The contribution of gender and age on early and late mortality following ST-segment elevation myocardial infarction: results from the Korean Acute Myocardial Infarction National Registry with Registries
2018-05-23AeYoungHerEunSeokShinYongHoonKimScotGargMyungHoJeong
Ae-Young Her, Eun-Seok Shin, Yong Hoon Kim, Scot Garg, Myung Ho Jeong
1Division of Cardiology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, South Korea
2Department of Cardiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Republic of Korea
3East Lancashire Hospitals NHS Trust, Blackburn, Lancashire, UK
4The Heart Center of Chonnam National University Hospital, Gwangju, Republic of Korea
1 Introduction
Although the mortality of cardiovascular disease (CVD)has declined substantially due to advances in its management and treatment, acute coronary syndrome (ACS) is currently a leading cause of mortality in the Asia-Pacific region, accounting for around half of the global burden.[1]In industrialized Western countries, improved adoption of evidence-based recommendations over the last decade strongly correlate with the reduction in both in-hospital and long-term mortality after ACS.[2,3]In contrast the 30-day mortality after hospital admission for acute myocardial infarction (AMI) in South Korea is still high compared to average according to the Organization for Economic Cooperation and Development (OECD).[4]Even between Asia-Pacific countries, registry data show strong regional heterogeneity in the patterns of clinical practice, and in short- and long-term clinical outcomes.[5,6]
Of note, previous investigations have focused on variations in the treatment and subsequent outcomes of AMI that are related to international and gender differences.[7–12]Several studies, including some from the U.S. and Europe, have suggested that gender differences in mortality following AMI vary by age, with a particularly adverse prognosis in younger women, which persists after adjustment for risk factors.[13–15]Similarly, in China, gender differences in early mortality were age dependent, with the greatest differences seen in younger females (i.e. < 70 years of age).[16]The main reasons for these findings among younger women include the poorer implementation of evidence-based medication and delays to timely reperfusion therapy.
In view of these findings it is of vital importance to examine whether these gender and age differences in outcome exist in patients with ST-segment elevation myocardial infarction (STEMI) in South Korea. Although previous studies using Korean data have already reported higher rates of mortality in women,[17,18]it is less clear whether these gender differences in prognosis after STEMI are age dependent.We have already published the results on the poor short- and long-term clinical outcomes of younger women with AMI but have not stratified these outcomes according to age,whilst also including patients with both STEMI and non-STEMI, resulting a heterogeneous population with ACS.[19]
The objective of this study is to examine the interaction of gender and age on in-hospital, early (< 30 days after admission) and late (12 months) mortality in patients with STEMI who were enrolled in the nationwide registry of the Korea Working Group of Myocardial Infarction.
2 Methods
2.1 Data source and study population
The Korean Acute Myocardial Infarction Registry(KAMIR), was a nationwide registry conducted from November 2005 to January 2008, whilst its successor, the Korean Myocardial Infarction (KorMI) registry, was conducted from January 2008 to July 2011. These were prospective multicentre online Korean registries reflecting current practice in the management and clinical outcomes of Asian patients diagnosed with AMI and supported by the Korean Working Group of Acute Myocardial Infarction. The protocols and details of the registries have been published previously.[20,21]Data were collected at each site by an experienced study coordinator using a standardized case report form and protocol, and then merged with the intention of improving the statistical power. Figure 1 presents the scheme of this study. The data of 30,001 among 31,149 AMI patients in the database were extracted for this study.Invalid or incomplete data and non-STEMI were excluded,leaving a final cohort of 17,021 patients for use in the analysis. Patients were divided into two groups according to their gender. The study protocol was reviewed and approved by the institutional review board at each participating center.
