Psychosocial Stress, the Unpredictability Schema, and Cardiovascular Disease in Women
2018-02-28TomCabezadeBacaPhDandMichelleAlbertMDMPH
Tom á s Cabeza de Baca, PhD and Michelle A. Albert, MD, MPH
1 Department of Medicine, University of California, San Francisco, 505 Parnassus Avenue, San Francisco, CA 94117, USA
Abstract Depression/anxiety-related disorders and psychosocial stress have been implicated as cardiovascular disease (CVD) risk factors. Women are at considerable risk for a ffective disorders and report greater severity from psychosocial stress, compared to men. Affective disorders and cardiovascular disease likely share underlying pathophysiological mechanisms that are potentiated among women - especially younger women. Environmental stressors that threaten the safety, security, and status of an individual are appraised by the brain, producing a cascade of evoked physiological and cognitive responses. In the short term, these processes overcome stressors, but come with long-term health implications. Chronic psychosocial stress leads to a dysregulation of the stress response systems that can lead to a heightened stress appraisal schema called the unpredictability schema, a construct that might arguably place women at heightened risk for CVD.
Keywords: cardiovascular disease ; psychological stress ; depression ; anxiety ; W omen ; unpredictability schema ; life history theory; psychosocial stress
Introduction
Women’ s cardiovascular health is in part impacted by: (1) physiological and biological systems and(2) the societal and community demands unique to the female gender [ 1, 2]. Women have higher prevalence of stress-related mental disorders such as depression or anxiety than men [ 3 - 5]. It is increasingly acknowledged that the relationship between cardiovascular disease (CVD) and depression/anxiety-related disorders is highly prevalent in women, especially in younger women [ 6 - 9T h]. us,this review focuses on CVD and affective disorders(e.g., anxiety, post-traumatic stress disorder (PTSD),and depression) as end-products that potentially result from overcoming a lifetime of environmental and psychosocial stress. Stressors may serve as cues that convey key information about the condition and availability of resources in the immediate environment that are processed by the brain and conveyed to the circulatory system and the rest of the body via the autonomic nervous system, hypopituitary-adrenal axis, and inf ammatory processes[ 10]. Individuals identify the level of predictability,controllability, and safety present in the environment through a cognitive perceptual and appraisal system called the unpredictability schema [ 1 1 ]. The inf uence of environmental stressors spans across physiology, development, behavior and, ultimately,health. We provide a conceptual explanation of the unpredictability schema, followed by short sections def ning psychosocial stress and reviewing its impact on CVD risk in women.
The Unpredictability Schema: Affect and Cardiovascular Disease
The brain has been characterized as the “ central organ of stress ” [ 12, 13] because it perceives,appraises, and labels external environmental stimuli as either safe or threatening (see Figure 1 ).Contingent on the assessments of the brain appraisal system, bio-ener getic resources are mobilized across physiological systems to create a coordinated stress response [ 10 , 12 - 14F o]. r instance, the autonomic nervous system - notably the vagal nerve - is hypothesized to be an organizer for social behavior across phylogenetic time [ 15]. When an individual perceives themselves to be in an unsafe or threatening situation, the stressor evokes a physiological response that activates the sympathetic nervous system [ 15]. Sympathetic activation creates a cascade of coordinated responses within the circulatory system (among others) designed to overcome the stressor. Because the circulatory system is designed to attend to ur gent threats to health (e.g., wounds,viral/bacterial infections etc.) and to mobilize and transport resources and defenses (i.e., nutrients,oxygen, hormones, cytokines) across tissues, the coordinated response includes increased heart rate,vasodilation and mobilization of oxygenated blood to the extremities with diversion of resources away from vital or gans. Blood during a stress response becomes increasingly coagulated and the immune system is mobilized. These physiological responses were designed to facilitate adaptive behaviors that would quickly overcome environmental challenges in the short term.
