中西医结合治疗与护理干预对妊娠期肝内胆汁淤积症疗效及相关血清学指标的影响
2017-09-16尹秀玲
尹秀玲
(菏泽市立医院,山东菏泽274031)
中西医结合治疗与护理干预对妊娠期肝内胆汁淤积症疗效及相关血清学指标的影响
尹秀玲
(菏泽市立医院,山东菏泽274031)
目的探讨中西医结合治疗与护理干预对妊娠期肝内胆汁淤积症肝功能、血流变学、凝血功能及炎性因子的影响。方法妊娠肝内胆汁淤积症96例,随机分为两组,对照组31例,观察组65例,两组一般资料比较,P>0.05。选择正常妊娠孕妇50例为正常对照组。对照组基本治疗加熊去氧胆酸,常规护理。观察组在对照组的基础上加用清热解毒、保肝利胆、活血化瘀中草药,日一剂,水煎服。两组均治疗两周。治疗前与治疗两周后抽取晨起静脉血检测肝功能、血流变学、凝血功能、D-二聚体、炎性因子等。应用SPSS20.0软件,所获数据采用方差分析、t检验和χ2检验。结果两组治疗前与正常对照组肝功能变化比较,P均>0.05;对照组治疗前后肝功能变化比较,P均<0.0005;观察组治疗前后肝功能变化比较,P均<0.0005;两组治疗前后肝功能变化比较,P均<0.0005。两组治疗前与正常对照组血流变学变化比较,P均<0.00005。两组治疗前血流变学变化比较,P均>0.05。对照组治疗前后全血黏度高切、红细胞压积、血沉变化比较,P均<0.00005;对照组治疗前后全血黏度低切变化比较,P>0.05;对照组治疗前后血浆黏度变化比较,P<0.05。观察组治疗前后血流变学变化比较,P均<0.0005。两组治疗后全血黏度高切、血浆黏度变化比较,P>0.05;两组治疗后全血黏度低切、红细胞压积变化比较,P均<0.01;两组治疗后血沉变化比较,P<0.005。两组治疗前与正常对照组凝血指标变化比较,P均<0.01~0.0005。两组治疗前凝血指标变化比较,P>0.05。对照组治疗前后PLT比较,P<0.0005;对照组治疗前后FIB比较,P<0.05;对照组治疗前后PT、APTT变化比较,P>0.05。观察组治疗前后PLT、FIB变化比较,P均<0.0005;观察组治疗前后PT变化比较,P<0.01;观察组治疗前后APTT变化比较,P<0.005。两组治疗后PLT变化比较,P<0.01;两组治疗后FIB、PT变化比较,P均<0.05;两组治疗后APTT变化比较,P>0.05。两组治疗前与正常对照组炎性因子及D-二聚体水平比较,P均<0.0005。两组治疗前炎性因子及D-二聚体水平比较,P>0.05。对照组治疗前后炎性因子及D-二聚体水平比较,P均<0.0005。