2.2 Definitions and clinical end points
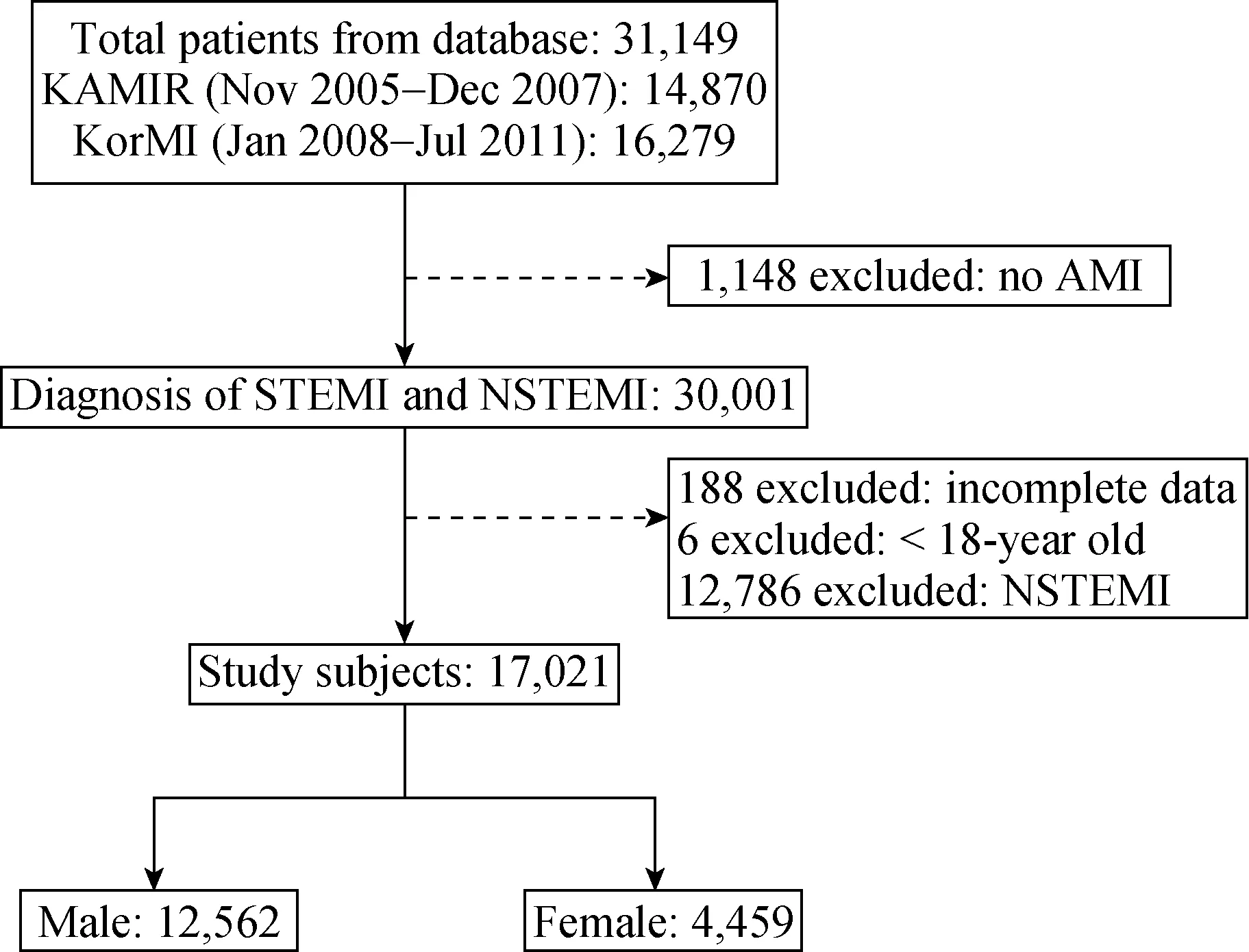
Figure 1. The scheme of this study. The data of 30,001 among 31,149 patients with AMI in the database were extracted for this study. Invalid or incomplete data and non-STEMI were excluded,leaving a final cohort of 17,021 patients for use in the analysis.AMI: acute myocardial infarction; KAMIR: the Korean Acute Myocardial Infarction Registry; KorMI: the Korean Myocardial Infarction; NSTEMI: Non ST-segment elevation myocardial infarction; STEMI: ST-segment elevation myocardial infarction.
AMI was defined on the basis of appropriate clinical signs or symptoms, increased cardiac biomarkers, and 12-lead ECG findings. Patients were diagnosed with STEMI if they had chest pain longer than 30 minutes and ECG changes with ST elevation greater than 2 mm in at least two precordial leads or greater than 1 mm in the limb leads, or new left bundle branch block, and abnormal troponin levels or creatine kinase-MB (CK-MB) at least twice the upper limit of normal.[22]Major bleeding was defined as an absolute hematocrit drop of ≥ 15%, any intracranial bleeding,bleeding events associated with causing death, the need for surgery or transfusion, or any clinically relevant bleeding as judged by an investigator. All-cause deaths were considered cardiac unless a non-cardiac cause could be clearly identified. Recurrent myocardial infarction (MI) was defined as recurrent symptoms with new ECG changes compatible with MI or cardiac markers at least twice the upper limit of the normal. Repeat revascularization included target lesion revascularization (TLR) and target vessel revascularization(TVR). TLR was defined as a repeat intervention in the stent, or within 5 mm proximal or distal to the stent. TVR was defined as a repeat intervention in the same vessel, > 5 mm from the stent. Major adverse cardiac events (MACEs)were defined as a composite of death, recurrent MI, and repeat revascularization. The primary end point was the composite of MACEs during hospitalization as well as early(before 30 days after admission) and late (12 months) clinical follow-up.
2.3 Statistical analysis
All statistical analyses were done using SPSS version 19.0 (SPSS, Inc., Chicago, Illinois, USA). Based on the distribution of early and late mortality among women and men, we classified the patients into four pre-specified age groups (< 60, 60–69, 70–79, and ≥ 80 years). For discrete variables, differences were presented as counts and percentages, and were analyzed using ax2test (or Fisher’s exact test) between women and men in each age group. Crude odds ratios (ORs) with 95% confidence intervals (CIs) for women versus men were reported.
