单侧与双侧入路行椎体后凸成形术的效果比较
2017-09-06宋爱国倪文卓岳立群
胡 波,宋爱国,倪文卓,岳立群
·短篇论著·
单侧与双侧入路行椎体后凸成形术的效果比较
胡 波,宋爱国,倪文卓,岳立群
目的 对比单侧入路与双侧入路行经皮球囊扩张椎体后凸成形术(PKP)治疗胸腰椎骨质疏松性骨折的疗效。方法 回顾性统计北京水利医院2011年6月~2015年10月收治的69例胸腰椎骨质疏松性骨折,其中男性19例,女性50例,年龄52~91岁,平均 66.7岁。采用单侧入路或双侧入路行PKP治疗,记录骨水泥用量、手术时间、VAS评分、Cobb角变化度、椎体高度压缩率、恢复率等指标,术后随访时间1个月。结果 单侧入路组的手术时间为(28.6±6.4)min,显著优于双侧入路组的(40.1±9.6)min(P<0.05)。两组的骨水泥用量分别为(4.2±1.7)mL和(4.5±2.0)mL无统计学差异(P>0.05)。两组的术前Cobb角分别为(19.5±7.9)°和(21.1±9.1)°,术后分别为(11.6±5.5)°和(12.2±5.8)°,两组术后Cobb角均较术前有明显改善(P<0.05),但两组间无显著统计学差异。两组术前椎体高度压缩率分别为(31.7±11.6)%和(34.2±15.1)%,术后分别为(12.4±5.7)%和(12.8±4.9)%,术后椎体高度较术前均有明显恢复(P<0.05),恢复率分别为(60.9±20.1)%和(62.6±22.4)%,两组间无显著统计学差异。两组VAS评分,术前分别为(7.65±1.91)和(7.82±1.75),术后即刻分别为(3.88±1.12)和(4.03±1.02),术后1d分别为(2.36±0.49)和(2.34±0.53),术后3d分别为(1.48±0.33)和(1.41±0.41),术后1月分别为(0.12±0.05)和(0.19±0.06)。术后较术前疼痛均有明显缓解(P<0.05),但两组间无显著统计学差异。结论 单、双侧入路椎体后凸成形术治疗胸腰椎骨质疏松性骨折,均能达到满意疗效,若采用C型臂X线机透视,单侧入路手术时间更短。
骨质疏松性骨折; 胸腰椎; 单侧入路; 双侧入路; 椎体后凸成形术
自1987年法国Galibert等[1]首次报道采用经皮椎体成形术(PVP)治疗椎体血管瘤以来,PVP以及在此基础上发展起来的经皮球囊扩张椎体后凸成形术(PKP)[2],近年来已经逐渐成为骨质疏松性椎体压缩骨折的首选治疗方法。但术中是经单侧还是经双侧椎弓根灌注骨水泥,专家学者们对此尚存在争议[3-6]。