Over time, repeated exposure to stress and stress response activation results in physiological, neurological, and brain re-or ganization that canalize stress responses and cognitive adaptations in ways that help individuals specialize and sensitize to the features of their immediate environment [ 10,14 , 16 - 18C ]. hronic stress alters brain anatomy by increasing amygdala functioning (e.g., vigilance), decreasing ventral striatal reward sensitivity (e.g., reward-seeking behavior), and decreasing executive functioning of the prefrontal cortex (e.g.,impulsive behavior) [ 14, 17]. Pervasive and longterm activation of these brain and stress response systems from chronic stress results in dysregulation of the stress response system [ 12 , 19 ] and greater vigilance and impulsive behavior [ 10 , 20 ]. These adaptations, however, come with upstream costs.These adaptations manifest as decrements in mental and physical health - such as depression and CVD -through exogenous (i.e., dysregulation of the stress response systems) and endogenous pathways (i.e.,increased risk-taking, decreased health-maintaining behavior, and decreased interoceptive awareness)[ 13 , 21 ]( Figure 2 ).
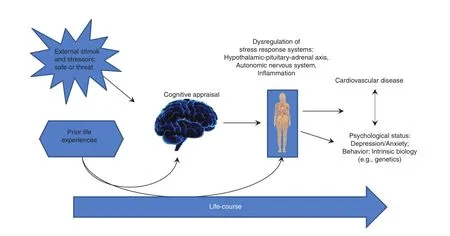
Figure 1 Potential Life-Course Pathways of Cardiovascular Disease and Mental Psychological Stress.
Evidence suggests that early and repeated exposure to stressful or threatening environments can shape worldviews and perceptions in a manner that orients individuals toward perceiving society and the environment as unpredictable, unreliable, threatening, and hostile, and discounting the future [ 11,16, 22]. This cognitive orientation has been called the unpredictability schema [ 1 1 , 23 ] and includes behavioral and af fective components of decreased perceptions of control, increased pessimism, hostility, and vigilance (see Table 1 for additional components of the unpredictability schema).
