Ⅲc期卵巢癌淋巴结转移对患者预后的影响
2018-01-06孙墨红苑中甫通讯作者
孙墨红 苑中甫(通讯作者)
452470登封市妇幼保健院妇科1 450052河南省郑州大学第一附属医院2
Ⅲc期卵巢癌淋巴结转移对患者预后的影响
孙墨红1,2苑中甫(通讯作者)2
452470登封市妇幼保健院妇科1450052河南省郑州大学第一附属医院2
目的:探讨Ⅲc期卵巢癌淋巴结转移对患者预后的影响。方法:收治Ⅲc期卵巢癌患者40例,进行随访观察,记录疾病进展情况。结果:40例患者中,盆腔淋巴结转移10例中,3年生存率90.0%,5年生存率80.0%;30例腹膜转移中,3年生存率56.70%,5年生存率36.7%。残留病灶<1 cm 24例中,3年生存率79.2%,5年生存率54.2%;残留病灶>1 cm 16例中,3年生存率43.8%,5年生存率18.8%。腹膜转移生存率明显低于盆腔淋巴结转移(P<0.05),残留病灶>1 cm患者生存率明显低于残留病灶<1 cm患者(P<0.05)。结论:腹膜转移生存率明显低于盆腔淋巴结转移,残留病灶>1 cm患者生存率明显低于残留病灶<1 cm的患者。
Ⅲc期卵巢癌;淋巴结转移;腹膜转移;生存率
卵巢癌是女性生殖器官常见的肿瘤之一[1],死亡率较高[2],对妇女生命造成严重威胁。卵巢癌扩散的主要途径之一是淋巴结转移[3],宫颈癌国际妇产科联盟(FIGO)分期系统将存在淋巴转移的患者划分为Ⅲc期[4]。2011年2月-2012年5月收治Ⅲc期卵巢癌患者40例,进行回顾性分析,现报告如下。
资料与方法
2011年2月-2012年5月收治Ⅲc期卵巢癌患者40例,年龄28~73岁,平均(39.6±5.2)岁。所有患者均接受规范性手术治疗,术后无病灶残留或者残留灶<1 cm 24例(60.0%),术后残留灶>1 cm 16例(40.0%)。腹腔腹膜种植直径>2 cm不考虑淋巴结转移者30例,有盆腔淋巴结转移者10例。
方法:对所有患者进行随访观察,并记录疾病进展情况。
结 果
40例Ⅲc期卵巢癌患者3年、5年生存率情况:盆腔淋巴结转移10例中,3年生存9例,3年生存率90.0%;5年生存8例,5年生存率80.0%。30例腹膜转移中,3年生存17例,3年生存率56.70%;5年生存11例,5年生存率36.7%。残留病灶<1 cm 24例中,3年生存19例,3年生存率79.2%;5年生存13例,5年生存率54.2%。残留病灶>1 cm 16例中,3年生存7例,3年生存率43.8%;5年生存3例,5年生存率18.8%。腹膜转移生存率明显低于盆腔淋巴结转移的患者,差异有统计学意义(P<0.05)。残留病灶>1 cm患者生存率明显低于残留病灶≤1 cm的患者,差异有统计学意义(P<0.05),见表1。
讨 论
卵巢癌淋巴结转移途经主要有3条途经[5]:①沿卵巢血管上行注入腹主动脉旁淋巴结或腰淋巴结;②沿阔韧带下行注入髂内、髂外、髂间或髂总淋巴结,不论上行路线是否受阻,实际上两条途经常同时存在,这可以解释临床上卵巢癌盆腔淋巴结转移和腹主动脉旁淋巴结转移的机会几乎相等;③极少数沿圆韧带注入髂外尾部和腹股沟淋巴结。及时和准确的诊断是否有腹膜后淋巴结转移,对治疗和预后有着重要的临床意义。
本组资料通过对40例Ⅲc期卵巢癌患者进行随访观察,结果发现,盆腔淋巴结转移10例中,3年生存9例,3年生存率90.0%;5年生存8例,5年生存率80.0%。30例腹膜转移中,3年生存17例,3年生存率56.70%;5年生存11例,5年生存率36.7%。残留病灶<1 cm 24例中,3年生存19例,3年生存率79.2%;5年生存13例,5年生存率54.2%。残留病灶>1 cm 16例中,3年生存7例,3年生存率43.8%;5年生存3例,5年生存率18.8%;腹膜转移生存率明显低于盆腔淋巴结转移的患者,差异有统计学意义(P<0.05)。残留病灶>1 cm患者生存率明显低于残留病灶<1 cm的患者,差异有统计学意义(P<0.05)。由此可见,腹膜转移生存率明显低于盆腔淋巴结转移的患者,残留病灶>1 cm患者生存率明显低于残留病灶≤1 cm的患者。
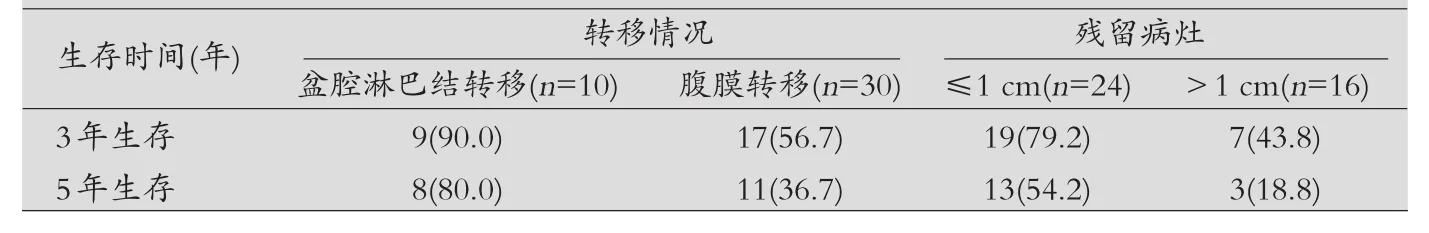
表1 患者预后分析[n(%)]
[1]Wang H,Wu XH,Shi L,et al.Lysophosphatidic acid promotes transplanted tumor growth of human epithelium ovarian cancer in nude mice[J].Nan Fang Yi Ke Da Xue Xue Bao,2013,27(2):228-231.
[2]Robert L Coleman,Alan Gordon,James Barter,et al.Early Changes in CA125 After Treatment with Pegylated Liposomal Doxorubicin or Topotecan Do Not Always Reflect Best Response in Recurrent Ovarian Cancer Patients[J].The Oncologist,2014,12:72-78.
