血清钾、钠联合肝转氨酶在钝性肝损伤中的临床价值研究
2017-12-21黄超,张坤,江艺
黄 超,张 坤,江 艺
·论 著·
血清钾、钠联合肝转氨酶在钝性肝损伤中的临床价值研究
黄 超,张 坤,江 艺
目的探讨血清钾、钠联合肝转氨酶在钝性肝损伤中的临床应用价值。方法回顾性分析2003年10月—2016年4月福州总医院收治的202例钝性肝脾损伤患者的临床资料。按是否存在肝损伤分为肝损伤组101例,无肝损伤组即脾损伤组101例;按肝损伤程度分为轻度肝损伤组53例,严重肝损伤组48例。检测两组血清钾(K+)、血清钠(Na+)、谷丙转氨酶(ALT)、谷草转氨酶(AST)的值,通过Logistic回归建立回归模型,绘制受试者工作特征曲线(ROC曲线)并计算曲线下面积(AUC)以评价单独及联合指标检测的诊断价值。通过ROC曲线确定ALT、AST在肝损伤中的最佳阈值及血清K+、Na+、ALT、AST在严重肝损伤中的最佳阈值。结果肝损伤与无肝损伤组血清K+、Na+、ALT、AST水平四种指标的差异有统计学意义(P<0.01);轻度与严重肝损伤组四种指标水平的差异有统计学意义(P<0.01)。对于判断闭合性腹部损伤是否合并肝损伤,联合指标检测的AUC大于单独检测的AUC,但差异无统计学意义(P>0.05);ALT单独和联合检测对肝损伤和非肝损伤的预测率分别为89.1%、94.1%;ALT单独判断肝损伤的敏感度和特异度分别为92.1%、93.1%,而联合检测则分别为93.1%、93.1%。对于判断钝性肝损伤是否为严重肝损伤,联合检测的AUC大于单独检测的AUC,且差异有统计学意义(P=0.043);ALT单独检测对轻度肝损伤和严重肝损伤的预测率分别为79.2%、58.3%,而联合则分别为81.1%、70.8%;ALT单独检测判断严重肝损伤的敏感度和特异度分别为83.3%、54.7%,而联合则分别为66.7%、94.3%。通过ROC曲线评估得出ALT、AST在肝损伤中的最佳阈值分别为57.55U/L、59.2U/L;血清K+、Na+、ALT、AST在严重肝损伤中的最佳阈值分别为3.685mmol/L、142.55mmol/L、171.50U/L、364.00U/L。血清K+和Na+水平在轻度和严重肝损伤组呈负相关(P=0.005,r=-0.382;P=0.001,r=-0.494),且在严重肝损伤中最为明显。结论肝转氨酶升高与肝损伤密切相关;肝功能联合电解质检测对临床鉴别钝性肝损伤是否为严重肝损伤有较高的准确性、预测性和特异度,可作为临床早期鉴别的一种初步有效的手段之一,从而为其治疗提供有力的证据。
肝损伤; 血清钾; 血清钠; 转氨酶
