Fabry disease combined with acute interstitial nephritis:one case and literature review
2018-04-23JinshanSunChaoyingChenYubingWen
Jinshan Sun,Chaoying Chen ,Yubing Wen
1Children's Hospital Affiliated to Capital Institute Of Pediatrics,Department of Nephrology,Beijing 100020,China. 2Peking Union Medical College Hospital,Chinese Academy of Medical Sciences,Department of Nephrology,Beijing 100020,China.
Introduction
Fabry's disease is a rare x-linked inherited lysosomal storage disorder,the disease is caused by the Xq21.33-xq22 alpha galactose glucoside enzyme encoded on A(alpha galactosidase.A,alpha GalA)gene mutations cause alpha GalA activity decline,the alpha galactose residues from neutral sugar lipid molecules over from blocked the scabbard, which caused the melamine hexose amide (globotriao sylceramide, Gb3) in including skin,kidneys,heart,central nervous tissue of abnormal deposition, As a result, multiple organ function injuries were caused,among which kidney injury was initially manifested as renal concentration dysfunction,followed by a large amount of proteinuria and further development of renal failure. Acute interstitial nephritis (ATIN) is a group of clinical pathological syndromes caused by a variety of etiologies,with rapid onset,clinical manifestations of Acute renal insufficiency or failure, and pediatric clinical is not common.According to literature review,there were no reports of Fabry disease combined with ATIN. A case of Fabry disease diagnosed in nephrology department of the capital institute of pediatrics is reported to improve the understanding of this disease.
Clinical data
The patient was a boy over 10 years old,whose main cause was "intermittent vomiting with decreased appetite for more than 2 months,and blood creatinine increased for 9 days".The patient showed no obvious cause of loss of appetite and vomiting for 2 to 3 times/day after 2 months.The upper gastrointestinal imaging was improved in local hospital in January before admission. The vomiting symptoms of the children were not significantly relieved 9 days before admission, and they were seen again in the local hospital,and urine routine was improved:proportion 1.014,urine protein negative,4 white blood cells/HP and 0 red blood cells/HP.Biochemistry:creatinine 198umol/L, urea 8.9mmol/L; CRP is 35.3 mg/L;Routine urine reexamination was performed on the day of admission on the 9th day of omeprazole,melocillin and xiyan calmness:1.012,urine protein 2+,urine sugar+,4-6 white blood cells/HP and 0-1 red blood cells /HP. Biochemistry: creatinine 224.9umol/L,albumin 39.9g/L, urea 5.3mmol/L, for further diagnosis and treatment in the hospital. No fever,edema,less urine,increased nocturnal urine,no rash,fear of heat less sweat,no limb end pain,joint pain.Since the onset,the child has lost 7Kg of weight.The maternal grandmother has a history of kidney disease,the specific unknown. Physical examination: blood pressure 110/65mmhg,mental clarity,stable breathing,obesity,BMI 22.3kg/m2.There was no skin rash or hair follicle keratosis,no obvious abnormality in the physical examination of heart,lung,abdomen and nervous system,no obvious edema in the whole body,no swelling and limited movement of the joints.Laboratory tests:urine specific gravity 1.006 uric sugar+,urinary protein+,microscopic observation of 1-3 white blood cells/HP,0-1 red blood cells /HP; 24-hour urinary protein 808.8mg/d;Urine protein electrophoresis:0%of macromolecules,43.9%of medium and 56.1%of small proteins;24-hour urinary calcium is normal;24-hour urinary creatinine clearance rate was 24.4ml/min; EGFR 23.02 ml/min. Urinary cupramine 0.43g/L;Urinary albumin 5.29mg/dL up;Urine transferritin 0.26mg/dL up,urine IgG determination 1.99mg/dL up; Urea 2 microglobulin 3.38mg/L?Urinary retinol binding protein 9.72mg/dL up; Urine N- acetylace-d amino glucosidase quantitative 68U/L? Uria 1 microglobulin 12.7mg/dL up.Blood routine:white blood cell count 9.81 x 109/L,hemoglobin 103g/L,platelet 509 x 109/L. Blood biochemistry:creatinine 239umol/L,urea 6.2mmol/L,cystatin C 2.9mg/L,albumin 40g/L.Blood gas analysis:PH 7.393, co2 partial pressure 29.2mmHg, plasma bicarbonate of hydrogen 17.40,be-6.6.Humoral immunity and cellular immunity were generally normal.ANA,ANCA negative;C3,1.67g/L.ASO,536 iu/ml;Echo,COX,EB virus antibody IgG positive,IgM negative;IgM parvovirus antibody,negative;T cells were negative for TB infection.Two halves of hepatitis b,hepatitis c,syphilis and HIV antibody negative. Galactosidase 0.9-1.3nmol/h/mg/Pr (reference range 29-64.4nmol/h/mg/Pr); 1.6-galactosidase 156.1-172.0nmol/h/mg/Pr (reference range: 88-220nmol/h/mg/Pr). No obvious abnormalities were found in abdominal ultrasound, urinary system ultrasound and echocardiography. Chest film:thick lung markings.