观察组治疗前后炎性因子及D-二聚体水平比较,P均<0.0005。两组治疗后炎性因子水平比较,P<0.0005;两组治疗后D-二聚体水平比较,P<0.05。对照组痊愈4例,占12.90%;显效9例,占29.03%;总有效率77.42%。观察组痊愈20例,占30.77%;显效26例,占40.00%;总有效率98.46%。结论中西医结合治疗与护理干预妊娠肝内胆汁淤积症能更大程度的减轻症状和体征、保护胎儿降低早产率、窒息率、死亡率,对母婴无明显的副作用。
妊娠;肝内胆汁淤积症/治疗;肝内胆汁淤积症/护理;中西医结合疗法/治疗应用;血流变学;凝血功能;炎性因子
妊娠肝内胆汁淤积症是妊娠晚期的常见并发症之一,其临床表现有阻塞性黄疸的一般特征。严重影响母儿的健康,甚或胎儿死亡[1]。其病因尚不明确,可能与家族、雌二醇代谢相关。国人发生率2%~4%,首发症状是瘙痒、数日后出现黄疸,黄疸发生率国内报道15%~60%之间[2]。多数常合并肝炎。目前国内外尚无理想的治疗方案。为此,我们自2015年1月—2017年1月对妊娠期肝内胆汁淤积采用中西医结合与护理干预了解其血流变学、凝血功能及炎性因子的变化。现报道如下。
1 临床资料
1.1 一般资料妊娠肝内胆汁淤积症96例,年龄最小者21岁,最大年龄40岁,平均29.45岁;初产妇61例,经产妇25例;均为单胎。均符合诊断标准[3]。瘙痒出现时间最早26周,最晚35周,平均28.3周。病程最短1周,最长4周,平均2.5周。排出妊娠合并高血压、糖尿病、肝肾功能异常者、服用对凝血功能及血流变学有影响的药物者、不配合者、胎儿畸形等。随机分为两组。对照组31例,观察组65例。两组孕周、年龄、孕产次、体质指数、文化程度、经济水平,等一般资料比较,P>0.05,无显著性差异,具有可比性。另外,选择正常妊娠孕妇50例,最小年龄22岁,最大年龄39岁,平均年龄28.86岁;初产妇38例,经产妇12例;均有剖宫产指征;做正常对照组。所有患者知情同意,并经院伦理委员会批准。
1.2 方法(1)治疗:①对照组:吸氧、胎心监护、胎动监测、每周检测尿雌激素/肌酐比值(E/C);定期复查B超检测:羊水、胎儿宫内窘迫、不可控的宫缩、胎儿成熟度、孕周超过35周者及时结束妊娠,分娩前3天给予维生素K,静滴能量合剂、维生素C、辅酶A、三磷酸腺苷、低分子右旋糖酐、氟美松、腺苷蛋白酸等。口服巴比妥、熊去氧胆酸。②观察组:在上述治疗的基础上给予中草药:茵陈25 g、党参15 g、白术15 g、茯苓15 g、山药15 g、栀子15 g、黄芪20 g、黄芩10 g、当归15 g、丹参20 g、金钱草10 g、郁金10 g、泽泻10 g、甘草10 g、黄柏10 g、桑寄生10 g、苎麻根10 g等。