在各种腹部损伤中肝脏损伤占20%~30%,发病率仅次于脾脏,位居第二[1],若不能及时、有效地治疗,病死率高达55%~75%。因而,对其损伤程度的准确判断是降低病死率、减少并发症的关键。腹部创伤超声重点评估方案(focused abdominal sonography for trauma,FAST)对腹腔和盆腔游离液体的检测很敏感,但结果与操作者的技术经验有关,且有较多的局限性[2],主要为急诊FAST诊断钝性肝损伤的灵敏度只有64%,而当损伤仅涉及肝实质而无游离液体时,其灵敏度更低[3]。CT扫描不仅能够清晰地显示病变的范围及部位,而且对肝损伤的诊断及分级具有高度的特异性、敏感性和准确性,但需搬动患者、接触辐射、费用高、消耗时间长[4],因此仅适用于某些血流动力学稳定者[5]。在钝性肝损伤患者中,基本都会伴随着肝转氨酶的升高,但该指标用于肝损伤的预测和损伤程度的评估还未得到详细的研究。而且,有研究表明,肝转氨酶的升高往往不归因于缺血性肝炎(肝休克),而被认为是由冲击造成的[6-7]。此外,目前钝性肝损伤的术前诊断严重依赖于不能适用于所有患者的影像学检查。近年来,也有研究提出血清钾水平的监测和肝转氨酶水平的检测在钝性肝损伤患者中有重要意义,血清钾在严重肝损伤中会降低[8,18-22],而肝转氨酶的升高与肝损伤强烈相关[6,9-13]。基于上述相关现状及研究,为了明确实验室血清学指标检验与肝损伤的相关性,本研究回顾性分析2003年 10月—2016年4月福州总医院收治的202例钝性肝脾损伤患者的临床资料,对其血清K+、Na+、ALT、AST水平进行了单独以及联合分析,以探讨血清K+、Na+联合肝转氨酶在钝性肝损伤中的临床应用价值。
资料与方法
1一般资料
回顾性分析202例钝性肝脾损伤患者的临床资料,纳入可以获得详细的临床资料且受伤后初次就诊笔者医院的患者,排除腹部穿透伤、经外院治疗后转入笔者医院、合并心脏病和肝脏疾病的患者及高血压长期服用利尿剂、服用受体药物、甲亢、醛固酮增多症等会引起低钾的基础疾病患者。通过上腹部CT扫描或手术中探查确定肝损伤及脾损伤的程度分级,Ⅰ级、Ⅱ级为轻度肝损伤,Ⅲ级、Ⅳ级、Ⅴ级为严重肝损伤。按是否存在肝损伤,并根据美国创伤外科学会-器官损伤分级(AAST-OIS)及影像学Becker分级,分为肝损伤组101例(包括Ⅰ级20例、Ⅱ级33例、Ⅲ级25例、Ⅳ级23例)和无肝损伤组101例(包括Ⅰ级14例、Ⅱ级17例,Ⅲ级31例、Ⅳ级39例),两组患者一般资料差异均无统计学意义(P>0.05)。见表1。按肝损伤程度分为轻度肝损伤组53例(包括Ⅰ级20例、Ⅱ级33例)和严重肝损伤组48例(包括 Ⅲ级25例、Ⅳ级23例),两组患者一般资料差异均无统计学意义(P>0.05)。见表2。患者均为急诊入院诊治,受伤至入院时间为0.5~3.0h,入院后急查肝功能、电解质。检验均采用日本全自动生化分析仪OLYMPUS AU2700检验仪器进行,试剂均由仪器厂家配套提供。
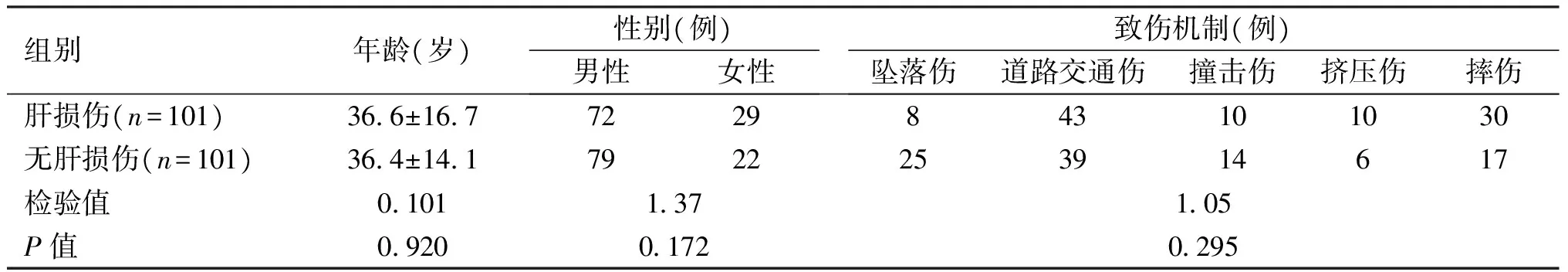
表1 肝损伤组和无肝损伤组一般资料比较
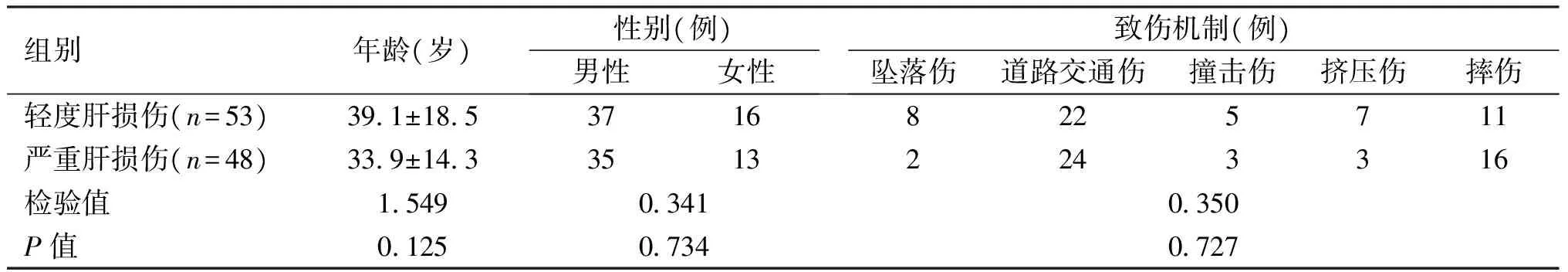
表2 轻度肝损伤组和严重肝损伤组一般资料比较
2统计学分析

结 果
1肝损伤与无肝损伤组的对比分析
肝损伤与无肝损伤组的血清K+、Na+、ALT、AST水平的差异均有统计学意义(P<0.05),表明肝损伤组较无肝损伤组, K+降低, Na+、ALT、AST均升高。见表3。