We used multivariable logistic regression models to calculate adjusted OR and 95% CI for in-hospital, early and late mortality in the overall population as well as within each age group, and to determine whether there was a significant interaction between gender and age with respect to in-hospital, early and late mortality. Final adjustment in the logistic model was performed with the following variables:age, gender, body mass index (BMI), hypertension, diabetes mellitus, dyslipidemia, current smoking, Killip class ≥ 3,symptom to balloon time and major bleeding. All comparisons were 2-tailed, with aPvalue < 0.05 considered statistically significant.
3 Results
3.1 Baseline characteristics
Baseline characteristics of patients stratified by gender and age are reported in Table 1. Younger women (< 60 years) were more likely to have lower BMI (OR: 1.29; 95%CI: 1.07–1.55) compared with men. Younger women (< 60 years) had a more frequent history of hypertension (OR:2.43; 95% CI: 2.04–2.90) and diabetes mellitus (OR: 1.59;95% CI: 1.30–1.93), but fewer of them were current smokers (OR: 0.09; 95% CI: 0.07–0.11) or had a previous history of MI (OR: 0.41; 95% CI: 0.24–0.68) compared with men.Women over the age of 60 years were also more likely to have hypertension, diabetes mellitus or dyslipidemia but less likely to smoke and have a previous history of MI. Although signs of heart failure at admission (Killip class ≥ 3)were found to be more severe in women of all age groups,left ventricular ejection fraction was similar between women and men by age group.
There was no significant difference in door-to-balloon time between genders by age group, however younger women (< 60 years) were more likely to have symptoms lasting > 12 hours before hospital admission (longer symptom to balloon time) than their male peers. Also, women aged 70–79 years were more likely to have symptoms lasting > 24 hours before hospital admission compared with men. CK-MB, troponin-I, and creatinine levels were higher in men of all age groups. Women aged 60–69 years had higher high-sensitivity C-reactive protein levels compared with men. Older women (≥ 60 years) had higher low-density lipoprotein cholesterol levels than their male peers at presentation.
The discharge medication also varied by gender and age.Younger women (< 60 years) were less likely to receive clopidogrel (OR: 0.51; 95% CI: 0.37–0.72) or an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker (ARB) (OR: 0.76; 95% CI: 0.61–0.95) at discharge compared with similarly aged men. Older women(aged 60–69 and 70–79 years) were also less likely to receive clopidogrel at discharge.
3.2 Angiographic characteristics
Angiographic findings of patients are presented in Table 2. Younger women (< 60 years) were more likely to have left main disease for culprit lesion (OR: 2.18; 95% CI:1.23–3.89), but older women (aged 60–69 years and 70–79 years) were less likely to have left main disease for culprit lesion compared with men. With respect to reperfusion strategies, younger women (< 60 years) were less likely to receive thrombolysis (OR: 0.73; 95% CI: 0.53–1.00) or percutaneous coronary intervention (PCI) (OR: 0.64; 95%CI: 0.49–0.84) compared with similarly aged men. Although women aged 60–69 years were more likely to have poor Thrombolysis in Myocardial Infarction (TIMI) flow(OR: 1.27; 95% CI: 1.08–1.50) at presentation, TIMI flow after PCI showed no significant differences between genders by age group. Women of all age groups had smaller stent diameters, but in stent type, length, and number, they showed no significant differences compared with their male peers.
Finally, younger women (< 60 years) had higher rates of major bleeding than men (OR: 7.04; 95% CI: 2.55–19.43)and women aged 70–79 years were more likely to have cardiogenic shock (OR: 1.64; 95% CI: 1.22–2.20).
3.3 Unadjusted early and late mortality
As shown in Table 3, overall in-hospital mortality rate was higher in women (12.2%vs. 5.5% in men,P< 0.001).In-hospital mortality after STEMI increased with age for both genders. In younger women (< 60 years), in-hospital mortality (5.8%vs. 2.5%,P< 0.001; unadjusted OR: 2.41,95% CI: 1.59–3.66), cardiac death (3.7%vs. 2.0%,P=0.011; unadjusted OR: 1.91, 95% CI: 1.15–3.16), and noncardiac death (2.1%vs.0.5%,P= 0.001; unadjusted OR:4.23, 95% CI: 2.04–8.75) were significantly higher compared with men (Table 3 and Figure 2A). The 30-day rates of MACE (6.6%vs. 3.2%,P< 0.001; unadjusted OR: 2.15,95% CI: 1.46–3.17) and all-cause mortality (6.2%vs. 2.6%,P< 0.001; unadjusted OR: 2.50, 95% CI: 1.67–3.75) were also higher in younger women (< 60 years) compared withtheir male peers (Table 3 and Figure 2B). In addition,12-month rates of MACE (8.9%vs. 5.9%,P= 0.009; unadjusted OR: 1.55, 95% CI: 1.11–2.16), all-cause mortality(7.0%vs. 3.1%,P< 0.001; unadjusted OR: 2.36, 95% CI:1.61–3.45) and cardiac death (4.6%vs. 2.2%,P< 0.001;unadjusted OR: 2.10, 95% CI: 1.32–3.34) were higher in younger women (< 60 years) compared with men (Table 3,Figure 2C and 2D). When mortality rates were analyzed by
age, a gender-age interaction was observed (in-hospital mortality,P< 0.001; 30-day mortality,P< 0.001; 12-month mortality,P< 0.001).