[3]Benjapibal M,Neungton C.Pre-operative prediction of serum CA125 level in women with ovarian masses[J].J Med Assoc Thai,2014,90(10):1986-1991.
[4]Liguang Z,Peishu L,Hongluan M,et al.Survivin expression in ovarian cancer[J].Exp Oncol,2014,29(2):121-125.
[5]Gordon AN,Tonda M,Sun S,et al.Long-term survival advantange forwomen treated with pegylated liposomal doxorubicin compared with topotecan in a phase 3 randomized study of recurrent and refractory epithelial ovarian cancer[J].Gynecol Oncol,2014,95(1):1-8.
Influence of lymph node metastasis on prognosis of patients withⅢc stage ovarian cancer
Sun Mohong1,2,Yuan Zhongfu(Corresponding author)2
Department of Gynaecology,the Maternal and Child Health Hospital of Dengfeng City 4524701Department of Gynaecology,the First Affiliated Hospital of Zhengzhou University,Henan Province 4500522
Objective:To explore the influence of lymph node metastasis on prognosis of patients withⅢc stage ovarian cancer.Methods:40 patients withⅢc stage ovarian cancer were selected.We followed up and recorded the progress of the disease.Results:In the 40 patients,there were 10 cases with pelvic lymph node metastasis.The 3-year survival rate was 90%,and the 5-year survival rate was 80%.There were 30 cases with peritoneal carcinomatosis.The 3-year survival rate was 56.70%,and the 5-year survival rate was 36.7%.There were 24 cases with residual lesion less than 1 cm.The 3-year survival rate was 79.2%,and the 5-year survival rate was 54.2%.There were 16 cases with residual lesion more than 1 cm.The 3-year survival rate was 43.8%,and the 5-year survival rate was 18.8%.The survival rate of peritoneal metastasis was significantly lower than that of pelvic lymph node metastasis(P<0.05).The survival rate of patients with residual lesion less than 1 cm was significantly lower than that of patients with residual lesion more than 1 cm(P<0.05).Conclusion:The survival rate of peritoneal metastasis was significantly lower than that of pelvic lymph node metastasis.The survival rate of patients with residual lesion less than 1 cm was significantly lower than that of patients with residual lesion more than 1 cm.
Ⅲc stage ovarian cancer;Lymph node metastasis;Peritoneal metastasis;Survival rate
10.3969/j.issn.1007-614x.2017.35.11