1.1肝损伤与无肝损伤组血清K+、Na+、ALT、AST水平的Logistic回归分析 经Logistic逐步回归分析,筛选出有意义的变量为ALT,得到Logistic回归模型:P(ALT)=1/[1+exp(4.031-0.056X1)]。见表4。强制选入Logistic回归法计算出回归模型:P(ALT+AST+Na++K+) =1/[1+exp(26.128-0.053X1-0.006X4-0.142X2-0.502X3)];P(ALT+AST) =1/[1+exp(4.157-0.051X1-0.006X4)];P(ALT+AST+Na+) =1/[1+exp(20.780-0.052X1-0.006X4-0.118X2)];P(ALT+AST+K+) =1/[1+exp(4.222-0.051X1-0.006X4-0.016X3)],X1=ALT,X2=Na+, X3=K+,X4=AST。结果表明:无论是ALT单独还是联合检测对肝损伤和无肝损伤均有很高的预测率。且经Logistic逐步回归筛选的ALT与强制选入Logistic回归的ALT、AST、Na+、K+联合预测肝损伤和无肝损伤的概率相等(89.1%,94.1%)。见表5。
1.2肝损伤与无肝损伤组ROC曲线
通过ROC曲线评估,ALT、AST在肝损伤中最佳阈值分别为57.55U/L、59.20U/L。图1的ROC曲线显示肝损伤与非肝损伤组指标检测的准确性、敏感度和特异度。结果显示:单独检测两个指标时,ALT的AUC最大(0.966),且敏感度和特异度均较高(93.1%,92.1%)。联合检测时,经Logsitic逐步回归筛选的ALT与强制选入Logistic回归的ALT、AST、Na+、K+联合的ACU差异无统计学意义(P>0.05),敏感度相同(93.1%,93.1%),特异度大致相同(92.1%,93.1%)。其他联合的AUC与单独ALT检测的AUC差异无统计学意义(P>0.05)。见表6。综上表明:无论是单独还是联合检测对判断肝损伤均有很高的准确性、预测性、敏感度和特异度,这也提示肝转氨酶是判断肝损伤非常敏感的指标。
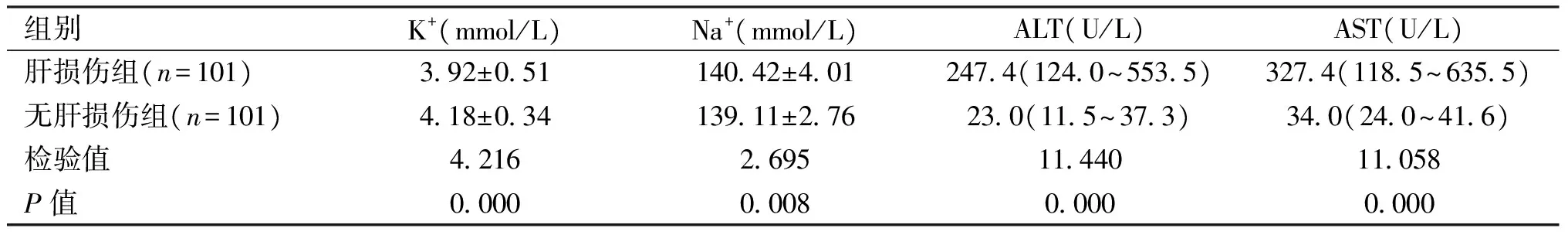
表3 肝损伤和无肝损伤组各指标的比较

表4 4个指标经Logistic回归分析结果
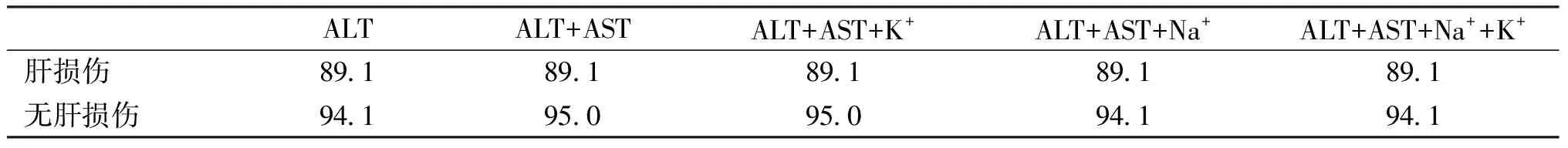
表5 经Logistic回归模型分析的预测概率(%)
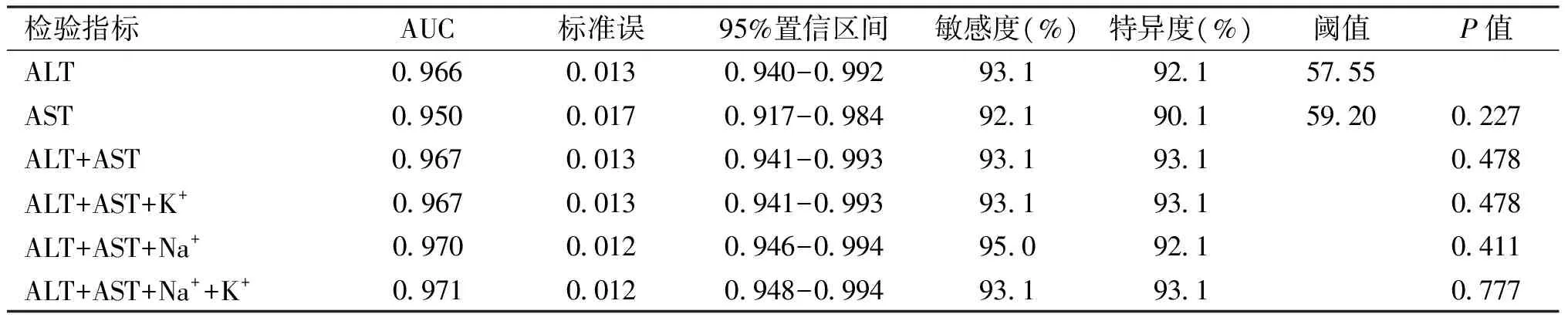
表6 肝损伤与无肝损伤组的AUC
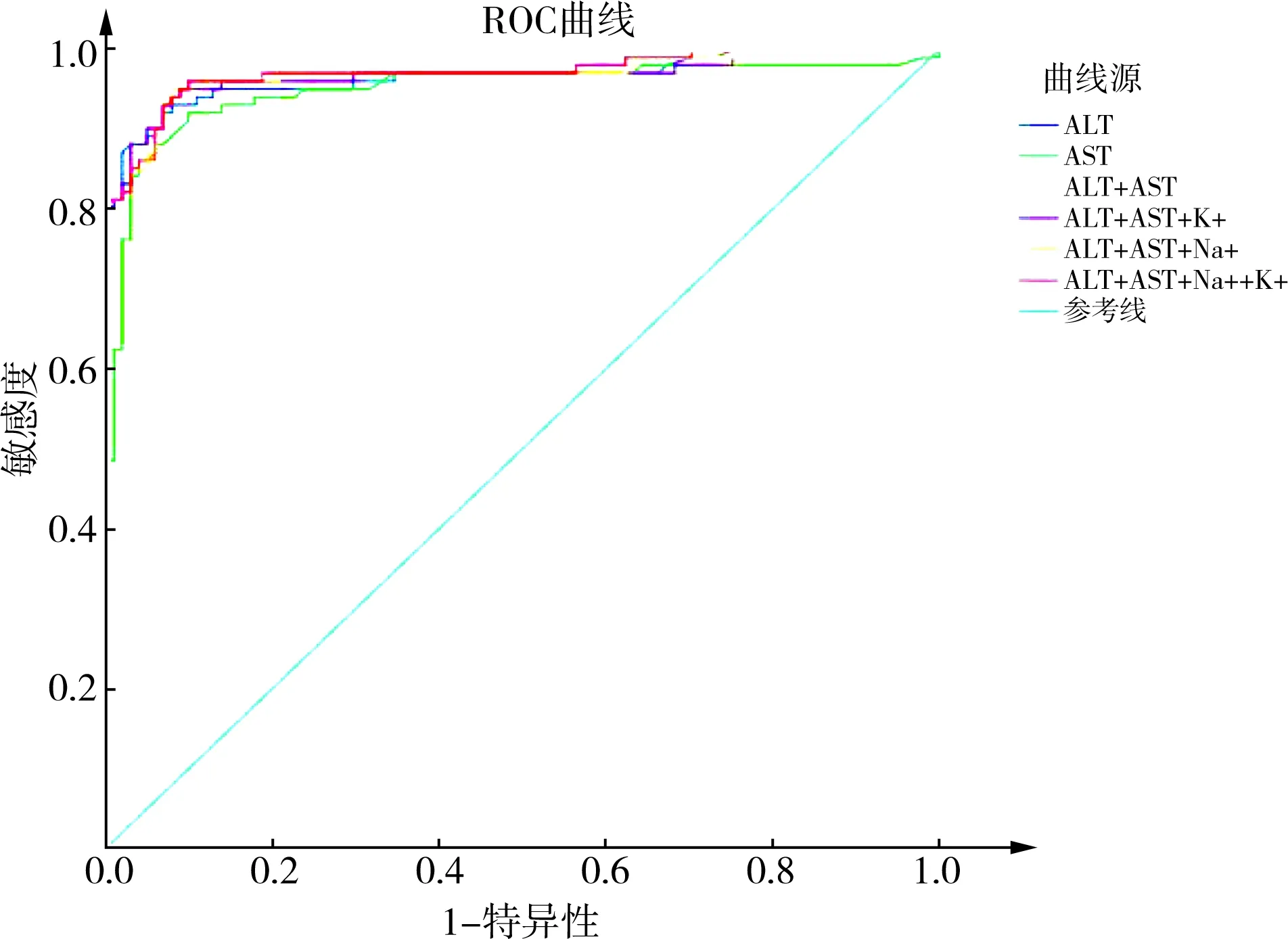
图1 肝损伤与非肝损伤组的ROC曲线
2轻度与严重肝损伤组的对比分析
轻度与严重肝损伤组的血清K+、Na+、ALT、AST水平的差异均有统计学意义(P<0.05),表明严重肝损伤较轻度肝损伤,K+降低, Na+、ALT、AST均升高。见表7。