The unpredictability schema and its components have been linked to greater anxiety and depressive symptoms, increased reward-seeking and risktaking and poor health-maintaining behavior (e.g.,over-eating) [ 24 , 26 - 28I n]. deed, research documents increased drive for reward-seeking behavior,following chronic stress exposure [ 14, 21]. Further,brain systems calibrated by chronic stress response such as the ventral striatum are implicated in increasing health-harming, reward-seeking behaviors [ 14].For example, smoking is one traditional healthharming/reward-seeking behavior both implicated in cardiovascular risk and associated with exposure to higher levels of stress [ 29 - 31T o]r. res and O ’ Dell[ 30], using extensive research from animal models, propose that females are especially sensitive tonicotine, with stress heightening nicotine sensitivity in neuro-reward pathways and increasing intensity of withdrawal.
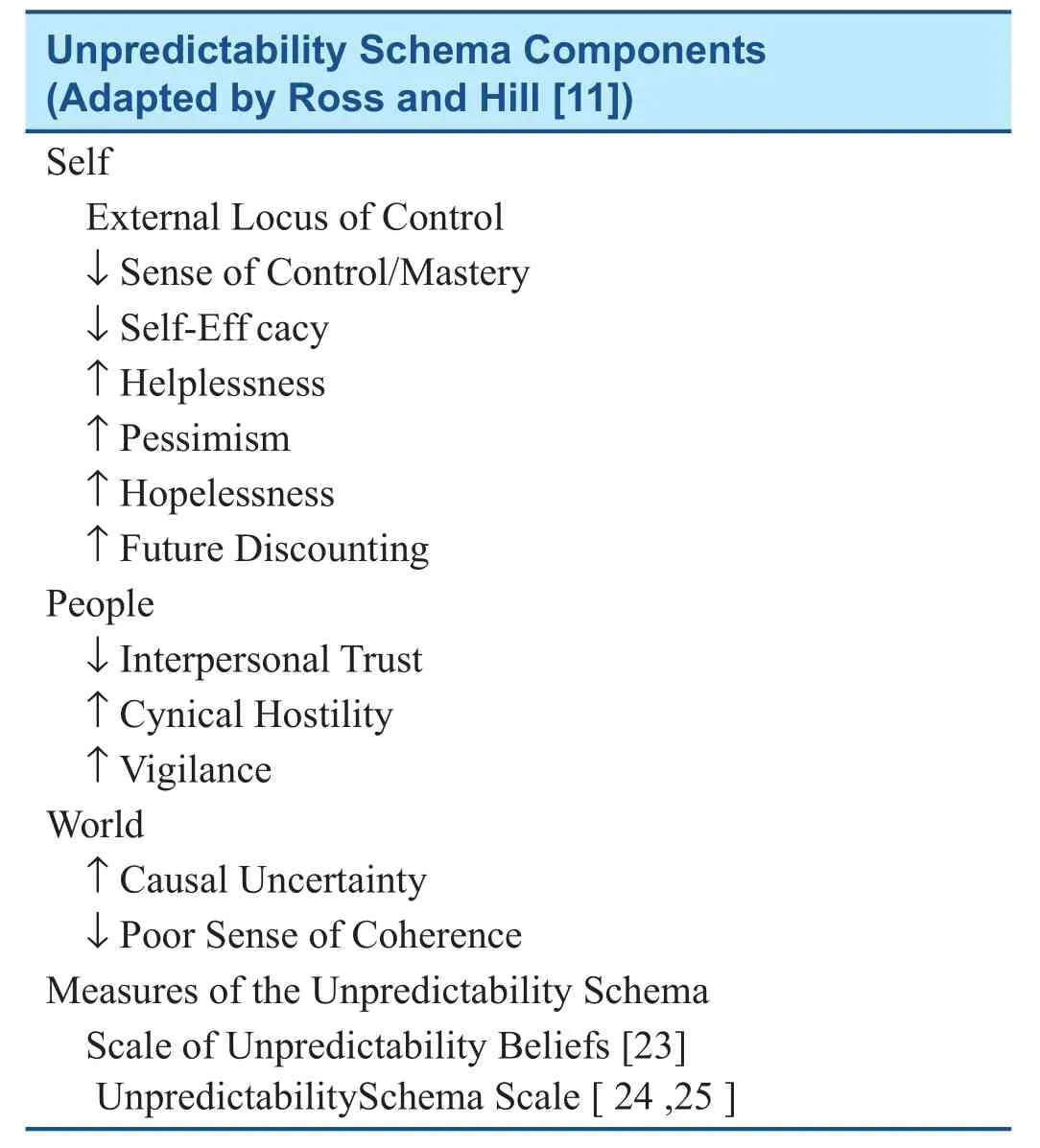
Table 1 Description of the Unpredictability Schema.
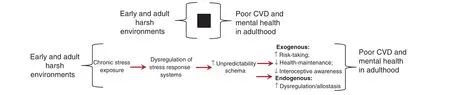
Figure 2 The “ Black Box” of Harsh Environments and Poor CVD Health in Adulthood.
In addition to increased reward-seeking, risk-taking and decreased health-maintenance, the unpredictability schema may produce a reduction in interoceptive awareness [ 24]. Interoceptive awareness is the perceptual processing of internal bodily states such as pain and hunger; conversely, exteroceptive awareness is the perceptual processing of external stimuli situated outside of the body [ 32].Evidence suggests that activation of one perceptual system may supersede the other [ 32]. Recent work on the unpredictability schema has proposed that early experiences of systemic chronic stress may orient individuals toward vigilance, which may alter perceptual systems to focus on exteroceptive awareness (external stimuli), foregoing interoceptive awareness (internal bodily sensations) [ 24].As predicted, the association between a heightened unpredictability schema was associated with decreased interoceptive awareness and over-eating[ 24]. Thus, it is possible that increased exteroceptive awareness, as a result of hyper-vigilance and stress response, may cause people to be less aware of bodily sensations.