Table 1. Unadjusted OR for characteristics of patients comparing women with men according to age.
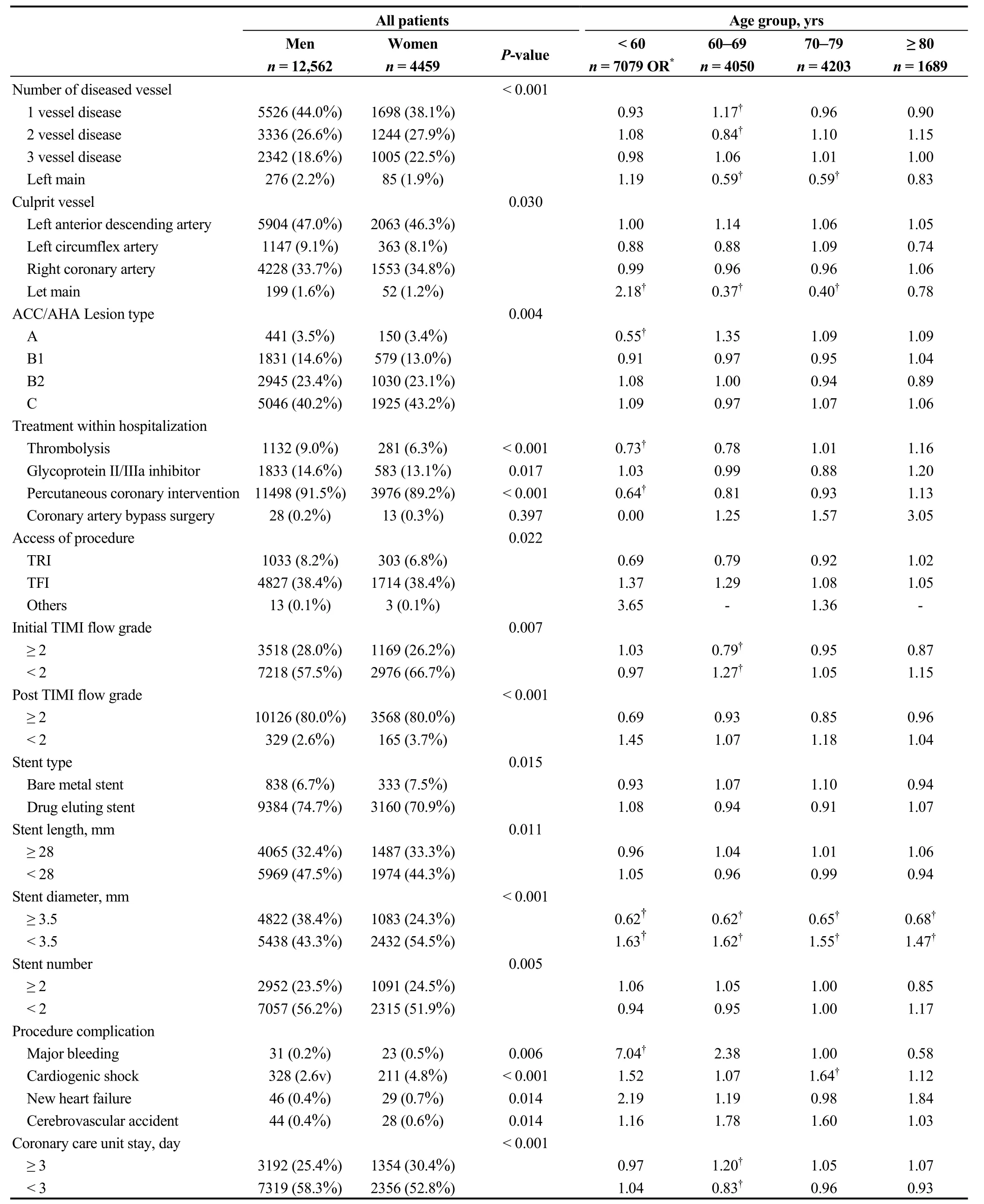
Table 2. Unadjusted OR for angiographic and procedural characteristics comparing women with men according to age.