2.1轻度与严重肝损伤组血清K+、Na+、ALT、AST的Logistic回归分析 经Logsitic逐步回归分析,筛选出有意义的变量为ALT、Na+和K+,得到Logistic回归模型:P(ALT+Na++K+) =1/[1+exp(30.678-0.003X1-0,25X2+1.44X3)]。见表8。强制选入Logistic回归法计算出回归模型:P(ALT+AST+Na++K+) =1/[1+exp(30.655-0.003X1-0,25X2+1.44X3-0.001X4)];P(ALT+AST+K+) =1/[1+exp(-6.994-0.002X1-0.001X4+2.073X3)];P(ALT+AST+Na+) =1/[1+exp(44.890-0.003X1-0.001X4-0.310X2)];P(AST+Na++K+) =1/[1+exp(27.302-0.002X4-0.223X2+1,272X3)]。见表9。X1=ALT,X2= Na+,X3= K+,X4=AST。结果表明:联合比单独检测对轻度和严重肝损伤的预测率高,且预测严重肝损伤的概率明显提高。见表10。
2.2轻度与严重肝损伤组血清K+、Na+、ALT、AST的ROC曲线 通过ROC曲线评估,血清K+、Na+、ALT、AST在严重肝损伤中最佳阈值分别为3.67mmol/L、142.55 mmol/L、171.50U/L、364.00U/L。图2的ROC曲线显示轻度与严重肝损伤组指标检测的准确性、敏感度和特异度。结果显示:单独检测时,ALT的AUC为0.735,特异度较低(54.70%)。联合检测时,Logistic逐步回归筛选的ALT、Na+、K+联合与强制选入Logistic回归ALT、AST、Na+、K+联合的AUC相等,均为0.844,且敏感度和特异度相等均较高(66.70%,94.30%)。ALT、AST、Na+、K+和ALT、Na+、K+联合的AUC与ALT单独检测的AUC差异有统计学意义(P=0.043);其他三项指标联合的AUC与ALT单独检测的AUC差异无统计学意义(P>0.05),但特异度均明显提高。见表11。综上表明:联合检测对严重肝损伤的诊断有较高的准确性、预测性和特异度。其中以ALT、Na+、K+或ALT、AST、Na+、K+联合检测的准确性、预测性和特异度最高。
3Pearson积差相关系数分析
血清K+和Na+的水平在轻度和严重肝损伤组呈负相关(P=0.005,r=-0.382;P=0.001,r=-0.494),也可以看出这种负相关在轻度肝损伤中为弱相关;在严重肝损伤中为中等程度相关。见表12。
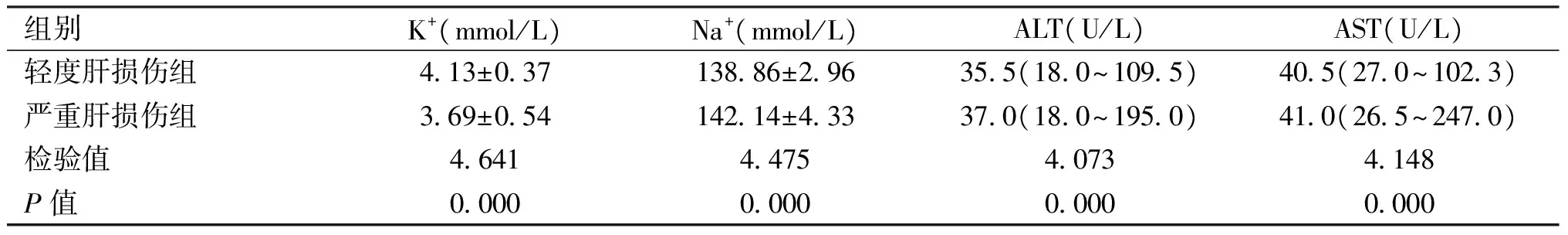
表7 轻度和严重肝损伤组各指标的比较
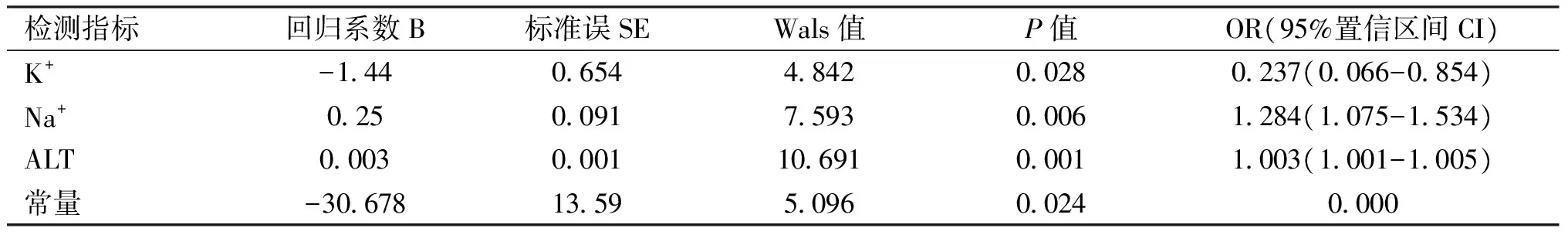
表8 4个检测指标经逐步Logistic回归分析结果
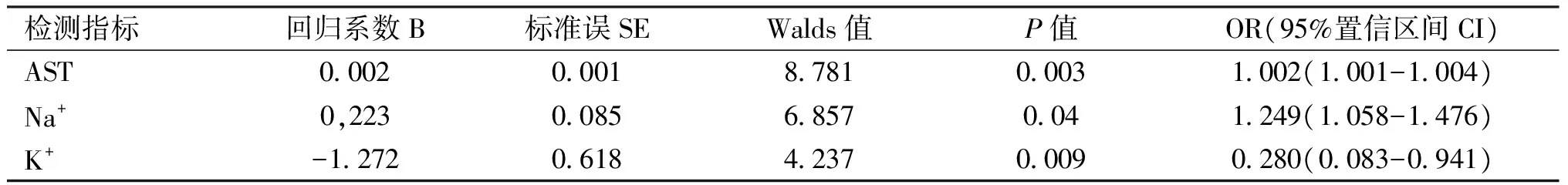