日一剂水煎分两次服用。两组均治疗两周,治疗前与治疗两周后抽取晨起静脉血检测:肝功能、血流变学、凝血功能、D-二聚体、炎性因子等。(2)护理:①一般护理。②基础护理。③皮肤护理。④饮食护理。⑤心理护理,充分利用“同室效应”和“同伴群体论”的相关内容增加依从性。⑥胎儿监护。⑦新生儿和围产期护理。
1.3 统计学处理应用SPSS20.0软件,所获数据采用方差分析、t检验和χ2检验。
2 结果
2.1 两组治疗前后谷丙转氨酶(ALT)、谷草转氨酶(AST)、血清总胆红素(TBIL)、直接胆红素(DBIL)、血胆汁酸(TBA)变化比较见表1。
2.2 两组治疗前后血流变学变化与正常对照组比较见表2。
2.3 两组治疗前后血小板(PLT)、纤维蛋白原(FIB)、凝血酶原时间(PT)、部分凝血酶原时间(APTT)变化见表3。
2.4 两组治疗后IL-18、IL-12、TNF-α、及D-二聚体水平比较见表4。2.5两组疗效比较对照组痊愈4例,占12.90%;显效9例,占29.03%;有效11例,占35.48%;无效7例,占22.58%。总有效率77.42%。观察组痊愈20例,占30.77%;显效26例,占40.00%;有效18例,占27.69%,无效1例,占1.54%。总有效率98.46%。两组比较,χ2=9.5675,P<0.005。
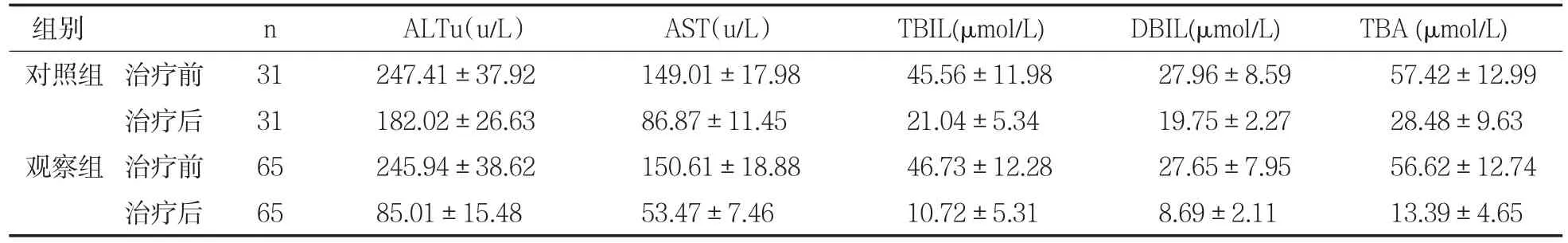
表1 两组治疗前后ALT、AST、STB、DBIL、TBA变化比较(x-±s)

表2 两组治疗前后全血流变学变化变化与正常对照组比较(x-±s)
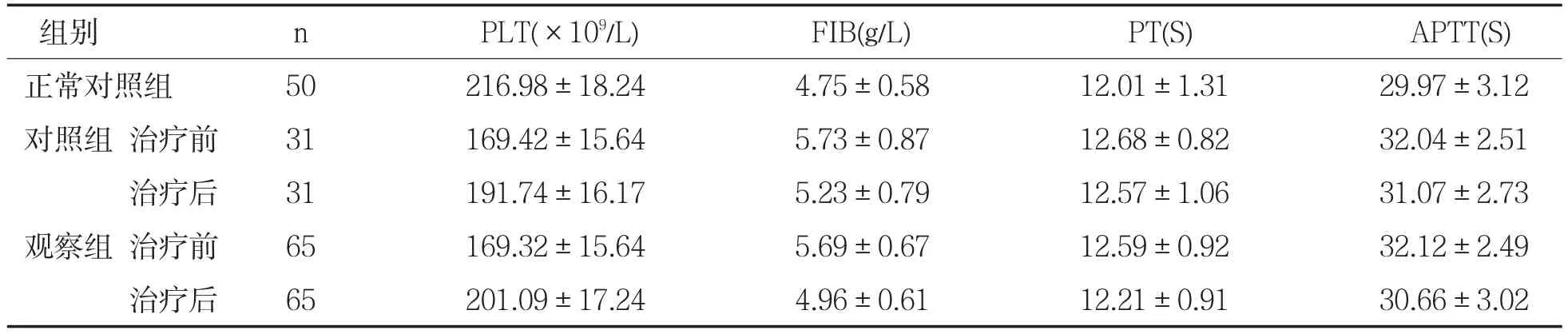
表3 两组治疗前后PLT、FIB、PT、APTT变化(x-±s)
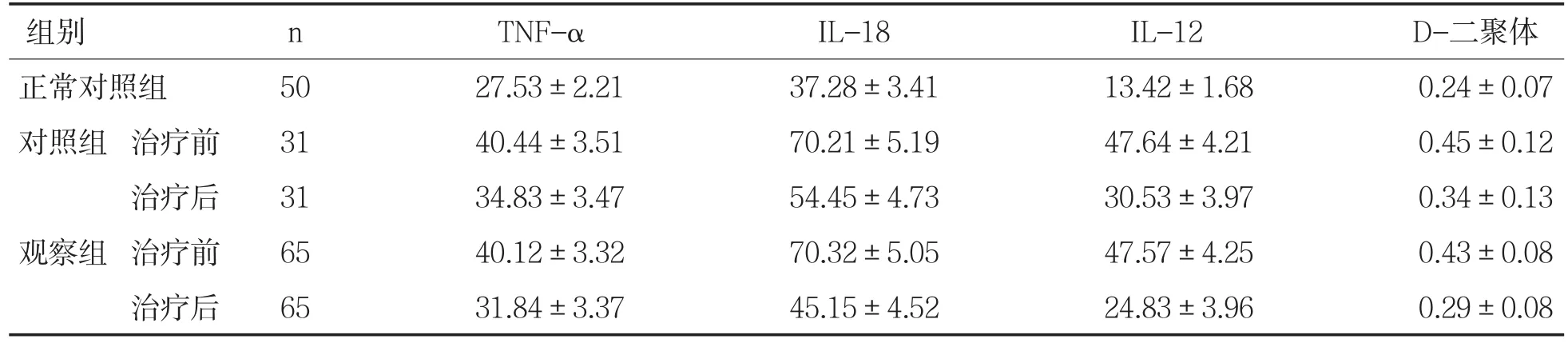
表4 两组治疗前后TNF-α、IL-18、IL-12及D-二聚体水平比较(ng/L,x-±s)
3 讨论
胎儿宫内死亡有50%是妊娠肝内胆汁淤积症所致[4]。妊娠肝内胆汁淤积症病因不明,可能与环境、遗传、雌二醇有关。雌二醇较密切,雌二醇可使肝细胞膜胆固醇和磷脂比例紊乱,流动性差、影响胆酸的通透性,胆汁排出障碍;血中胆红素增加,出现黄疸皮肤瘙痒,毛细血管通透性增加,胆汁水分回流到血液中,胆汁浓缩、黏稠、胆栓形成、胆汁淤积。母体胆汁酸升高,平滑肌收缩导致早产。维生素K吸收减少,凝血因子合成障碍,导致产后出血。