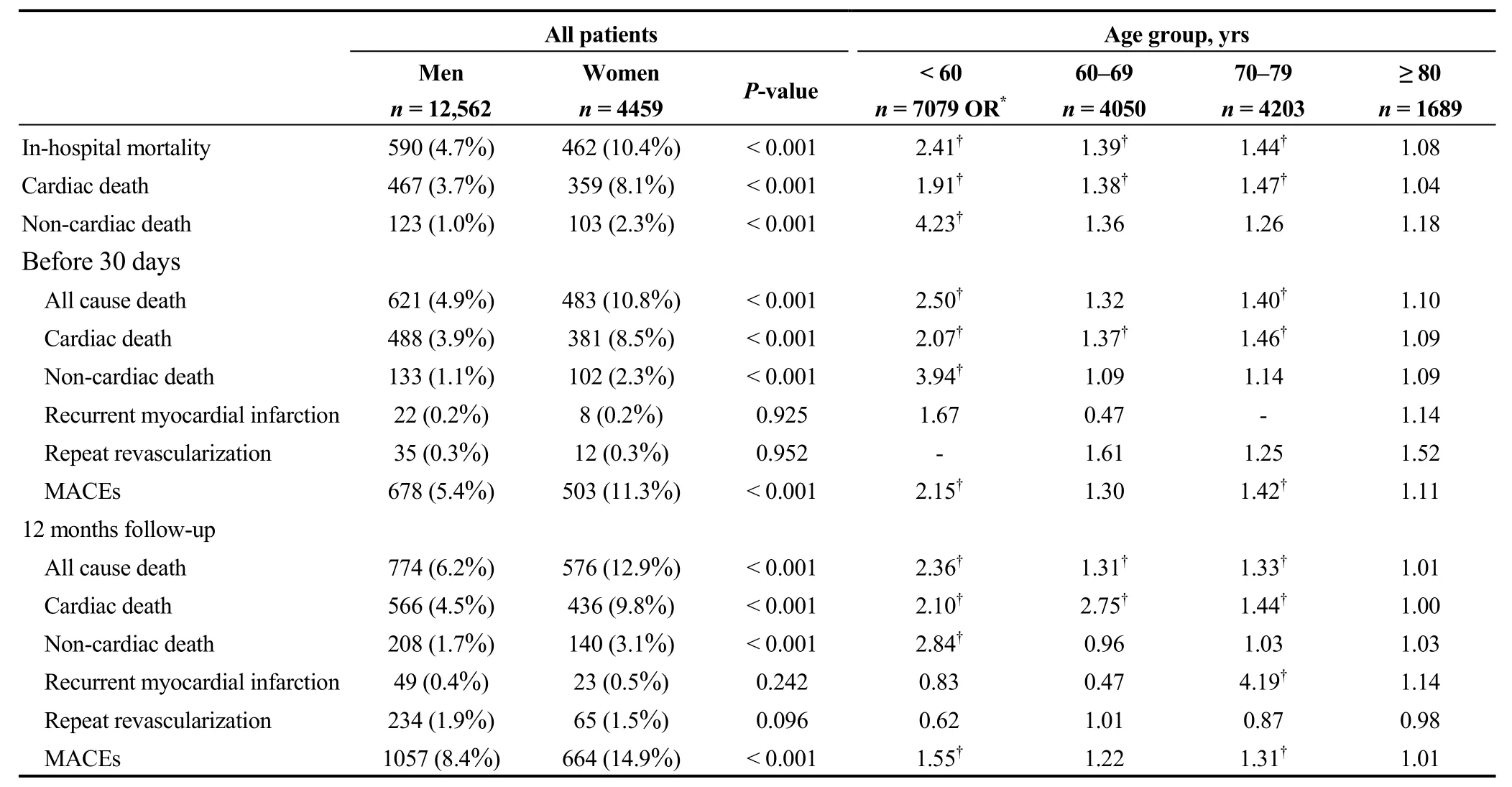
Table 3. MACEs between men and women.

Figure 2. Unadjusted risk of in-hospital (A) 30-day, (B) 12-month mortality, (C) and 12-month cardiac death rate (D) comparing women with men according to age. The interaction between gender and age was statistically significant (all P < 0.001).
Although a higher risk of death was observed among women ≥ 80 years at all time points, no significant between gender-differences were seen in patients ≥ 80 years. Similarly, there were no significant differences between gender and age in the rates of recurrent MI and repeat revascularization.
3.4 Multivariable-adjusted early and late mortality
In the multivariable model, adjusting for age, gender,BMI, hypertension, diabetes mellitus, dyslipidemia, current smoking, Killip class ≥ 3, symptom to balloon time, and major bleeding, there were no statistically significant interactions between gender and age for mortality (Figure 3A–3C). Similarly, 12-month cardiac death was not significantly different between gender and age (Figure 3D).
4 Discussion
The present study showed for the first time that there was a significant gender-age interaction with early and late mortality in Korean patients with STEMI. In younger women (<60 years), in-hospital, early and late mortality rates were significantly higher compared with men. No significant differences in early and late mortality were observed between gender in the very old age group (≥ 80 years). The poorer prognosis in younger women (< 60 years) may be explained by adverse patient characteristics, higher Killip class ≥ 3, longer symptom to balloon time, and more frequent major bleeding.