表9 3个检测指标经逐步Logistic回归分析结果
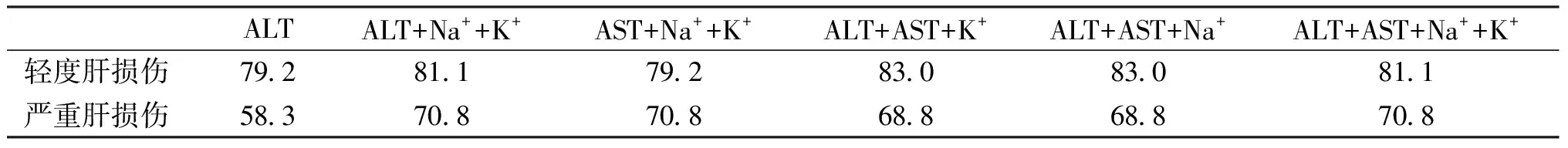
表10 经Logistic回归模型分析的预测概率(%)
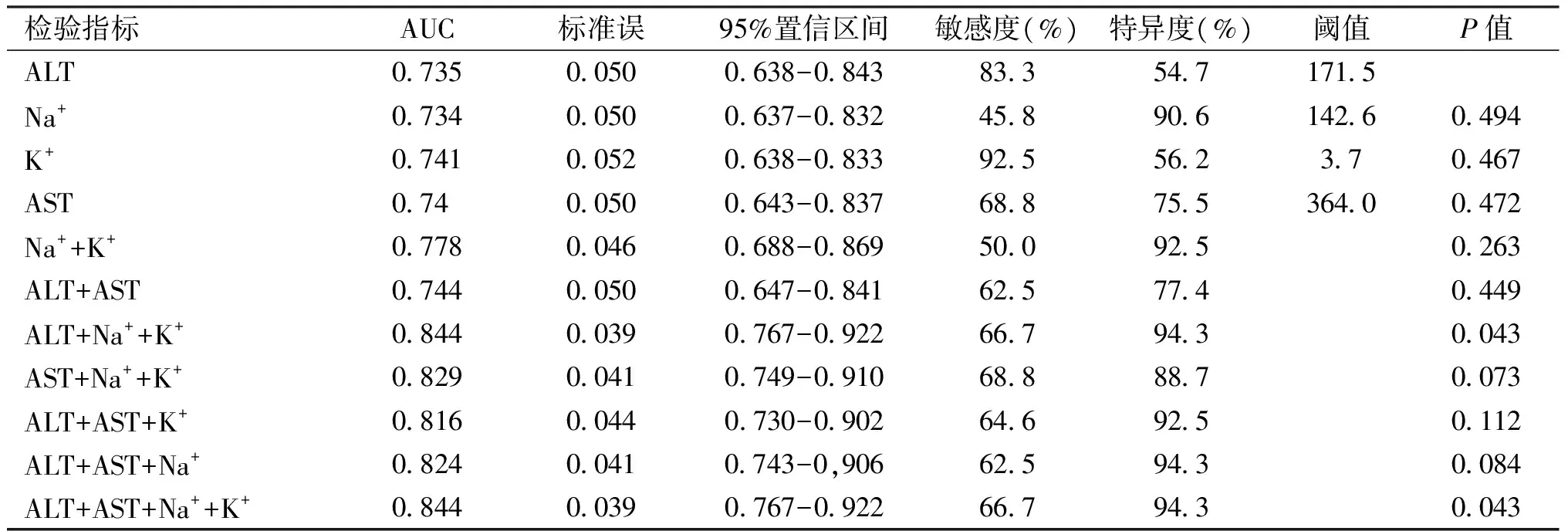
表11 轻度与严重肝损伤组的AUC
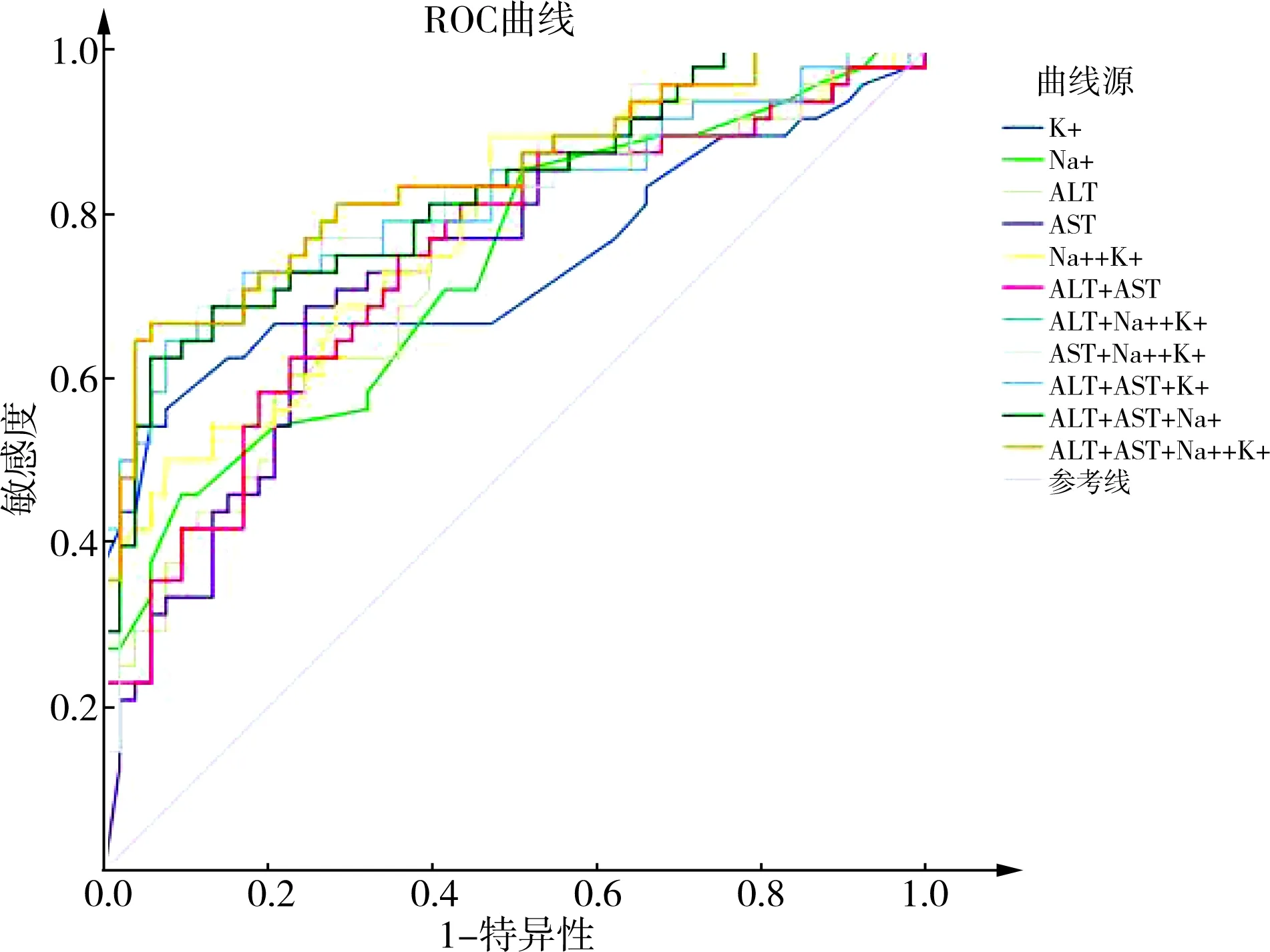
图2 轻度与严重肝损伤组的ROC曲线
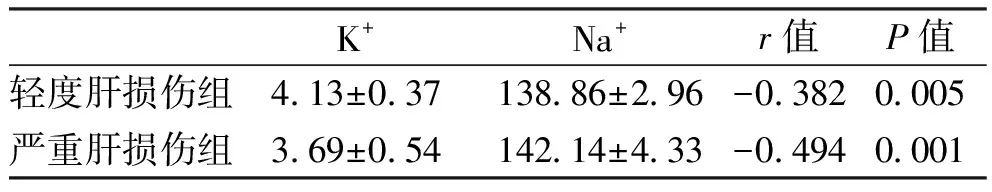
K+Na+r值P值轻度肝损伤组413±03713886±296-03820005严重肝损伤组369±05414214±433-04940001
讨 论
肝脏作为人体最大的实质性脏器,是闭合性腹部损伤中常见的损伤器官,钝性肝损伤的处理常常通过影像学检查和生化检验帮助临床评估。最常用的影像学检查包括CT扫描和超声,但其均有自身的限制和不足。CT扫描需搬动患者、接触辐射、费用高、消耗时间长,而且仅适用于血流动力学稳定者。FAST受操作者的技术经验和肝损伤程度的限制,尤其是对肝实质损伤而无腹腔积血患者的诊断。
Tan等[9]证明肝转氨酶升高与肝损伤强烈相关,且ALT水平高于正常2倍提示严重肝损伤,ALT、AST、LDH正常提示不可能为严重的肝损伤。Lee等[10]研究发现,在闭合性腹部损伤的患者中,若AST>100IU/L、 ALT>80IU/L和WBC计数>10 000/mm3,则强烈提示肝脏破裂,敏感度和特异度分别为90.0%、92.3%。Karaduman等[11]研究发现, AST突然上升至110.5U/L和ALT上升至63.5U/L,表明腹腔内脏器损伤;伴随更高水平的AST和ALT应该怀疑为严重肝损伤。Srivastava等[6]采用观察性队列研究,强烈地认为血清ALT的升高是诊断钝性肝损伤的一个敏感指标以及其升高的水平可以帮助判断预后和指导治疗。Stassen等[12]研究表明,患者入院时AST水平>360U/L和FAST阴性,有88%的概率是任何程度的肝损伤,有44%的概率是严重肝损伤;AST水平<360U/L和FAST阴性,只有14%的概率有肝损伤,没有概率是严重肝损伤;当对比AST>360U/L组和AST<360U/L组时发现AST水平>360U/L组为严重肝损伤的概率增加;入院时AST水平>360U/L的患者诊断为严重肝损伤的敏感度为100%,特异度为75%。Tian等[13]研究表明,在腹部钝性肝损伤患者中,异常的转氨酶水平与肝损伤相关,ALT>57U/L和AST>113U/L与肝损伤强烈相关。Seeto等[7]研究表明,单独的全身性低血压或休克不会导致缺血性肝炎,绝大多数患者的缺血性肝炎有严重的潜在心脏疾病,而心脏疾病常常导致肝脏的被动充血。伴随肝静脉充血的右心衰竭,通过低血压引起的肝损伤。本研究表明肝转氨酶与肝损伤密切相关,当ALT水平>57.55U/L、AST水平>59.20U/L则提示肝损伤;在钝性肝损伤中,若ALT水平>171.50U/L、AST水平>364.00U/L则提示严重肝损伤。