Conceptualization of Psychosocial Stress and Stressors
An extensive literature exists that describes the conceptualization and measurement of stress and stressors [ 33 , 34 ]. A stressor is conceptualized as an environmental stimulus or event that threatens the security, autonomy, status, and, survival of an organism. Broadly, there exists three domains of stressors [ 33]: (1) negative life events , discrete events that individuals experience such as losing a job or death of a loved one, (2) chronic difficulties, sustained and long-term stressful situations,such as caring for a loved one or living in a disadvantaged neighborhood, and (3) cumulative stress exposure (lifetime stress) which is also known as the sum-total or culmination of chronic and acute life stressors across the lifespan. Stressors are further distinguished across development, whereby stressors experienced prenatally or in childhood/adolescence are categorized as early adversity and stressors following those developmental stages are adult stressors.
Harshness - def ned as “ external sources of disability and death ” that are independent of age and health [ 16 ] - and unpredictability - def ned as “ spatial variation in harshness ” [ 16] - have been suggested as relevant dimensions of environmental risk (i.e., life stressors) that convey key information about the safety, security, and controllability about the immediate environment and the reliability and trustworthiness of individuals present in the environment. Indeed, harshness and unpredictability help inform and link the disparate literature between mood disorders and CVD risk in women.
Women CVD and Psychosocial Stressors in Women
Psychosocial stress and its underlying components negatively impact cardiovascular health and mortality [ 35] (see Figure 1 ). The INTERHEART study showed that psychosocial factors were as potent to CVD risk (Odds Ratio (OR): 2.67, 95% Conf dence Intervals (CI): 2.21 - 3.22) as smoking (OR: 2.87,95% CI: 2.58 - 3.19) as other traditional risk factors, like Type II diabetes (OR: 2.37, 95% CI: 2.07 -2.71) [ 36]. Disaggregation of psychosocial stress in INTERHEART revealed that, compared to age- and sex-matched controls, patients with reported myocardial infarction had elevated psychosocial stress from different measured stress domains, including home and work stress, f nancial stress, stressful life events, and depression [ 37]. Additionally, patients had lowered perceived locus of control. A series of meta-analytic and pooled-analyses work continues to f nd support for an association between psychosocial stress and CVD, including hypertension [ 38],stroke (with greater risk in women) [ 39], coronary heart disease [ 40], and CVD death [ 41].
The examination of the relationship between assorted domains of life stress (e.g., work, relationship, health, jobs) among middle-aged and older adults (45 - 84 years old) on markers of endothelial dysfunction, a precursor to CVD, found that reporting two or more stressful life events compared to no life events were associated with greater endothelial dysfunction, as evidenced by decreased f ow-mediated dilation and higher levels of I-CAM1 [ 42]. The sequelae of work stress have been an extensively studied stress domain. Meta-analyses have found an association between work stress and CVD [ 43],including stroke risk [ 44]. Specif cally focusing on women, prospective work in the Women’ s Health Study (WHS) highlighted the signif cance of psychosocial stress [ 45], by examining the effects of job strain on incident CVD risk [ 46]. Both high strain,characterized by a combination of low control and high demands, and active strain, characterized by high control and high demands, were associated with greater risk of acute cardiovascular events [ 46].Caregiver burden has also been implicated in CVD risk. Current [HR: 1.35, 95% CI: 1.06 - 1.68] and long-term care of a spouse [HR: 1.95, 95% CI: 1.19-3.18] have found strong associations between caregiving and CVD risk [ 47]. Caring for an ill spouse at ≥ 9 hours a week (RR: 1.82, 95% CI: 1.08 - 3.05)compared to 0 hours a week was associated with greater CVD risk in the Nurse’ s Health Study [ 48].