Figure 3. Unadjusted and adjusted risk of mortality. (A): Unadjusted and adjusted risk of in-hospital mortality rate following STEMI comparing women with men by age. In the unadjusted data, the interaction between gender and age was statistically significant (P < 0.001).After adjustment, the interaction between gender and age was not statistically significant (P = 0.418). (B): Unadjusted and adjusted risk of 30-day mortality rate following STEMI comparing women with men by age. In the unadjusted data, the interaction between gender and age was statistically significant (P < 0.001). After adjustment, the interaction between gender and age was not statistically significant (P = 0.584).(C): Unadjusted and adjusted risk of 12-month mortality rate following STEMI comparing women with men by age. In the unadjusted data,the interaction between gender and age was statistically significant (P < 0.001). After adjustment, the interaction between gender and age was not statistically significant (P = 0.446). (D): Unadjusted and adjusted risk of 12-month cardiac death rate following STEMI comparing women with men by age. In the unadjusted data, the interaction between gender and age was statistically significant (P < 0.001). After adjustment, the interaction between gender and age was not statistically significant (P = 0.418). OR: odds ratios; STEMI: ST-segment elevation myocardial infarction.
Despite improvement in short- and long-term survival following AMI over recent decades, the risk of a subsequent MI or death remains elevated in many countries.[2,3,5,6]In particular, in-hospital mortality after AMI is still higher in South Korea in comparison to other countries (DOI: 10.1787/health_glance-2015-en).[23,24]Although several studies have shown no differences, many studies have shown that women have a higher risk of early and late mortality after AMI.[8–10,25]In addition, these studies have identified an agegender interaction, whereby younger women were at particularly high risk of mortality after AMI even after adjustment for other prognostic factors.[14,15]However, some differences do exist between countries; for example, there was a higher risk of in-hospital mortality in women aged < 50 years in the U.S., while in China the increased risk of in-hospital mortality was observed in patients up to 70 years of age.[13,16]
In our Korean data, women aged < 60 years showed significantly higher in-hospital, early and late mortality compared with similarly aged men. However, after adjustment for cardiovascular risk factors, preadmission co-morbidities,Killip class ≥ 3, symptom to balloon time and major bleeding, the interactions between gender and age for mortality were no longer statistically significant. In other words, mortality rates were no longer related to gender in any age groups. Also, in contrast to Chinese data, the present study showed several potential explanations for the higher risk of mortality in younger women (< 60 years). Our study showed that younger women (< 60 years) with STEMI had a great number of risk factors and were more critically ill when compared with younger men, which in part explained their higher mortality. Similarly in the INTERHEART study,such risk factors as diabetes and hypertension were more strongly associated with the development of MI in women than in men, as well as in younger (< 60 years) compared with older (≥ 60 years) women.[26]As such, several strategies, including prevention, the early identification and aggressive management of risk factors before incidence, may be a target for future efforts to reduce the excess risk of mortality following STEMI among younger women, especially in Korea burdened with rapidly increasing cardiovascular risk factors.[27,28]Other possible explanations for the poor prognosis observed among younger women include a lack of awareness of symptoms, under-recognition at presentation, lower application of evidence-based medication and less timely reperfusion therapy. Previously, gender disparities in reperfusion therapy, short-, and long-term mortality for patients with STEMI have been well documented.[29,30]Celik et al showed that woman was an important risk factor for no-reflow in STEMI patients undergoing primary PCI.[30]Consistently in our study, women aged 60 years and younger had a longer time from symptom onset to balloon time compared with other age groups, and there was an association between symptom onset to balloon time and rate of revascularization (PCI and coronary artery bypass graft) (P= 0.013). This may explain the less frequent use of early reperfusion and ultimately the higher risk of mortality in this age group. Delayed hospital presentation in younger women may be due to atypical symptom onset of AMI,[31]which can also result in delayed diagnosis even after presentation to hospital.[32]However, our Korean data showed that although younger women (< 60 years) had longer symptom onset to balloon time compared with similarly aged men, there was no significant difference in door to balloon time between women and men in this age group.These data indicates that Korean hospitals have been accurately diagnosing AMI compared with other countries.[23,28]Therefore, more aggressive education and promotion may be necessary to overcome delayed hospital presentation. In addition, less use of evidence-based treatment on admission may contribute to the higher mortality in younger women.Of note, studies in the U.S. have found that gender difference in evidence-based treatment did not adequately account for the observed disparity in mortality.[33,34]Lessening the aforementioned disparities in disease awareness,[35]prompt diagnosis and the timely administration of evidence-based treatment could lead to meaningful improvement in the outcomes of younger women with AMI and should be the target of future interventions.