夏锋等[14]用Sevier-M unger改良法染色切片发现人与大鼠肝脏内分布有丰富的神经纤维,汇管区内的神经纤维分布与大鼠相似,且肝小叶内的神经分布较大鼠密集。Stoyanova[15]证明肝小叶和汇管区有大量的自主神经纤维。交感神经是其主要神经,主要分布于汇管区血管周围。Gardemann等[16]采用儿茶酚胺合成相关酶的抗体与神经元特异性烯醇化酶(neurorrspecificrendolase,NSE)得出60%的肝实质由无髓鞘轴索供应,供应脉管系统的神经纤维为交感神经;证实门静脉及肝动脉分支周围分布大量的肾上腺素能神经纤维。Miyazawa等[17]采用NSE的抗体及抗S-100蛋白证实了肝窦内神经纤维中分布肾上腺素能神经。机体创伤后低血钾的发生率较高,在严重创伤的患者中尤为明显,Meriggi等[8]根据文献的记载证实了钝性肝损伤的患者血清钾的水平可能显著性降低,且肝损伤越严重,低钾越显著。Pampolini等[18]研究表明,在钝性腹部损伤中,低血钾仅发生于肝损伤,其他脏器的损伤则不会出现低血钾。Beal等[19]研究表明,低血钾易发生于肝损伤。他们均认为人体存在一个促进钾转入细胞内的假说,尤其是在肝脏这个丰富神经纤维支配及富含神经纤维的脏器[14-17],肝脏一旦损伤,会立即刺激肝内的肾上腺素纤维,进而引起肾上腺素的释放,最后激活肾上腺受体,通过直接(β肾上腺能的激活通过cAMP机制激活Na+-K+泵)或间接(肝糖原分解-血糖升高-胰岛素分泌增加-激活Na+-K+-ATP酶)的途径以激活Na+-K+-ATP酶,Na+-K+-ATP酶的激活导致Na+-K+交换,即血清K+由细胞外转入细胞内及血清Na+由细胞内转出细胞外引起血清K+的降低和血清Na+的升高[8、18-22]。有研究表明[22]收缩期血压<96.5mmHg、血清K+<3.625mmol/L、合并腹腔其他脏器损伤、腹膜刺激征为钝性肝损伤手术治疗的高危因素。本研究表明在钝性肝损伤患者中,如果血清K+<3.685mmol/L、血清Na+>142.55mmol/ L,则提示严重肝损伤;通过血清钾和钠水平相关性分析得出两者为负相关,且在严重肝损伤中为中等程度相关,即证明了人体确实存在这一Na+-K+-ATP酶的假说;同时也表明了这种负相关在严重肝损伤中尤为明显。
经过一系列的分析,本研究发现,对于判断钝性腹部损伤是否合并肝损伤,不论从判断的准确性,预测是否肝损伤的概率还是判断肝损伤的敏感度和特异度,联合较单独检测基本无差异,所以无论是单独还是联合检测判断肝损伤均有很高的准确性、预测性、敏感度和特异度,也提示肝转氨酶是判断肝损伤非常敏感的指标。对于判断钝性肝损伤是否为严重肝损伤,不论从判断的准确性预测损伤程度的概率还是判断严重肝损伤的特异度,联合较单独检测均有所提高,所以血清K+、Na+联合肝转氨酶检测对严重肝损伤的诊断有较高的准确性、预测性和特异度,可作为临床上早期诊断及治疗的初步参考依据之一。
