重症患者疾病严重程度与维生素D水平的相关性研究
2017-08-03杨绍兵李莎莎王晓红杨晓军
杨绍兵,蔡 庆,李莎莎,王晓红,丁 欢,杨晓军
·论 著·
重症患者疾病严重程度与维生素D水平的相关性研究
杨绍兵1,蔡 庆2,李莎莎3,王晓红1,丁 欢1,杨晓军1
目的 观察危重患者血清25-羟维生素D水平与各种疾病严重程度的相关性。方法 收集入住ICU病房时间超过48 h、年龄≥18岁的患者作为观察资料。根据入科24 h内急性生理学与慢性健康状况评分系统Ⅱ(APACHE Ⅱ)评分分为2组(APACHE Ⅱ评分<20分组、APACHE Ⅱ评分≥20分组),比较2组患者次日清晨血清25-羟维生素D水平、乳酸水平及住ICU时间、28 d病死率等指标的差异;并选择同期门诊体检患者60例作为健康人群组,比较健康人群与危重症患者之间25-羟维生素D水平有无差异。结果 共纳入患者114例,APACHE Ⅱ评分<20分患者74例、APACHE Ⅱ评分≥20患者40例。2组血清维生素D3水平分别为(7.77±4.30)ng/mL、(4.95±2.29)ng/mL(P<0.05),乳酸水平分别为(2.17±1.40)mmol/L、(3.76±2.80)mmol/L(P<0.05),白细胞计数分别为(10.73±3.56)×109/mL、(13.68±4.23)×109/mL(P<0.05),住ICU时间分别为(5.19±2.73)d、(7.20±3.03)d(P<0.05),28 d病死率分别为0%、20%,上述变量在2组间差异有统计学意义;血清25-羟维生素D3与APACHE Ⅱ评分呈明显负相关性(r=-0.275,P<0.05)。健康人群组60例,其血清维生素D3水平中位数为16.48 ng/mL,与危重症患者比较差异有统计学意义(P<0.05)。结论 健康人群、危重症患者普遍存在维生素D3不足或者缺乏,危重症患者更加明显,随着病情的危重程度加重,维生素D3水平逐渐减低。
重症患者;急性生理学与慢性健康状况评分系统;25-羟维生素D水平
血清维生素D是一种重要的营养素,在钙磷稳态、骨代谢及细胞生长、分化和凋亡中起着重要的作用[1-2]。维生素D主要通过暴露于阳光及膳食补充获得。近年来研究发现,维生素D不足与心血管疾病、肿瘤发生率、胰岛素抵抗及全因死亡率有关[3-7]。维生素D不足是一个普遍的全球现象,在住院患者尤其是危重症患者中更为显著[8-10]。维生素D不足与ICU患者疾病严重程度有明显的联系[11-12]。宁夏地处高纬度、较高海拔地区,地处此区域的危重症患者及健康人群是否存在维生素D不足的情况,尚未见报道。本研究的目的是评估ICU重症患者疾病严重程度与维生素D水平之间的相关性,并调查健康人群血清25-羟维生素D[25(OH)D]水平。
1 资料与方法