Of note, we observed a higher incidence of major bleeding in younger women (< 60 years), despite the absence of any significant differences in catheterization access site between gender and age. Although the mechanism for this association is incompletely understood, the adverse impact of bleeding has been shown in numerous studies,[36–38]together with a higher incidence of short-term bleeding in women even after adjustment for baseline differences. Acute bleeding may be life-threatening depending on its location and severe blood loss can contribute to persisting shock. Bleeding also leads to anemia and requires the transfusion of blood products, which promote inflammation.[39]Moreover,bleeding may result in the cessation of antiplatelet and anticoagulant therapy, which increases the risk of recurrent ischemic events such as stent thrombosis and recurrent MI.[40]
Finally, investigation into other factors such as socioeconomic, cultural, educational and psychological factors may have important implication on how we educate patients as well as physicians, and how we assess the risk and evaluate treatment strategies for younger women with AMI.
The possible limitations of this study are as follows. First,we could not identify any causality for the associations mentioned earlier. Second, as this study was based on registry data, which had been collected voluntarily at each participating center, we lacked data on some important clinical variables, such as bleeding event, coronary angiographic characteristics and other potential unmeasured factors, which may have influenced management. However, this study had the advantages of a large sample size, a multicenter design,and prospective data indigenous to Korea. Finally, we had no information on prehospital death and the long-term health outcomes of patients with STEMI.
In conclusion, we showed that in-hospital, early and late mortality rates were significantly higher in younger women(< 60 years) compared with similarly aged men. In contrast to this, no significant differences in early and late mortality were observed between sexes in a very old age groups (≥ 80 years). The poorer prognosis in younger women (< 60 years)can be explained by adverse patient characteristics, higher Killip class ≥ 3, longer symptom to balloon time and frequent major bleeding. Therefore, more precise and aggressive preventive strategies focused on risk factor reduction,education and more intensive management for younger women should be performed. Further research is required to enhance the understanding and development of intervention to improve the outcomes of younger women, especially under high risk conditions.
References
1 Ohira T, Iso H. Cardiovascular disease epidemiology in Asia:an overview.Circ J2013; 77: 1646–1652.
2 Granger CB, Steg PG, Peterson E,et al. Medication performance measures and mortality following acute coronary syndromes.Am J Med2005; 118: 858–865.
3 Boden H, van der Hoeven BL, Karalis I,et al. Management of acute coronary syndrome: achievements and goals still to pursue. Novel developments in diagnosis and treatment.J Intern Med2012; 271: 521–536.
4 Lafortune G, Devaux M, Mueller M,et al. Health at a Glance,2015: OECD Indicators; OECD Publishing, Paris, France,2015;1–216.
5 Prabhakaran D, Yusuf S, Mehta S,et al. Two-year outcomes in patients admitted with non-ST elevation acute coronary syndrome: results of the OASIS registry 1 and 2.Indian Heart J2005; 57: 217–225.
6 Koh AS, Khin LW, Choi LM,et al. Percutaneous coronary intervention in Asians--are there differences in clinical outcome?BMC Cardiovasc Disord2011; 11: 22.
7 Andre R, Bongard V, Elosua R,et al. International differences in acute coronary syndrome patients' baseline characteristics,clinical management and outcomes in Western Europe: the EURHOBOP study.Heart2014; 100: 1201–1207.
8 Bucholz EM, Butala NM, Rathore SS,et al. Sex differences in long-term mortality after myocardial infarction: a systematic review.Circulation2014; 130: 757–767.
9 Chung SC, Gedeborg R, Nicholas O,et al. Acute myocardial infarction: a comparison of short-term survival in national outcome registries in Sweden and the UK.Lancet2014; 383:1305–1312.
10 Hochman JS, Tamis JE, Thompson TD,et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators.N Engl J Med1999; 341: 226–232.
11 Mehta LS, Beckie TM, DeVon HA,et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association.Circulation2016; 133: 916–947.
12 Milcent C, Dormont B, Durand-Zaleski I,et al. Gender differences in hospital mortality and use of percutaneous coronary intervention in acute myocardial infarction: microsimulation analysis of the 1999 nationwide French hospitals database.Circulation2007; 115: 833–839.
13 Champney KP, Frederick PD, Bueno H,et al. The joint contribution of sex, age and type of myocardial infarction on hospital mortality following acute myocardial infarction.Heart2009; 95: 895–899.
14 Otten AM, Maas AH, Ottervanger JP,et al. Is the difference in outcome between men and women treated by primary percutaneous coronary intervention age dependent? Gender difference in STEMI stratified on age.Eur Heart J Acute Cardiovasc Care2013; 2: 334–341.
15 Simon T, Mary-Krause M, Cambou JP,et al. Impact of age and gender on in-hospital and late mortality after acute myocardial infarction: increased early risk in younger women: results from the French nation-wide USIC registries.Eur Heart J2006; 27: 1282–1288.
16 Zheng X, Dreyer RP, Hu S,et al. Age-specific gender differences in early mortality following ST-segment elevation myocardial infarction in China.Heart2015; 101: 349–355.
17 Park JS, Kim YJ, Shin DG,et al. Gender differences in clinical features and in-hospital outcomes in ST-segment elevation acute myocardial infarction: from the Korean Acute Myocardial Infarction Registry (KAMIR) study.Clin Cardiol2010;33: E1–E6.