笔者回顾性分析了北京水利医院2011年6月~2015年10月收治的69例骨质疏松性胸腰椎压缩骨折患者(为排除多椎体之间的相互干扰,入组条件为单椎体骨折,术后随访满1个月),采用PKP手术治疗,单侧或双侧入路经椎弓根灌注骨水泥,均取得满意疗效,现报道如下。
临床资料
1 一般资料
69例患者(69个椎体),男性19例,女性50例;年龄52~91岁,平均66.7岁。病程1~89d(2例曾先采取非手术治疗,疼痛无缓解,诊断为Kümmell病,分别于伤后46d和89d入院,术后疼痛症状明显缓解。其余患者均在伤后1周内完成手术)。跌倒致伤46例,无明显外伤患者23例(多在咳嗽、提物、弯腰或起床后出现症状)。骨折类型中,未累及终板的(Denis分型ⅠD型)47例,累及一侧终板的(ⅠB或ⅠC型)17例,累及双侧终板的(ⅠA型)3例,后壁不完整的(Ⅱ型)有2例。椎体高度压缩不超过1/3者37个椎体,在1/3~2/3者32个椎体,伤椎分布范围:T6~L5。所有患者均有明显伤椎区域疼痛症状,所有病例均行X线片、CT及MRI检查,以确定“责任椎体”。
2 分组与方法
分组:查阅患者手术记录,根据采用的入路方式分为两组,行单侧入路的55个椎体,双侧入路的14个椎体。
透视方式:术中C型臂X线机透视。由专职熟练技师完成。
手术方法: 患者取俯卧位,C型臂透视定位伤椎,常规消毒铺巾,以1%利多卡因局麻。
单侧入路:透视定位确定椎弓根体表投影,上胸椎采用经椎弓根外侧入路,胸腰段及腰椎采用经椎弓根入路,调整尖锥入针点及进针角度,旋入(正位尖端达椎体中线、侧位达椎体前1/4稍偏下,若骨折累及下终板的,则进针方向适当靠近上终板),置入工作通道,球囊扩张,膨胀5min后取出球囊,搅拌骨水泥至拔丝期,透视下缓慢注入,至骨水泥在椎体分布良好。
双侧入路:透视定位确定双侧椎弓根体表投影,胸椎及腰椎均采用经椎弓根入路,同法旋入尖锥,正位尖端各自达到椎体中、外1/3处,侧位均达到椎体中前1/3处稍偏下,若骨折累及下终板的,则进针方向适当靠近上终板,置入工作通道,于椎体高度压缩较重一侧置入球囊,或双侧先后使用球囊,扩张后,同法于双侧工作通道交替注入骨水泥。
3 观察指标
主要观察骨水泥用量、手术时间、VAS评分、Cobb角变化度、椎体高度压缩率、恢复率等指标。
骨水泥用量:计算单个椎体骨水泥最终总用量,其中双侧入路时为双侧用量之和。
手术时间:手术时间从穿刺定位开始计时,至骨水泥固化取出工作通道结束计时。