1.1 一般资料:采用前瞻性研究方法,选取宁夏医科大学总医院2014年8月-2015年4月入住ICU病房C区、时间超过48 h、年龄≥18岁的114例患者作为研究对象。年龄18~79岁,平均年龄(58±3.8)岁,性别不限。排除基础存在肾脏疾病及慢性肾功能衰竭、肿瘤以及既往1年内接受过维生素D制剂治疗的患者。病种构成:颅脑损伤及颅脑手术后39例,重症感染20例,胸腹手术后30例,其他25例。同期选择门诊体检患者60例作为健康人群组。本研究经本院伦理委员会批准,并获得患者或家属的知情同意。
1.2 分组:参照Knaus等[13]的标准,根据血清25(OH)D水平定义,维生素D缺乏为25(OH)D<20 ng/mL,维生素D不足为25(OH)D在20~29 ng/mL,维生素D充足为25(OH)D≥30 ng/mL[13]。对入ICU 24 h内患者各项生理参数及实验室指标进行急性生理学与慢性健康状况评分系统Ⅱ(APACHE Ⅱ)评分。国内研究报道,APACHEⅡ分值≥20分时,死亡危险度明显增加,对此应加强监护,及早调整治疗方案[14]。因此,本实验依据评分值,将患者分为2组:APACHE Ⅱ评分<20分,74例;APACHE Ⅱ评分≥20,40例;另选取门诊体检的健康人群组60例。
1.3 方法:对入住ICU患者第1个24 h内行血清25(OH)D标本收集,离心后置于-80 ℃冰箱待检。采用电化学发光法测定(Roche E601,罗氏,Swit)血清25(OH)D水平。

2 结果
2.1 2组患者临床资料的比较:2组患者在年龄、血清25(OH)D水平、白细胞计数、乳酸水平、是否合并多脏器功能障碍综合征(MODS)、住ICU时间及28 d病死率差异有统计学意义(P<0.05),在性别、血小板计数、C反应蛋白(CRP)、血清钙、血清磷、是否机械通气及是否手术差异无统计学意义(P>0.05),见表1。
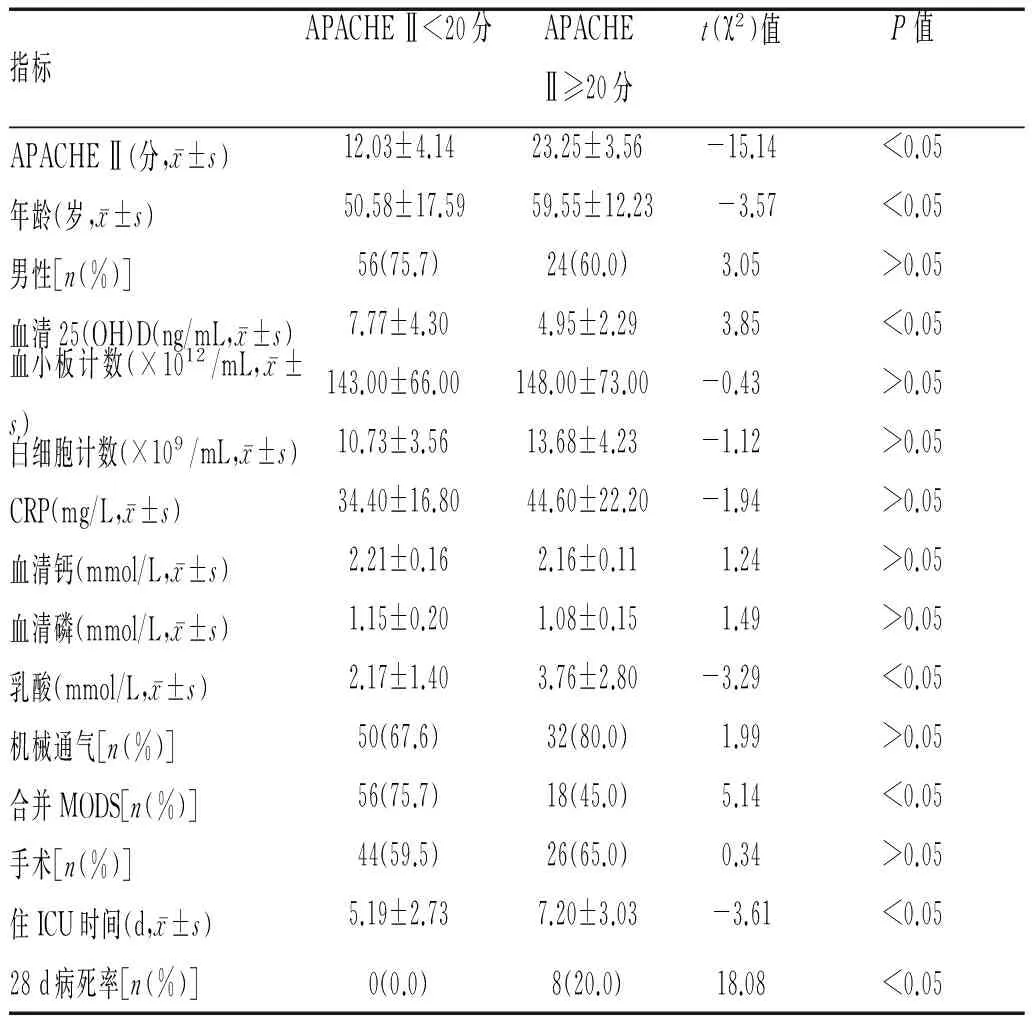
表1 2组危重症患者一般资料的比较
2.2 健康人群及危重患者血清25(OH)D水平缺乏的发生率:入选114例患者中,维生素D充足0例(0%),维生素D不足0例(0%),维生素D缺乏114例(100%),提示危重患者血清25(OH)D水平普遍缺乏。健康人群60例,维生素D充足6例(10%),维生素D不足8例(13%),维生素D缺乏46例(77%),健康人群亦存在维生素D不足或缺乏情况,但危重症患者更加明显(P<0.05),见表2。

表2 健康人群与危重症患者血清25(OH)D水平的比较
2.3 血清25(OH)D水平与患者疾病严重程度的相关性:血清25(OH)D水平与APACHE Ⅱ评分进行相关性分析,Spearman相关系数为-0.275,P<0.05,呈负相关性。结果表明APACHE Ⅱ 评分越高,血清25(OH)D水平越低。
3 讨论