[1] Sikhondze WL,Madiba TE,Naidoo NM,et al.Predictors of outcome in patients requiring surgery for liver trauma[J].Injury,2007,38(1):65-70.
[2] Tang J,Li W,Lv F,et al.Comparison of gray-scale contrast-enhanced ultrasonography with contrast-enhanced computed tomography in different grading of blunt hepatic and splenic trauma: an animal experiment[J].Ultrasound Med Biol,2009,35(4):566-575.
[3] Smith J.Focused assessment with sonography in trauma (FAST):should its role be reconsidered[J].Postgrad Med J,2010,86(1015):285-291.
[4] Rothrock SG,Green SM,Morgan R.Abdominal trauma in infants and children: prompt identification and early management of serious and life-threatening injuries.Part I: injury patterns and initial assessment[J].Pediatr Emerg Care,2000,16(2):106-115.
[5] Kreimeyer S,Grenacher L.Modern imaging techniques for liver trauma[J].Chirurg,2009,80(10):896-907.
[6] Srivastava AR,Kumar S,Agarwal GG,et al.Blunt abdominal injury: serum ALT-a marker of liver injury and a guide to assessment of its severity[J].Injury,2007,38(9):1069-1074.
[7] Seeto RK,Fenn B,Rockey DC.Ischemic hepatitis: clinical presentation and pathogenesis[J].Am J Med,2000,109(2):109-113.
[8] Meriggi F,Gramigna P,Tramelli P.About usefulness of kalemia monitoring after blunt liver trauma[J].HPB Surg,2012,2012:279708.