Renal biopsy pathology:a total of 22 glomeruli were taken with light microscopy(Fig.1A-1C).The number of glomerular cells was not significantly increased, and occasionally segmental mesangial cell proliferation and mesangial matrix were increased.Most capillary loops open well. No obvious thickening was observed in GBM.Renal tubular epithelial cells can be seen here with vacuolar degeneration stage brush edge exfoliation.A proteinaceous tubule is seen in the lumen.Slight TBM thickening was observed in diffuse distribution. Infiltration of lymphocytes was observed in some renal tubular walls. Diffuse edema can be seen in the interstitium, accompanied by infiltration of numerous lymphocytes, monocytes,eosinophils,neutrophils and plasma cells.No obvious abnormality was found in small renal vessels.Diagnosis:acute interstitial nephritis. No obvious abnormality was found in renal biopsy immunofluorescence.Electron microscopy(Fig.1D)showed few mesangial cells and mesangial substrates without electron dense deposition.The layered medullary phospholiform body and zebra body can be seen in the foot cells.No obvious abnormalities were found in GBM. Renal interstitial edema,mild collagen hyperplasia and a large number of lymphocytes,monocytes,plasma cells,eosinophil infiltration.Diagnosis by electron microscopy:1.Consistent with Fabry disease;2.Consistent with acute interstitial nephritis.
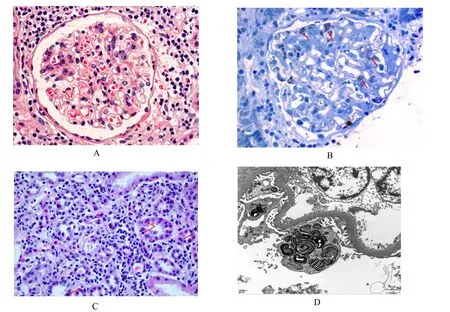
Fig.1 Renal biopsy pathology
Methylprednisolone was administered with 400mg/d shock for 3 days,followed by oral administration of methylprednisolone and gradual reduction, and methylprednisolone was stopped on August 26,2017.At present,the patient's urine sugar was normal,and the fluctuation of creatinine was at 27 weeks mol/L-74 weeks mol/L,eGFR 70ml/min-84.6ml/min,and the urinary protein was continuously negative.
Document literature
By taking "Fabry disease, acute renal tubular interstitial nephritis"and"Fabry disease,"and"acute tubule-interstitial nephritis" in PubMed, OVID and other medical literature databases including CNKI and wanfang in China,the retrieval time of each database was from the establishment of database to December 2017. Through comprehensive literature retrieval, there are no reports of Fabry disease with ATIN.
Discussion
ATIN is a group of clinicopathological syndromes caused by a variety of etiologies, which are characterized by acute renal insufficiency or failure, mainly by renal interstitial edema, renal interstitial inflammatory infiltration and tubular inflammation,and less involving glomeruli and blood vessels.First reported by Councilman,the disease has been gradually recognized by people and its incidence is on the rise[1,2].In addition,ATIN is an important cause of Acute renal failure(ARF).It is reported in literature that the percentage of children in ARF renal biopsy pathology is 0.87-15.7% [3]. The clinical manifestations of childhood were lack of specificity.Typical triad manifestations: fever, rash, and eosinophil are rare, accounting for 1.1-7% [4].Application before the onset of the children with a variety of drugs,clinical performance for creatinine increased sex,with low proportion of urine,glycosuria,urine protein electrophoresis of medium and small molecular protein (56.1%), strongly suggest renal tubular interstitial lesions, further biopsy showed visible diffuse distribution of renal tubule interstitial edema, accompanied by a large number of lymphocytes,monocytes and scattered eosinophils and neutrophils,plasma cell infiltration,so ATIN clear.This child also does not have typical trigeminal manifestations,so it should be noted that the idiopathic ATIN is excluded. Repeated ophthalmological examination has not shown the change of iris ciliary body inflammation,so the possibility of idiopathic ATIN is small.