Women hospitalized for Takotsubo or stressinduced cardiomyopathy, a diagnosis more prevalent in women, were more likely to report experiencing greater negative life events than unexposed women [ 49]. Other work in middle-aged adult men and women with stable coronary heart disease demonstrates that women (particularly younger women, e.g., ≤ 50 years old), compared to men, are at greater risk for mental stress-induced myocardial ischemia [ 50]. In this study, women experienced higher levels of myocardial ischemia in response to mentally-induced stress compared to men (OR:2.06, 95% CI: 1.12 - 3.79). These f ndings were more potent in younger women (e.g., ≤ 50 years old) where women had a 4-fold higher likelihood of mentally-induced stress ischemia compared to their male counterparts. This work may have relevance for the observed phenomenon in women aff icted with chest pain and without epicardial coronary artery disease. Additional work suggests that mental health status may moderate the association between life stressors and cardiovascular health. In a sample of 28,583 US men and women (mean age = 44.8;female = 57.6%), the association between negative life events and CVD incidence was stronger in participants who reported a history of depression [ 51],suggesting that psychological status may amplify the ef fects of negative life events. Furthermore,early adversity has been implicated in the progression of CVD risk [ 52]. Some research suggests that the effects of early adversity may be more potent in women, as well as heightened in women with stressful life experiences in adulthood [ 53]. Table 2 outlines studies of psychological status with a focus on stress and CVD in women.
Psychological Status and CVD Risk:Intersection of Sex and Race/Ethnicity
As reviewed by Mehta and colleagues [ 1], women of color, including Hispanic/Latinas and black women, experience more severe physical and mental comorbidities and greater cardiovascular complications at younger ages than other women.Although not only limited to U.S. women belonging to racial/ethnic minority groups, earlier progression of CVD in women is more pronounced in women with depression or anxiety disorders [ 1,58]. Further, because racial/ethnic minority women are more likely to reside in harsh, unpredictable,and uncontrollable environments, they are more likely to encounter chronic stress exposure across the lifespan, potentially making ethnic and racial minority women more susceptible to CVD as a result of their life experiences. Additionally, nativity status is another important CVD factor to consider among racial/ethnic minorities. For example,foreign-born Hispanics/Latinos have greater risk of CVD death than US-born Hispanic/Latinos, the risk is highest among Cubans, then Puerto Ricans, and Mexicans [ 59 ].
Exposure to adversity among racial/ethnic minorities begins early in life. Racial/ethnic minorities,and economically-disadvantaged children have been reported to experience more adversity than white and economically-privileged children [ 60].Evidence suggests that a dose-effect of early adversity on adult cardiovascular health exists. Men and women who reported 3 or more early adverse (ACE)events compared to no events had greater CVD risk(OR: 2.14, 95% CI: 1.56 - 2.94) and the ef fect was most potent in individuals who reported 2 or more adult life events (OR: 3.00, 95% CI: 1.74 - 5.20)[ 53 ]. When stratif ed by sex, the association was only signif cant among women [ 53]. This trend continues into later adulthood and may be partially attributed to socioeconomic status.
Data from the Women’ s Health Study (WHS)showed that markers of economic prestige (higher education and income) were protective against prospective cardiovascular events over 10 years,even after control for traditional cardiovascular risk factors and novel CVD surrogate biomarkers markers such as C-reactive protein [ 61]. Emerging work from WHS demonstrates that cumulative psychosocial stress, a composited measure consisting of acute negative life events and chronic stressors was signif cantly higher among Blacks,Hispanics, and Asians when compared to White women, even when after accounting for SES anddepression/anxiety [ 62]. Other work in a sample of over 9000 men and women similarly f nds that poorer psychological quality is related with decrease likelihood of attaining ideal or intermediate cardiovascular health status [ 57]. Trauma exposure [ 54,55] and PTSD symptoms arising from trauma [ 8]are also substantial CVD risk factors [ 8, 63].