腺苷蛋氨酸促进肝细胞膜的流动性,具有促进肝细胞内合成半胱氨酸、谷胱甘肽、牛磺酸的作用,保护肝细胞,有助于缓解瘙痒、降低血中胆酸与转氨酶的浓度。熊去氧胆酸对肝有多重保护作用,防止疏水酸对胆管细胞的损伤,降低胆汁酸的毒性;促进肝内胆管的分泌;免受肝细胞对胆汁酸所致的死(凋)亡[5]。
妊娠肝内胆汁淤积症系祖国医学的黄疸、子黄、胎毒等范畴,以目赤黄染为特征,是内外因所致的湿浊,胆液不循规,外溢肌肤而身黄。上输目、下注膀胱出现目尿黄。按照湿热分行,速从二便排出。方中茵陈清利湿热、退黄;栀子泻胆;黄芩清热燥湿、安胎;大黄清热解毒、泻黄;金钱草利水退黄;党参、白术、茯苓、甘草利湿健脾;黄芪、山药健脾益气;当归、丹参活血化瘀,疏通微循环[6];郁金、泽泻疏肝利湿、利胆;黄柏消炎利黄疸;桑寄生益血、安胎、止腰膝酸痛;苎麻根活血、止血、安胎。诸药和用健脾养血、活血化瘀、泻补兼备。共奏利湿热、疏肝脾、养活血、安稳胎之功。
妊娠肝内胆汁淤积症患者的护理工作是不可或缺的,一般护理、基础护理、母儿监护、饮食护理、皮肤护理、分娩护理、新生儿护理、产褥期护理较为常规[7]。我们重点加强了心理护理,充分利用“同室效应”和“同伴群体论”[8]的相关方法,对每位患者进行多次、多医护人员的相关知识教育。
妊娠肝内胆汁淤积症采用中药口服比单用西药效果好。观察组总有效率98.46%。对照组总有效率77.42%。两组比较,P<0.005,有非常显著性差异。症状改善,两组比较也有显著性差异。
两组治疗前与正常对照组肝功能变化比较,P均>0.05;对照组治疗前后肝功能变化比较,P均<0.0005,有非常显著性差异,说明胆汁淤积后肝功发生率较大的变化。观察组治疗前后肝功能变化比较,P均<0.0005;两组治疗前后肝功能化比较,P均<0.0005,均有非常显著性差异,服用中药组肝功改善效果更好,与文献报道一致[9]。
两组治疗前与正常对照组血流变学变化比较,P均<0.00005,有非常显著性差异,说明胆汁淤积后血液的黏度明显增加。两组治疗前后血流变学均有明显的改善,对照组全血黏度高切、红细胞压积、血沉变化比较,P均<0.0005,有非常显著性差异;但全血黏度低切变化比较,P>0.05,无显著性差异;血浆黏度变化比较,P<0.05,有显著性差异。而观察组治疗前后血流变学变化比较,P均<0.0005,均有非常显著性差异,说明中药活血化瘀效果显著[10]。
两组治疗前与正常对照组凝血指标变化比较,P均<0.01~0.0005,具有显著性差异,说明患病后均有不同程度的凝血机制障碍。通过治疗两组均有不同程度的改善,口服中药效果更好。