[9] Tan KK,Bang SL,Vijayan A,et al.Hepatic enzymes have a role in the diagnosis of hepatic injury after blunt abdominal trauma[J].Injury,2009,40(9):978-983.
[10] Lee WC,Kuo LC,Cheng YC,et al.Combination of white blood cell count with liver enzymes in the diagnosis of blunt liver laceration[J].Am J Emerg Med,2010,28(9):1024-1029.
[11] Karaduman D,Sarioglu-Buke A,Kilic I,et al.The role of elevated liver transaminase levels in children with blunt abdominal trauma[J].Injury,2003,34(4):249-252.
[12] Stassen NA,Lukan JK,Carrillo H,et al.Examination of the role of abdominal computed tomography in the evaluation of victims of trauma with increased aspartate aminotransferase in the era of focused abdominal sonography for trauma[J].Surgery,2002,132(4):642-647.
[13] Tian Z,Liu H,Su X,et al.Role of elevated liver transaminase levels in the diagnosis of liver injury after blunt abdominal trauma[J].Exp Ther Med,2012,4(2):255-260.
[14] 夏锋,何振平,王晓丽,等.大鼠肝脏内神经分布的形态学观察[J].第三军医大学学报,2003,25(22):2025.
[15] Stoyanova II.Relevance of mast cells and hepatic lobule innervation to liver injury[J].Rom J Gastroenterol,2004,13(3):203-209.
[16] Gardemann A,Püschel GP,Jungermann K.Nervous control of liver metabolism and hemodynamics[J].Eur J Biochem,1992,207(2):399-411.
[17] Miyazawa Y,Fukuda Y,Imoto M,et al.Immunohistochemical studies on the distribution of nerve fibers in chronic liver diseases[J].Am J Gastroenterol,1988,83(10):1108-1114.
[18] Pampolini M,Cavallini G,Cavallesco G,et al.Different kalemia in abdominal trauma[J].J Trauma Acute Care Surg,1988,28(4):526-529.
[19] Beal AL,Scheltema KE,Beilman GJ,et al.Hypokalemia following trauma[J].Shock,2002,18(2):107-110.
[20] Zavagli G,Pampolini M,Cavallini G,et al.Different kalemia in abdominal trauma[J].J Trauma,1988,28(4):526-529.
[21] Beal AL,Deuser WE,Beilman GJ.A role for epinephrine in post-traumatic hypokalemia[J].Shock,2007,27(4):358-363.
[22] 黄超,张坤,江艺.闭合性肝损伤手术治疗危险因素102例分析[J].中国实用外科杂志,2016,36(12):1313-1317.
Clinicalvalueofserumpotassiumandsodiumcombinedhepatictransaminasesinthebluntliverinjury
HUANGChao,ZHANGKun,JIANGYi
(Department of Hepatobiliary Surgery,Fuzong Medical College of Fujian Medical University,Fuzhou General Hospital,Fuzhou 350025,China)
ObjectiveTo investigate the clinical application value of serum potassium and sodium combined hepatic transaminases in the blunt liver injury.MethodsClinical data of 202 patients with blunt liver and spleen injury admitted between Oct. 2003 and Apr. 2016 in the Fuzhou General Hospital were reviewed retrospectively.According to the presence or absence of liver injury,they were divided into liver injury group and non-liver injury group, with 101 cases in each group. In the liver injury group,53 cases of mild liver injury were taken as the mild liver injury group and 48 cases of severe liver injury were taken as the severe liver injury group. Values of serum potassium,sodium,alanine aminotransferase(ALT) and aspartate aminotransferase(AST) in the two groups were detected,and the regression model was established by Logistic regression to draw receiver operating characteristic curve to evaluate the diagnostic value of individual and joint detection indicators. The optimal threshold of ALT and AST in liver injury and serum potassium,sodium,ALT and AST in severe liver injury were determined by the ROC curve.ResultsFour metric levels were statistically significant(P<0.01) between non-liver injury group and liver injury group,and were statistically significant(P<0.01) between mild liver injury group and severe liver injury group. AUC of combined detection was greater than single detection for judging the presence or absence of liver injury in the blunt abdominal injury,but the difference was not statistically significant (P>0.05). Prediction rates of ALT alone and combined detection were 89.1% and 94.1% for the presence of liver injury, respectively,and sensitivity and specificity of ALT alone for determination of liver injury were 92.1% and 93.1%, respectively,but combined were 93.1% and 93.1%. AUC of combined detection was greater than single detection for judging the presence or absence of severe liver injury in the blunt liver injury and the difference was statistically significant (P=0.043),prediction rates of ALT alone detection were 79.2% and 58.3%, respectively,but combined were 81.1% and 70.8% for the mild liver injury and severe liver injury,and sensitivity and specificity of ALT alone for determination of liver injury were 83.3% and 54.7%, respectively,but combined were 66.7% and 94.3%.This study obtained that of the optimal threshold of ALT,AST in liver injury were 57.55U/L and 59.20U/L, respectively,and that the optimal threshold of serum potassium,sodium,ALT and AST of severe liver injury were 3.685mmol/L,142.55mmol/L,171.50U/L and 364.00U/L, respectively by the ROC curve assessment. Levels of serum potassium and sodium are negatively correlated in mild liver injury and severe liver injury(P=0.005,r=-0.382;P=0.001,r=-0.494),especially significant in severe liver injury.ConclusionIncreased liver transaminases are closely related to liver damage. Combined electrolytes detection of liver function for clinical identification of whether liver injury is severe has high accuracy,predictability and specificity in the blunt liver injury,which could be used as one of the initial effective means for early clinical judgment of whether blunt liver injury is severe,so as to provide strong evidence for its clinical treatment.
hepatic injury; serum potassium; serum sodium; transaminases
1009-4237(2017)12-0904-07
R 657.3
A
10.3969/j.issn.1009-4237.2017.12.007
南京军区医学科研重大专项基金资助(CNJ15J002;14ZX22)
350025 福州,福建医科大学福总临床医学院(南京军区福州总医院肝胆外科)
江艺,E-mail:jiangyi8183@163.com
2017-02-17;
2017-04-20)
郭 卫)
