) patients had hs-TnI < 6.5 ng/L, and 22 (11.3%) patients had hs-TnI ≥ 6.5 ng/L (adjusted HR: 2.34; 95% CI: 1.14–4.79;P= 0.02). In the RCRI 1 or more subgroup, MACE occurred in 29(43.2%) patients, 3 (4.4%) patients had hs-TnI < 6.5 ng/L,and 26 (38.8%) patients had hs-TnI ≥ 6.5 ng/L (adjusted HR:10.0; 95% CI: 2.41–41.82;P< 0.01).
3.4 Independent predictors of major adverse cardiac events

Figure 2. The frequency of major adverse cardiovascular events in the RCRI = 0 subgroup (A); and RCRI = 1 or more subgroups(B) according to hs-TnI cutoff value. hs-TnI: high sensitive troponin I; MACE: major adverse cardiovascular event; RCRI: revised cardiac risk index.
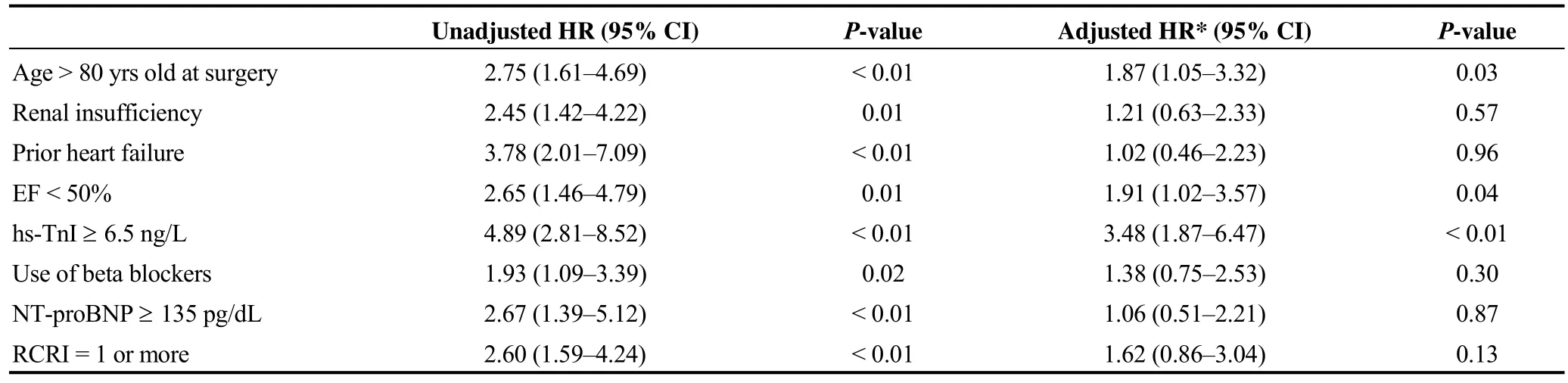
Table 3. Independent predictors of major adverse cardiovascular event development following hip fracture surgery in elderly patients.
A multivariate Cox regression analysis was performed to identify predictors of MACE development following HFS(Table 3). The independent predictors of MACE development were an age > 80 years old at the time of surgery (adjusted HR: 1.89; 95% CI: 1.08–3.31;P =0.03), EF < 50%(adjusted HR: 2.20; 95% CI: 1.20–4.03;P =0.01) and preoperative hs-TnI ≥ 6.5 ng/L (adjusted HR: 3.78; 95% CI:2.11–6.76;P <0.01).
4 Discussion
The results of this study can be summarized as follows.A considerable number of elderly hip fracture patients had MACE, even though they were in the RCRI = 0 subgroup.Preoperative elevated hs-TnI levels were associated with higher risk of MACE following HFS, and this relationship was driven by a higher incidence of postoperative AF and HF. An age > 80 years old at the time of surgery, left ventricular ejection fraction (LVEF) < 50% and preoperative hs-TnI > 6.5 ng/L were significant predictors of the development of MACE following HFS.
The current 2014 American College of Cardiology and American Heart Association (ACC/AHA) guidelines do not recommended routine postoperative screening of troponin levels in unselected patients who do not exhibit signs or symptoms suggestive of myocardial ischemia (Class III,level of evidence B), and the recent European Society of Cardiology guidelines do not recommended universal preoperative routine biomarker sampling for risk stratification or to prevent cardiac events (Class III, level of evidence C),although they do suggest that cardiac troponins may be considered in high-risk patients both before and at 48–72 hours after major surgery (Class IIb, level of evidence B).[2,13]However, the lack of recommendation for pre/postoperative troponin monitoring in these guidelines is based on a few studies with perioperative conventional troponin concentrations instead of preoperative high sensitive troponin, and they have mainly focused on perioperative mortality and MI when assessing cardiovascular risk.