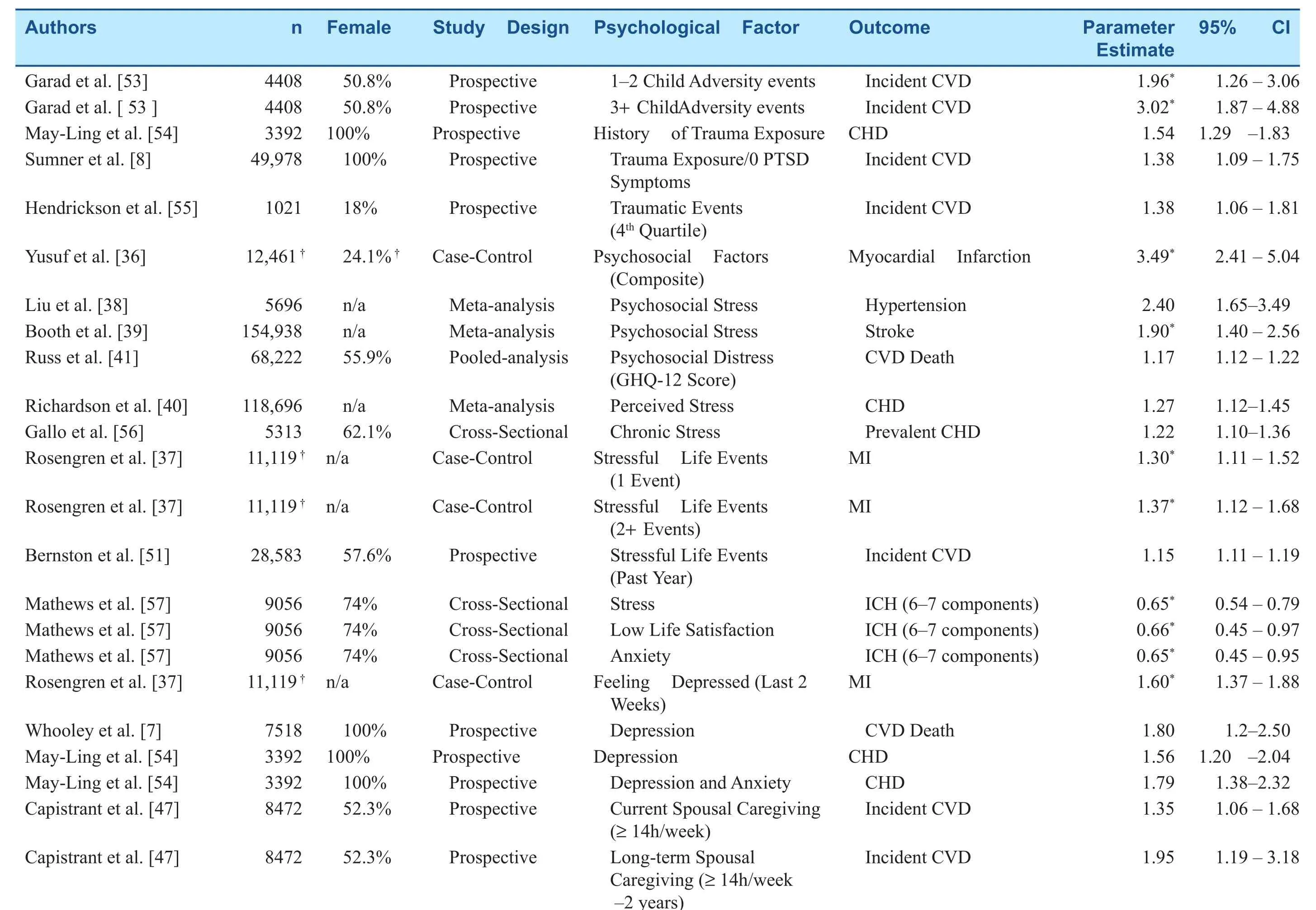
Table 2 Selected Summary of Psychosocial Status Papers with a Focus on Stress and Cardiovascular Disease Risk.