18 Kang SH, Suh JW, Yoon CH,et al. Sex differences in management and mortality of patients with ST-elevation myocardial infarction (from the Korean Acute Myocardial Infarction National Registry).Am J Cardiol2012; 109: 787–793.
19 Cho KI, Shin ES, Ann SH,et al. Gender differences in risk factors and clinical outcomes in young patients with acute myocardial infarction.J Epidemiol Community Health2016;70: 1057–1064.
20 Chen KY, Rha SW, Li YJ,et al. Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention.Circulation2009; 119: 3207–3214.
21 Kim HK, Jeong MH, Lee SH,et al. The scientific achievements of the decades in Korean Acute Myocardial Infarction Registry.Korean J Intern Med2014; 29: 703–712.
22 O'Gara PT, Kushner FG, Ascheim DD,et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol2013; 61: e78–e140.
23 Lee SW, Kim HC, Lee HS,et al. Thirty-year trends in mortality from cardiovascular diseases in Korea.Korean Circ J2015;45: 202–209.
24 Kim JH, Chae SC, Oh DJ,et al. Multicenter cohort study of acute myocardial infarction in Korea: interim analysis of the Korea Acute Myocardial Infarction Registry-National Institutes of Health Registry.Circ J2016; 80: 1427–1436.
25 Koek HL, de Bruin A, Gast F,et al. Short- and long-term prognosis after acute myocardial infarction in men versus women.Am J Cardiol2006; 98: 993–999.
26 Anand SS, Islam S, Rosengren A,et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study.Eur Heart J2008; 29: 932–940.
27 Ueshima H, Sekikawa A, Miura K,et al. Cardiovascular disease and risk factors in Asia: a selected review.Circulation2008; 118: 2702–2709.
28 Lee KH, Jeong MH, Ahn Y,et al. New horizons of acute myocardial infarction: from the Korea Acute Myocardial Infarction Registry.J Korean Med Sci2013; 28: 173–180.
29 Celik T, Balta S, Ozturk C,et al. Survival of the young patients with acute ST segment elevation myocardial infarction treated with primary percutaneous coronary intervention:Does gender matters?Int J Cardiol2016; 210: 54–55.
30 Celik T, Balta S, Ozturk C,et al.Predictors of no-reflow phenomenon in young patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention.Angiology2016; 67: 683–689.
31 Canto JG, Goldberg RJ, Hand MM,et al. Symptom presentation of women with acute coronary syndromes: myth vs reality.Arch Intern Med2007; 167: 2405–2413.
32 Pope JH, Aufderheide TP, Ruthazer R,et al. Missed diagnoses of acute cardiac ischemia in the emergency department.N Engl J Med2000; 342: 1163–1170.
33 Vaccarino V, Parsons L, Every NR,et al. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants.N E ngl J Med1999; 341: 217–225.
34 Ani C, Pan D, Martins D,et al. Age- and sex-specific in-hospital mortality after myocardial infarction in routine clinical practice.Cardiol Res Pract2010; 2010: 752–765.
35 Canto JG, Rogers WJ, Goldberg RJ,et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality.JAMA2012; 307: 813–822.
36 Mehta RH, Stebbins AS, Lopes RD,et a l. Comparison of incidence of bleeding and mortality of men versus women with ST-elevation myocardial infarction treated with fibrinolysis.Am J Cardiol2012; 109: 320–326.
37 Manoukian SV. Predictors and impact of bleeding complications in percutaneous coronary intervention, acute coronary syndromes, and ST-segment elevation myocardial infarction.Am J Cardiol2009; 104: 9c–15c.
38 Oldgren J, Wernroth L, Stenestrand U,et a l. Fibrinolytic therapy and bleeding complications: risk predictors from RIKS-HIA.Heart2010; 96: 1451–1457.
39 Willis P, Voeltz MD. Anemia, hemorrhage, and transfusion in percutaneous coronary intervention, acute coronary syndromes, and ST-segment elevation myocardial infarction.Am J Cardiol2009; 104: 34c–38c.
40 Chan MY, Sun JL, Wang TY,et al. Patterns of discharge antiplatelet therapy and late outcomes among 8,582 patients with bleeding during acute coronary syndrome: a pooled analysis from PURSUIT, PARAGON-A, PARAGON-B, and SYNERGY.Am Heart J2010; 160: 1056–1064.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Association between preoperative high sensitive troponin I levels and cardiovascular events after hip fracture surgery in the elderly
- The subcutaneous implantable cardioverter defibrillator––review of the recent data
- Should atrial fibrillation patients with hypertension as an additional risk factor of the CHA2DS2-VASc score receive oral anticoagulation?
- Successful conservative management of Class III iatrogenic aortic dissection
- Anterior myocardial pseudoinfarction in a patient with diabetic ketoacidosis
- Simultaneous multiple coronary arteries thrombosis in patients with STEMI