VAS评分:在术前,术后即刻,术后1、3d,1个月对每例患者疼痛症状进行VAS评分,0分:无痛;<3分:有轻微疼痛,能忍受;4~6分,疼痛并影响睡眠,尚能忍受;7~10分:有渐强烈疼痛,难忍受。
Cobb角变化度:术前、术后所有病例均行X线片和CT检查,分别测量每个伤椎的Cobb角(椎体上下缘连线的夹角),Cobb角变化度=术前度数-术后度数。
椎体高度压缩率及恢复率:侧位X线片测量伤椎压缩最明显部位的术前高度h1和术后高度h2以及相应部位上位椎体高度h3和下位h4。得到正常椎体原始高度h=(h3+h4)/2,计算术前椎体压缩率=(h-h1)/h,术后椎体压缩率=(h-h2)/h,依次计算得椎体高度恢复率=(术前压缩率-
术后压缩率)/术前压缩率。
4 统计学处理
应用SPSS 18.0统计软件进行分析,单侧入路及双侧入路组各数据采用t检验。P<0.05为差异有统计学意义。
结 果
单、双侧入路两组患者之间,手术时间差异有统计学意义(P<0.05),单侧入路用时明显少于双侧入路组。两组患者术前和术后对比的VAS评分、Cobb角变化及椎体高度变化的差异均有统计学意义(P<0.05),但两组之间差异并无统计学意义(P>0.05),见表1、2。
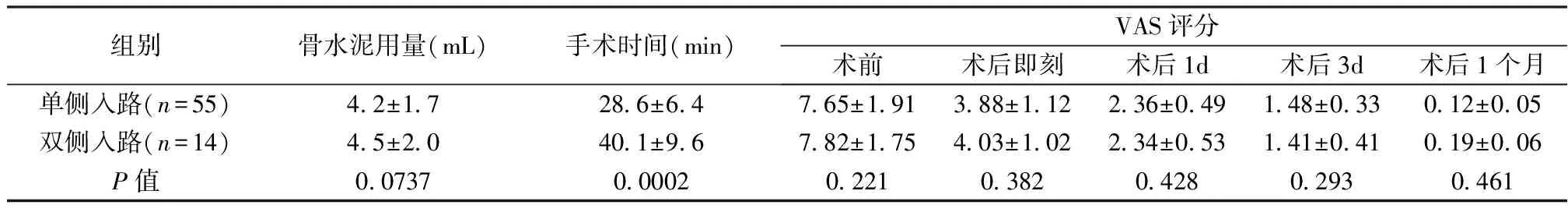
表1 两组骨水泥用量、手术时间,术前术后VAS评分比较
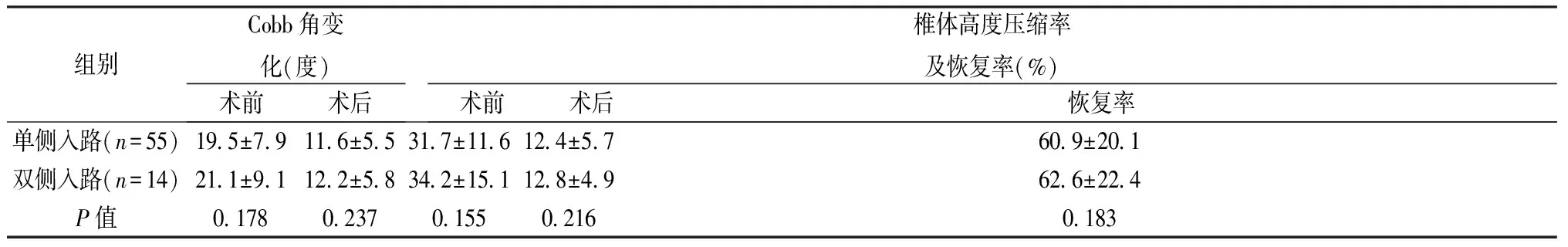
表2 两组术前术后Cobb角变化及椎体高度压缩率及恢复率比较
讨 论
PKP在治疗骨质疏松性胸腰椎压缩骨折方面,因其微创、缓解疼痛立竿见影、操作简便、可在局麻下完成、对老年人麻醉风险小等优点,已被广泛应用于临床。采用单侧入路或双侧入路对手术效果的影响,也有较多学者进行过统计分析,但至今结论仍有较多争议。例如Chen等[7]经过文献综述meta分析后认为,单侧入路用时少,骨水泥用量也少,渗漏风险更小,推荐使用单侧入路。Huang、Hui等[8-9]则认为骨水泥渗漏、相邻节段骨折等并发症无统计学差异,单侧入路仅仅在手术时间和骨水泥用量方面少于双侧入路。本文的69例统计分析结果则显示,单侧入路除了手术时间较少,包括骨水泥用量在内的其他方面,单双侧入路均无统计学差异。笔者认为,骨水泥用量和骨水泥渗漏与单侧入路穿刺技术的学习曲线有一定关系。单侧入路因为要将尖锥尽量穿刺到椎体中线,甚至稍过中线,要求横向角更大,所以在椎弓根内的通道更窄(图1),对穿刺入针点及进针角度的要求更高,难度相对较大,可能会因此增加操作时间,如果穿刺角度不理想,则会影响骨水泥的扩散分布,进而影响骨水泥用量和渗漏方面的统计结果。