两组治疗前与正常对照组炎性因子及D-二聚体水平比较,P均<0.0005,有非常显著性差异,说明患病后炎性因子和D-二聚体均有明显的变化。通过治疗两组均有一定程度的改善。对照组治疗前后炎性因子及D-二聚体水平比较,P均<0.0005,有非常显著性差异。观察组治疗前后炎性因子及D-二聚体水平比较,P均<0.0005,有非常显著性差异。两组治疗后炎性因子水平比较,P<0.0005,有非常显著性差异,与文献报道一致[11];两组治疗后D-二聚体水平比较,P<0.05,有显著性差异。
从结果可以看出中西医结合治疗和护理干预对妊娠肝内胆汁淤积症是目前较为有效的办法,改善孕产妇的症状和体征,减轻了痛苦,保护了胎儿、降低了早产的发生、降低了新生儿窒息及死亡率。且对母婴均无明显的不良反应。适合于各级各类医院推广。
[1]薛清秀.86例妊娠期肝内胆汁淤积与围生儿与预后相关因素分析[J].中国现代医生,2010,48(3):125-126.
[2]李杰.自拟利胆退黄汤治疗妊娠肝内胆汁淤积症临床疗效观察[J].中华中医药学刊,2015,33(11):2807-2811.
[3]罗杰.妇产科学[M].第7版,北京:人民卫生出版社,2008:52-56.
[4]Burrows RF,Clavisi O,Burrows E.lntervetion for treating cholestasis pregnancy[J].Cochrane Database Syst Rev,2001,(4):493-501.
[5]赵敏,于月成,吴维光,等.S腺苷蛋氨酸促联合熊去氧胆酸治疗妊娠肝内胆汁淤积症疗效观察[J].第四军医大学学报,2006,27(3): 258-260
[6]姚祝玲,王彩月.复方丹参治疗妊娠肝内胆汁淤积综合征的观察和护理[J].求医问药,2010,10(7):160.
[7]季晔.妊娠肝内胆汁淤积症患者的护理[J].医疗装备,2016,29(17):200-201.
[8]许国峰,姜桂娥.外来务工人员强化培训前后艾滋病相关知识教育评价研究[J].菏泽医学专科学校学报,2016,28(1):78-84.
[9]陈友英,陈宣伊,梁国强.茵陈加味汤联合熊去氧胆酸治疗妊娠肝内胆汁淤积症62例[J].东南大学学报(医学版),2014,33(2): 159-161.
[10]张莉,李晓丽,兰远霞.妊娠肝内胆汁淤积症孕妇血流变学、凝血功能和细胞因子的变化及临床意义[J].海南医学院学报,2015, 21(8):1088-1090.
[11]方彩云,方孝梅,梁江红.妊娠肝内胆汁淤积症护着血清TNF-α检测的意义[J].中国妇幼健康研究,2008,19(1):79-80.