A recent large cohort study compared patients who underwent non-cardiac surgery to a reference group (peak hs-TnT elevated level < 5 ng/L) and found that elevated perioperative hs-TnT, either with or without ischemic fea-tures, was significantly associated with an increased risk of 30-day mortality.[11]Another retrospective study of patients who underwent major orthopedic surgery found that a postoperative increase in serum troponin levels was associated with increased mortality at three years.[3]In the present study, unlike previous studies, all-cause death and MI were not associated with an increase in high sensitive troponin.However, the rate of MACE development was significantly higher in the group with preoperative hs-TnI ≥ 6.5 ng/L than in the group with hs-TnI < 6.5 ng/L, and this relationship was driven by a higher incidence of postoperative AF and HF. In elderly patients, hip fracture is commonly accompanied by impaired functional status and medical co-morbidities, including cardiovascular disease.[14–16]In this population with undergoing HFS, non-fatal perioperative cardiovascular events, such as atrial arrhythmia or pulmonary congestion, are not uncommon complications that can affect clinical outcomes.[17]With the introduction of new high-sensitive troponin assays, a growing amount of evidence indicates that troponins are also elevated in patients with various cardiovascular diseases, such as well-compensated heart failure, stable coronary heart disease or rhythm disturbance,which reflect minor myocardial injury.[18–20]In recent study of the general population, high cardiac troponin concentration within the normal range is associated with an increased cardiovascular disease risk.[21]A relationship between cardiac stress and cardiac troponin concentrations was demonstrated to involve the activation of the adrenergic and renin-angiotensin-aldosterone systems in previous study.[22]
The predictors for cardiovascular complication following HFS that were identified in this study are consistent with those reported in previous studies. Older age and low EF are established risk factors for perioperative cardiovascular complications in HFS.[5]Previous studies performed in patients with hip fracture consistently demonstrated that patients with elevated postoperative troponin levels are at a higher risk for subsequent cardiac events.[23,24]
In this study, the risk of MACE was higher in the RCRI= 1 or more subgroup than in the RCRI = 0 subgroup.However, even among the elderly patients in the RCRI = 0 group who underwent HFS, a considerable number of MACE occurred. In the RCRI = 0 subgroup, the risk of MACE was higher in patients with preoperative hs-TnI ≥6.5 ng/L than in those with postoperative hs-TnI < 6.5 ng/L.This minimal elevation in preoperative hs-TnI was associated with the development of MACE. Hence, in addition to its usefulness in conventional perioperative risk assessments,hs-TnI may be helpful for further risk refinement in elderly patients who undergo HFS.
There are some limitations to the present study. First, the study design was nonrandomized, retrospective, and observational, and the presence of confounding factors may have significantly affected the results. Although we performed a multivariate analysis to adjust for potential confounding factors, we were not able to correct for unmeasured variables. In particular, because of limitations associated with the patient database, we could not obtain information on the fragility of individual patients (e.g., no information on the presence of chronic pulmonary disease or cancer was available). Second, in preoperative evaluations, whether to test for biomarkers was left to the discretion of the cardiology consultation physician. Hence, not all patients in the registry were evaluated to determine their hs-TnI levels, and the selection bias associated with this factor is difficult to overcome. However, the findings of this study may be reflecting those observed in real practice, given the current guideline recommendations for preoperative assessment using cardiac troponin. Third, a relatively small number of variables were included in the multivariate Cox proportional hazard model,and this may have reduced the detection power or influenced the validity of the interactions.
In conclusion, a considerable number of elderly hip fracture patients in this study had MACE, even if they were in the RCRI = 0 subgroup. A preoperatively elevated hs-TnI level was associated with a higher risk of MACE following HFS, and this interaction was driven by a higher incidence of postoperative atrial fibrillation and heart failure. Performing a preoperative assessment using hs-TnI may be helpful for further risk refinement in elderly patients who undergo HFS.
References
1 Smilowitz NR, Berger JS. Perioperative management to reduce cardiovascular events.Circulation2016; 133: 1125–1130.
2 Fleisher LA, Fleischmann KE, Auerbach AD,et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.Circulation2014; 130: e278–333.
3 Oberweis BS, Smilowitz NR, Nukala S,et al. Relation of perioperative elevation of troponin to long-term mortality after orthopedic surgery.Am J Cardiol2015; 115: 1643–1648.
4 Chiang CH, Liu CJ, Chen PJ,et al. Hip fracture and risk of acute myocardial infarction: a nationwide study.J Bone Miner Res2013; 28: 404–411.