但只要熟练掌握该技术的原理及相关解剖知识,则基本可以消除上述影响。所以本文的统计结果中,仅仅显示出单侧入路在手术时间上的优势。值得一提的是,笔者医院PKP术中使用的透视机均为C型臂X线机,在透视脊柱正侧位时需反复调整管球方向,需耗费大量时间,极大地延长了操作等待的时间,即使是熟练的操作人员也仍然会对手术时间有较大影响。如果采用G型臂X线机,术前调整好位置后,术中无需移动透视机,能极大缩短穿刺操作时间,在这种情况下,双侧入路手术时间的缩短将会更加明显,届时,两种入路方式的手术时间是否仍会有统计学差异,将有待进一步研究。上述文献中也都未提到C型臂X线机和G型臂X线机透视对手术时间的影响。因此,仅在C型臂X线机透视时,推荐使用单侧入路。
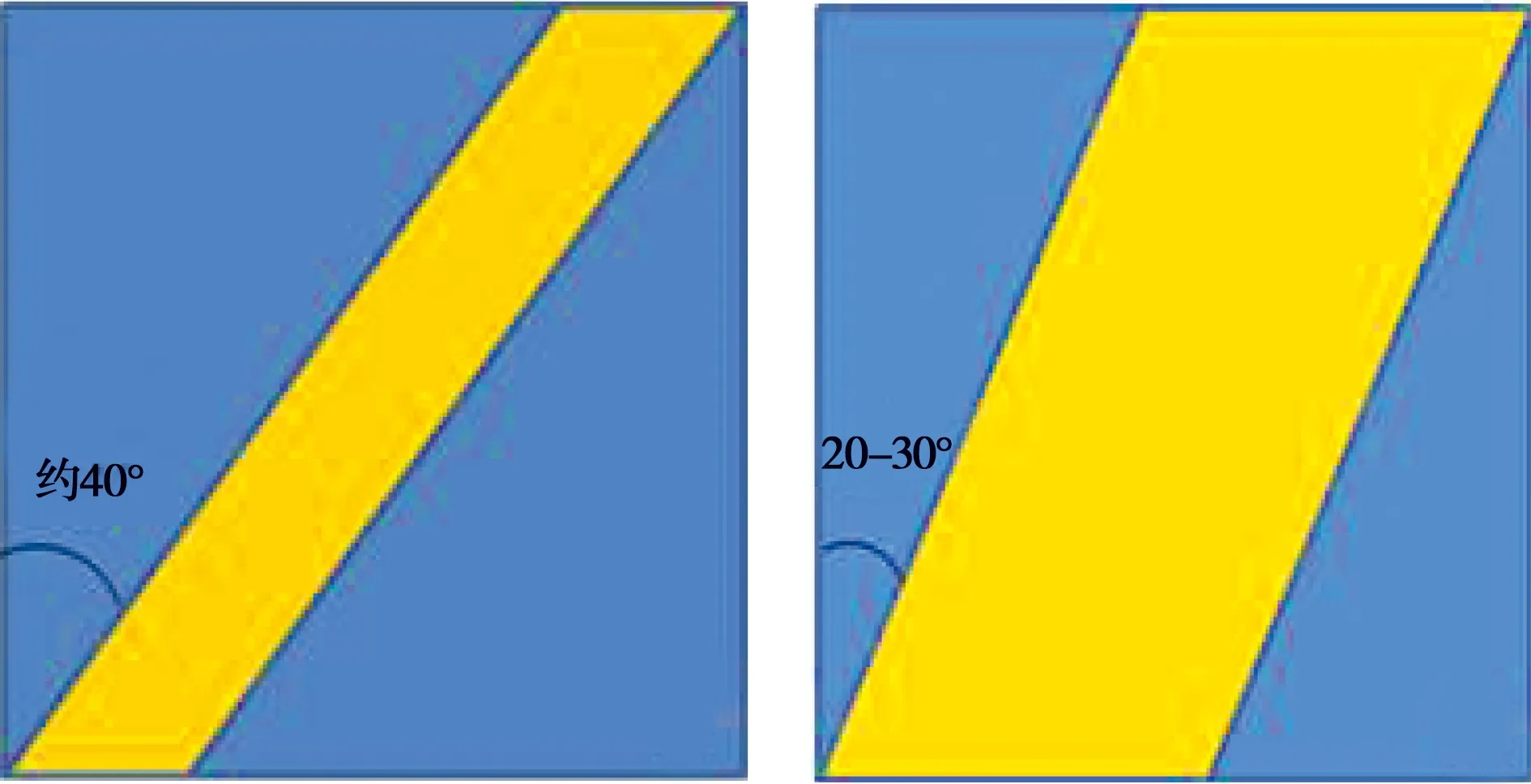
a b
图1 单双侧入路椎弓根通道示意图。a.单侧入路,横向角大,椎弓根内的通道较窄;b.双侧入路,横向角小,通道较宽
[1] Galibert P,Deramond H,Rosat P,et al.Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty [J].Neurochirurgie,1987,33(2):166-168.
[2] Garfin SR,Yuan HA,Reiley MA.New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures [J].Spine(Phila Pa 1976),2001,26(14):1511-1515.
[3] Chung HJ,Chung KJ,Yoon HS,et al.Comparative study of balloon kyphoplasty with unilateral versus bilateral approach in osteoporotic vertebral compression fractures [J].Int Orthop,2008,32(6):817-820.
[4] Lin J,Zhang L,Yang HL.Unilateral versus bilateral balloon kyphoplasty for osteoporotic vertebral compression fractures[J].Pain Physician,2013,16(5):447-453.