The Effects of Combination Therapy and Nursing Intervention on the Liver Function and the Influence of Related Serological Indexes
Yin Xiuling
(Heze Municipal Hospital,Heze 274031,Shandong)
Pregnancy;Intrahepatic cholestasis of pregnancy/therapy;Intrahepatic cholestasis of pregnancy/nursing; Chinese and western medicine combination therapy/therapeutic sue;Hemorrheology;Blood coagulation function;Inflam⁃matory cytokines
R446.11;R473.71
A
1008-4118(2017)03-0080-05
2017-07-05
10.3969/j.issn.1008-4118.2017.03.025
Abstract:Objective To discuss the cooperation of Chinese and western medicine therapy and nursing interven⁃tion of gestation intrahepatic cholestasis disease of liver function,hemorrheology and coagulation function and inflammato⁃ry factor influence.Methods96 cases were randomly divided into two groups,compared to the control group,the con⁃trol group was 65,and the comparison of the two groups was P>0.05.In addition,50 cases of normal pregnant women were chosen as normal control group.The control group treated the bear deoxycholic acid.Routine nursing.The observa⁃tion group,based on the control group,was used to detoxify,hepatobiliary,and blood stasis,and a daily dose of water de⁃coction.Both groups were treated for two weeks.After two weeks before the treatment,the blood tests were taken:liver function,blood rheology,coagulant function,d-dimer,inflammatory factor,etc.Using SPSS20.0 software,the data ob⁃tained using variance analysis,t test and χ2test.Results Compared with normal control liver function,P averaged>0.05.The comparison of liver function in the control group was<0.0005.The comparison of liver function before and af⁃ter treatment was observed,and P was<0.0005.Both groups were compared before and after treatment,and the P was<0.0005.Compared with the normal control group,the P was<0.00005.The two groups were compared to the changes in blood rheology,and the P was>0.05.In the control group,the ratio of full-blood viscosity,erythrocyte and hematogenous changes were compared,and P was<0.00005.The control group was treated with a lower and lower blood viscosity change compared to P>0.05.The comparison of plasma viscosity changes in the control group was P<0.05.The compari⁃son of blood rheological changes before and after treatment was<0.0005.The two groups were treated with high blood viscosity and plasma viscosity changes,and P>0.05.The two groups were compared with the lower blood viscosity and the variation of red blood cell pressure.The comparison of the two groups of treatments was compared with the comparison of the two groups with the normal control group of the control group,which was<0.01~0.0005.The comparison of the two groups of precurable blood markers was P>0.05.The control group compared the PLT before and after treatment,P<0.0005.The control group was treated before and after the FIB comparison,P<0.05.The control group treatment was com⁃pared to PT and APTT,P>0.05.Before and after group therapy,the PLT and FIB changes were compared,and P was<0.0005.The comparison of the PT changes before and after treatment was observed,P<0.01.The APTT comparison was observed before and after treatment,and P<0.005.After two groups of treatment,PLT changes compared to P<0.01.After two groups of treatment,FIB and PT were compared with P<0.05.After treatment,APTT was compared,P>0.05.Both groups were compared with normal control inflammatory factors and d-dimer levels,and P was<0.0005.The two groups were compared to the preinflammatory factor and the d-dimer level,P>0.05.The comparison of inflammatory factors and d-dimer levels in the control group was<0.0005.The comparison of the inflammatory factors and the level of d-dimer was observed in the observation group,P<0.0005.The levels of inflammatory factors were compared after two groups of treatment,P<0.0005.The two groups were compared with the d-dimer,P<0.05.The control group recovered 4 cases,ac⁃counting for 12.90 percent.In 9 cases,29.03%.Total efficiency 77.42%.The observation group recovered 20 cases,ac⁃counting for 30.77%.In 26 cases,40.00%.Total efficiency 98.46%.Conclusion Combine traditional Chinese and west⁃ern medicine therapy and nursing intervention in intrahepatic cholestasis of pregnancy disease can reduce the signs and symptoms,greater protection of fetus to reduce the rate of premature birth,asphyxia rate,mortality rate,the maternal and infant has no obvious side effects.