Table 2(continued)
Unique Global Environmental Threats Faced by Women
Across the globe, women encounter distinct life experiences that may amplify the risk of mental illness and cardiovascular disease. At birth and infancy, some groups experience a greater “ loss” of female babies than is expected [ 64]. Additionally,young girls in select cultures and environments may experience reduced access to health care, increasing risk of child mortality [ 65]. Early stressful experiences marked by sexual, emotional and physical abuse are more likely to be reported by women and individuals from disadvantaged economic backgrounds [ 66]. Women are also disproportionately at risk for increased poverty than men [ 67, 68]. As such, greater poverty increases the likelihood that women will be exposed to or reside in harsh and unpredictable neighborhoods [ 69, 70] or will report more negative life events [ 71], with U.S minority women and their offspring experiencing higher levels of poverty than white women [ 68]. For example, in 2015, Black women had the highest levels of poverty (23.1%), followed by Native American(22.7%), Hispanic/Latinas (20.9%), and Asian women (1 1.7%) [ 68]. Furthermore, women will be more likely to sustain households with minimal resources [ 72, 73]. Overall, thus, women, across their life span, may potentially encounter adverse environments and experience negative life events that may impact mental and cardiovascular health.
Sex, Environmental Appraisal,and Processing
In addition to unique lived experiences of some women, evidence suggests potential differential processing of environmental information by sex; differences that may emer ge at puberty [ 74].Humans have an evolutionary history of cooperation and reliance on others for security, resources and survival [ 75]. For this reason, humans, among other social animals, have an intense drive for connection and need to belong [ 76], which emer ges early in life through the attachment to caregivers and persists in adulthood through romantic relationships and familial/friendship bonds. As such,any stressor that deprives an individual of social connection, threatens an individual ’ s status, and/or ostracizes an individual from a group, can result in marked negative physiological responses [ 77 - 79 ].Perceptions of stress are also inf uenced by social connections. Individuals who report depression,lower social support, a recent relationship dissolution, or family conf ict report higher levels of perceived stress [ 71]. The impact of psychological stress on health may be contingent on the appraised level of social support available to the individual in their immediate environment. In particular toxic stress [ 80 ], def ned by adverse experiences without social support and unhealthy brain architecture results in illness compared to both positive or tolerable stress which are both associated with good social support and healthy brain architecture [ 81].Indeed, evidence shows heightened diastolic blood pressure reactivity to acute stress in lonelier individuals, with the effect particularly more potent in women [ 82]. Loneliness has been linked with lower quality support networks (i.e., smaller support networks, less emotional and practical support) [ 82].Indeed, a study by Steptoe et al. found that social isolation/loneliness contributes to increased stroke and coronary artery disease risk, as well as all-cause mortality among 6500 participants of the English Longitudinal Study of Ageing (ELSA) [ 83].
Some research suggests that differences in estrogen and oxytocin levels by sex may differentially modulate the stress response [ 84 - 86E ]l. evated levels of sustained inf ammation, as measured by surrogate inf ammatory biomarkers like C-reactive protein, may be the result of a dysregulated glucocorticoid stress response and reduction in antiinf ammatory effects [ 87].
Finally, the relationship between stressful life experiences and CVD progression may also be implicated by telomere attrition. Telomeres are nucleoprotein sequences that serve as protective caps that conserve the cellular integrity of chromosomes and have been demonstrated to be shorter in women with elevated psychosocial stress and in individuals with recent stressful life events [ 88, 89]. Furthermore, individuals aff icted with affective disorders had signif cantly shorter telomeres when compared to age-matched controls [ 90], and other evidence suggests that chronicity of affective disorders is also linked with shorter telomeres [ 91]. In totality, emerging evidence suggests an interplay between psychosocial stressors, the unpredictability schema and chronic diseases such as cardiovascular disease.
Conflict of Interest
The authors declare no conf ict of interest.
杂志排行
Cardiovascular Innovations and Applications的其它文章
- Challenges in Cardiovascular Risk Prediction and Stratification in Women
- Nonobstructive Coronary Artery Disease in Women: Risk Factors and Noninvasive Diagnostic Assessment
- Antiplatelet Therapy Considerations in Women
- Novel Imaging Approaches for the Diagnosis of Stable Ischemic Heart Disease in Women
- Heart Disease in Pregnancy: A Special Look at Peripartum Cardiomyopathy
- Heart Failure with Preserved Ejection Fraction:Time to Revisit the Stiff Heart