5 Sathiyakumar V, Avilucea FR, Whiting PS,et al. Risk factors for adverse cardiac events in hip fracture patients: an analysis of NSQIP data.Int Orthop2016; 40: 439–445.
6 Giannitsis E, Katus HA. Cardiac troponin level elevations not related to acute coronary syndromes.Nat Rev Cardiol2013;10: 623–634.
7 Ahmed AN, Blonde K, Hackam D,et al. Prognostic significance of elevated troponin in non-cardiac hospitalized patients:a systematic review and meta-analysis.Ann Med2014; 46:653–663.
8 Michos ED, Wilson LM, Yeh HC,et al. Prognostic value of cardiac troponin in patients with chronic kidney disease without suspected acute coronary syndrome: a systematic review and meta-analysis.Ann Intern Med2014; 161: 491–501.
9 Lipinski MJ, Baker NC, Escarcega RO,et al. Comparison of conventional and high-sensitivity troponin in patients with chest pain: a collaborative meta-analysis.Am Heart J2015;169: 6–16.
10 van der Linden N, Klinkenberg LJ, Bekers O,et al. Prognostic value of basal high-sensitive cardiac troponin levels on mortality in the general population: a meta-analysis.Medicine(Baltimore) 2016; 95: e5703.
11 Devereaux PJ, Biccard BM, Sigamani A,et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery.JAMA2017; 317: 1642–1651.
12 Lee TH, Marcantonio ER, Mangione CM,et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery.Circulation1999;100: 1043–1049.
13 Kristensen SD, Knuuti J, Saraste A,et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA).Eur Heart J2014; 35: 2383–2431.
14 Sennerby U, Farahmand B, Ahlbom A,et al. Cardiovascular diseases and future risk of hip fracture in women.Osteoporos Int2007; 18: 1355–1362.
15 Bentler SE, Liu L, Obrizan M,et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality.Am J Epidemiol2009; 170: 1290–1299.
16 Sennerby U, Melhus H, Gedeborg R,et al. Cardiovascular diseases and risk of hip fracture.JAMA2009; 302: 1666–1673.
17 Gupta BP, Steckelberg RC, Gullerud RE,et al. Incidence and 1-year outcomes of perioperative atrial arrhythmia in elderly adults after hip fracture surgery.J Am Geriatr Soc2015; 63:2269–2274.
18 Caselli C, Prontera C, Liga R,et al. Effect of coronary atherosclerosis and myocardial ischemia on plasma levels of highsensitivity troponin T and NT-proBNP in patients with stable angina.Arterioscler Thromb Vasc Biol2016; 36: 757–764.
19 McCarthy CP, Yousuf O, Alonso A,et al. High-sensitivity troponin as a biomarker in heart rhythm disease.Am J Cardiol2017; 119: 1407–1413.
20 Seliger SL, Hong SN, Christenson RH, et al. High-sensitive cardiac troponin T as an early biochemical signature for clinical and subclinical heart failure: MESA (Multi-Ethnic Study of Atherosclerosis).Circulation2017; 135: 1494–1505.
21 Willeit P, Welsh P, Evans JDW,et al. High-sensitivity cardiac troponin concentration and risk of first-ever cardiovascular outcomes in 154,052 participants.J Am Coll Cardiol2017; 70:558–568.
22 Pastormerlo LE, Agazio A, Benelli E,et al. Usefulness of high-sensitive troponin elevation after effort stress to unveil vulnerable myocardium in patients with heart failure.Am J Cardiol2015; 116: 567–572.
23 Ausset S, Auroy Y, Lambert E,et al. Cardiac troponin I release after hip surgery correlates with poor long-term cardiac outcome.Eur J Anaesthesiol2008; 25: 158–164.
24 Katsanos S, Mavrogenis AF, Kafkas N,et al. Cardiac biomarkers predict 1-year mortality in elderly patients undergoing hip fracture surgery.Orthopedics2017; 40: e417–e424.
杂志排行
Journal of Geriatric Cardiology的其它文章
- The contribution of gender and age on early and late mortality following ST-segment elevation myocardial infarction: results from the Korean Acute Myocardial Infarction National Registry with Registries
- The subcutaneous implantable cardioverter defibrillator––review of the recent data
- Should atrial fibrillation patients with hypertension as an additional risk factor of the CHA2DS2-VASc score receive oral anticoagulation?
- Successful conservative management of Class III iatrogenic aortic dissection
- Anterior myocardial pseudoinfarction in a patient with diabetic ketoacidosis
- Simultaneous multiple coronary arteries thrombosis in patients with STEMI