[5] Yan L,He B,Guo H,et al.The prospective self-controlled study of unilateral transverse process-pedicle and bilateral puncture techniques in percutaneous kyphoplasty [J].Osteoporosis International,2016,27(5):1849-1855.
[6] Liang L,Chen X,Jiang W,et al.Balloon kyphoplasty or percutaneous vertebroplasty for osteoporotic vertebral compression fracture? An updated systematic review and meta-analysis[J].Ann Saudi Med,2016,36(3):165-174.
[7] Chen H,Tang P,Zhao Y,et al.Unilateral versus bilateral balloon kyphoplasty in the treatment of osteoporotic vertebral compression fractures[J].Orthopedics,2014,37(9):e828-835.
[8] Huang Z,Wan S,Lei N,et al.Is unilateral kyphoplasty as effective and safe as bilateral kyphoplasties for osteoporotic vertebral compression fractures: a meta-analysis[J].Clinical Orthopaedics & Related Research,2014,472(9):2833-2842.
[9] Hui FM,Peng HM,Zhang XS,et al.Unilateral versus bilateral percutaneous kyphoplasty for osteoporotic vertebral compression fractures: a systematic review and meta-analysis of RCTs[J].J Orthop Res,2015,33(11):1713-1723.
(本文编辑: 黄小英)
Comparative study of percutaneous kyphoplasty with unilateral or bilateral approach
HUBo1,SONGAi-guo2,NIWen-zhuo1,YUELi-qun2
(1.The Second Department of Orthopedics, Chaoyang Integrative Medicine Emergency Medical Center.Beijing, China, 100022;2.Trauma Department, Beijing Water Resources Hospital.Beijing, China, 100036 )
Objective To compare the differences of percutaneous balloon kyphoplasty (PKP) in treating osteoporotic thoracolumbar vertebral fractures through unilateral versus bilateral approach. Methods The data of 69 patients who suffered from osteoporotic thoracolumbar vertebral fractures were retrospectively analyzed, who were admitted from Jun.2011 to Oct. 2015 and were treated by PKP through unilateral or bilateral approach. The cement usage,operation time,VAS scores,pre- and post- operative Cobb angle and reduction of vertebral height were analyzed. Results The operating time of unilateral approach was (28.6±6.4) min,and was significantly shorter than that of bilateral approach of (40.1±9.6) min (P<0.05). The cement volumes of the two groups were (4.2±1.7)mL and (4.5±2.0)mL,respectively,which showed no statistical difference(P>0.05). The post-operative Cobb angle of the two groups was (11.6±5.5)° and (12.2±5.8)°,respectively,which was significantly reduced than that of pre-operation[ (19.5±7.9)° and (21.1±9.1)°,respectively,P<0.05],but there was no significant difference between the two groups. The post-operative percentage of the compression of vertebral height of the two groups was (12.4±5.7)% and (12.8±4.9)%,respectively,and was more significantly restored than those of pre-operation[(31.7±11.6)% and (34.2±15.1%),respectively,P<0.05]. The restoration of the two groups was (60.9±20.1)% and (62.6±22.4)% respectively,but there was no significant difference between the two groups. The pre-operative VAS scores of the two groups were (7.65±1.91) and (7.82±1.75),were (3.88±1.12) and (4.03±1.02) immediately after operation,were (2.36±0.49) and (2.34±0.53) at postoperative day 1,were (1.48±0.33) and (1.41±0.41) at postoperative day 3,and were (0.12±0.05) and (0.19±0.06) at 1 month after operation. The pain in both groups was significantly relieved after surgery,but showed no difference between the two groups. Conclusion Both approaches are efficient,but unilateral approach takes less time while using C arm X-ray.
osteoporotic vertebral fractures; thoracolumbar; unilateral approach; bilateral approach; percutaneous kyphoplasty
100022 北京,北京朝阳中西医结合急诊抢救中心骨二科(胡波,倪文卓);100036 北京,北京水利医院创伤科(宋爱国,岳立群)
1009-4237(2017)05-0374-04
R 683.2
A
10.3969/j.issn.1009-4237.2017.05.013
2016-06-21;
2016-09-07)