Overseas retrospective analysis of pathological reports[5]showed no significant difference in renal function recovery between the two groups with or without glucocorticoid therapy.However,most studies supported the use of glucocorticoids,believing that the application of glucocorticoids can improve and accelerate renal function recovery and prevent renal interstitial fibrosis and further damage.The patient was treated with methylprednisolone 400mg/d after 3 days,and the renal function returned to normal and the urinary protein turned negative.
In addition, another prominent pathological presentation of the kidney in this child was electron microscopy showing the stratified medullary phosphatlike body and the formation of zebras and the fusion of foot processes.The above lesions support the diagnosis of Fabry disease in children.In 1897,Anderson and Fabry respectively reported two patients with multiple angioglioma, proteinuria and lymphedema, and proposed that the disease was a comprehensive disease involving skin and blood vessels. In 1955, it was named anderson-fabry disease,also known as Fabry disease[6].
Fabry's disease as an x-linked genetic lysosomal storage disorder,is due to the disease in Xq21.33-xq22 alpha galactose glucoside enzyme encoded on A(alpha galactosidase.A,alpha GalA)gene(GLA)gene mutations can lead to alpha A galactose glucoside enzyme activity decreased,the alpha galactose residues from neutral sugar lipid molecules over from blocked the scabbard,which caused the melamine hexose amide(globotriao sylceramide,Gb3)in including skin, kidneys, heart, central nervous tissue of abnormal deposition,As a result,the function of multiple organs is damaged[7].
Fabry disease can be divided into two categories, namely classic and late hairstyle according to clinical manifestations.It is reported that 4-year-olds can show symptoms of Fabry disease commonly seen in men[8].In patients,the activity of cirs-gala is very low, resulting in extensive deposition of a large number of sphingolipids in the body.Clinical symptoms can be characterized by dry skin without khan,paroxysmal limbs pain, skin vascular glioma,corneal opacity, gastrointestinal discomfort,muscle joint pain [9], as the illness progress gradually appear in patients with progressive renal damage, initially for kidney dysfunction,concentrate then gradually appear a large amount of proteinuria, further development can appear kidney failure.The cardiovascular system may also appear hypertrophy, arrhythmia, valvular heart disease,heart failure,myocardial ischemia or infarction,etc.Cerebral hemorrhage and cerebral infarction can occur in the central nervous system,and serious complications can threaten patients'life [10].The other type is late hairstyle: the characteristic depends on its happening time is late than classics model commonly,call not classic Fabry disease.The patient retains part of his or her activity,and the clinical symptoms are relatively mild,either asymptomatic or merely involving a single organ such as a dirty or kidney.
The kidney damage of Fabry disease is usually most prominent in glomerular lesions,followed by renal tubular and interstitial vascular lesions.After the destruction of the epithelial cells in the renal glomerulus,the early stage is foot protrusion and damage. After that, the basement membrane directly contacts with and sticks to the epithelial cells, resulting in thickening of basement membrane,proliferation of mesangial membranes,increase of extracellular matrix,capillary loops collapse, and glomerular sclerosis. Gb3 accumulation in renal tubular epithelial cells also leads to focal renal tubular atrophy, loss of function of the upstream glomeruli,compensatory hypertrophy of other glomeruli,ultrafiltration,and focal segmental glomerulosclerosis. Gb3 accumulation in renal vessels leads to endothelial cell necrosis, smooth muscle proliferation,interstitial fibrosis,and vascular wall thickening.Vascular occlusion causes renal ischemic changes,and also participates in the formation of glomerular sclerosis.
There is no specific cure method for Fabry disease at present, and gene recombinant GlA replacement therapy is the only specific clinical treatment method at present.Enzyme replacement therapy can replenish GlA in the body of patients, reduce blood Gb3 concentration and the accumulation of Gb3 in the body of cellular lysozyme, and prevent or delay the occurrence of various diseases[11].At present,there is no clinical manifestation of Fabry disease,and there is no effective way to obtain therapeutic drugs,so there is no alternative treatment.
The children for more than 10 years old boy,acute onset, clinical vomiting as the main performance,blood biochemical prompt creatinine increased significantly,urine protein increased significantly,the CCr and eGFR reduced obviously, significantly increased renal tubular damage markers, with compensatory metabolic acidosis, renal biopsy pathology prompt renal tubular epithelial cells visible level of denaturation loss of brush border. A proteinaceous tubule is seen in the lumen.Slight TBM thickening was observed in diffuse distribution.Infiltration of lymphocytes was observed in some renal tubular walls. Diffuse edema can be seen in the interstitium,accompanied by infiltration of numerous lymphocytes,monocytes,eosinophils,neutrophils and plasma cells. Therefore, the diagnosis of acute interstitial nephritis is clear.Before the onset of the disease,children have a variety of drug application history,such as xiyanping,meloxilin,omeprazole,etc.,considering that the above drugs may be related to the ATIN, some studies suggest that the storage of glycolipids may cause youdao autoimmune response[12], and the analogues of Gb3 can induce glomerulonephritis [13].The first symptom of this patient was ATIN.Only laboratory examination and renal biopsy electron microscopy supported the diagnosis of Fabry disease without obvious typical clinical manifestations of Fabry disease.Therefore,the diagnosis of acute interstitial nephritis combined with Fabry disease was considered.
In this case, there was no obvious clinical manifestation of Fabry disease,such as skin rash,joint pain and limb end pain.The results of renal biopsy revealed that electron microscopy suggested the formation of layered myelophosphat-like bodies and zebras in the podocyte cells, the fusion of foot processes and segments,and further investigation of the deactivation of galactosidase, leading to the establishment of Fabry disease. Therefore, electron microscopy plays an important role in the diagnosis of complex diseases. According to the morphological clues, the enzyme and gene examinations can be selected appropriately for further diagnosis and targeted treatment.This case is the first reported case of Fabry with acute interstitial nephritis.The treatment,outcome and prognosis of children with Fabry disease complicated with acute interstitial nephritis still require further follow-up observation and study.The main clinical manifestations of this patient were renal insufficiency, with no obvious extrarenal manifestations,and the diagnosis was made by renal biopsy cases with light and electron microscopy.It is suggested that the diagnosis of renal insufficiency should be confirmed by renal puncture biopsy and early treatment should be sought.
1. Bomback A S, Markowitz G S. Increased prevalence of acute interstitial nephritis:more disease or simply more detection?.Nephrology Dialysis Transplantation,2012,28:16-18.
2. Goicoechea M."Increased prevalence of acute tubulointerstitial nephritis." Nephrology Dialysis Transplantation,2012,1:112-115.
3. Van Biljon G.Causes,prognostic factors and treatment results of acute renal failure in children treated in a tertiary hospital in South Africa.Journal of Tropical Pediatrics,2008,54:233-237.
4. Clarkson M R,Giblin L,O'connell F P,et al.Acute interstitial nephritis: clinical features and response to corticosteroid therapy.Nephrology Dialysis Transplantation,2004,19:2778-2783.
5. Raza M N,Hadid M,Keen C E,et al.Acute tubulointerstitial nephritis, treatment with steroid and impact on renal outcomes.Nephrology,2012,17:748-753.
6. China Fabry disease expert cooperation group.China Fabry disease(Fabry disease)diagnosis and treatment expert consensus. Chinese Medical Journal,2013,93:243-247.
7. Germain D P.Fabry disease.Orphanet Journal of Rare Diseases,2010,5:30.
8. Liu YP,Huang Y,Wang J,et al.Fabry's disease at age 4: a case report. Journal of Peking University(medical edition),2013,45:307-311.
9. Zhang W,Kang MD,Zhao YW,et al.Clinical characteristics of multiple organ lesions in patients with fabry's disease.Chinese Journal of Medicine,2015,95:1829-1832.
10. Hwu W L, Chien Y H, Lee N C, et al.Newborn screening for Fabry disease in Taiwan reveals a high incidence of the later‐onset GLA mutation c.936+919G>A(IVS4+919G>A).Human Mutation,2009,30:1397-1405.
11. Li YK,Chen N,Zhang SG.Status of fabry's disease diagnosis and progress of enzyme replacement therapy. Chinese Journal of Nephrology,2017,2:150-154.
12. Hamers M N,Donker-Koopman W E,Dupouey P,et al. Characterization of antibodies against ceramidetrihexoside and globoside.Immunochemistry,1978,15:353-358.
杂志排行
Clinical Research Communications的其它文章
- Treatment of refractory H.pylori by Chai Ping Decoction:two case reports
- A protocol for the reporting and methodological quality of robotic surgery case reports
- Research progress of microRNA in prevention and treatment of osteonecrosis of the femoral head
- Research progress of continuous nursing care in patients with percutaneous coronary intervention