众多流行病学资料和临床观察研究表明,血清维生素D水平低下是多种免疫系统及慢性疾病发病的危险因素,维生素D对多种疾病有潜在的预防和治疗作用,对疾病的严重程度有一定的警示作用。危重患者因为器官功能损害、制动、阳光暴露少、禁食或营养方案不合理等原因,成为维生素D不足或缺乏的高危人群。据文献报告,危重患者中维生素D不足或缺乏的发生率高达74%~98.8%[8-9]。本研究中,维生素D不足或缺乏发生率为100%,较国内其他[15]报道更低,且健康体检人群亦普遍存在维生素D不足或缺乏的情况,考虑原因为宁夏地处高纬度地区、年均气温低、日照时间较低纬度地区短,维生素D3合成较少,且膳食以肉食为主,故宁夏地区人群血清25(OH)D水平较南方地区更低。然而Lee[16]认为,与普通人群相比,ICU人群存在巨大的病理生理学改变及医疗干预措施,可能并不适用于普通人群维生素不足或缺乏的定义标准,制定出适合ICU人群的维生素D最佳水平的定义仍需不断的实践探索和完善。
本研究结果显示,危重症患者维生素D水平与APACHE Ⅱ评分呈负相关性。APACHE Ⅱ评分是ICU中最常用的评估患者预后的评分系统,随评分的增加,患者病死率亦增高。重症患者往往存在多器官功能障碍综合征,常合并免疫麻痹、感染、应激性高血糖、呼吸肌无力等问题。多项研究表明[17-21],高的血清维生素D水平可以改善重症患者免疫麻痹状态,起到增强抗炎症、抗微生物作用,缩短机械通气及ICU停留的时间。
综上所述,健康人群及危重患者维生素D不足或缺乏发生率高,疾病程度越重,患者血清维生素D水平越低。血清维生素D水平对患者病情危重程度有一定预警作用,并且在调节免疫及降低糖尿病、心血管疾病及肿瘤发生率方面具有重要作用,因此不仅应纳入危重患者常规检查中,也应作为健康人群的体检项目,并建议适当补充维生素D3制剂。因本研究纳入病例数不足,2组死亡率病例较少,不能做多因素Logistic回归分析了解血清维生素D水平是否为危重患者死亡的独立的危险因素,因此尚需后期继续收集病例来验证。
[1] Holick MF.Evolution and function of vitamin D[J].Recent Results in Cancer Research,2003,164(5):3-28.
[2] Holick MF.Vitamin D deficiency[J].N Engl J Med,2007,357:266-281.
[3] Heidari B,Nargesi AA,Hafezi Nejad N,et al.Assessment of serum 25-hydroxy vitamin D improves coronary heart disease risk stratification in patients with type 2 diabetes[J].American Heart Journal,2015,170(3):573-579.
[4] Gupta D,Vashi PG,Trukova K,et al.Prevalence of serum vitamin D deficiency and insufficiency in cancer:Review of the epidemiological literature[J].Experimental and Therapeutic Medicine,2011,2(2):181-193.
[5] Asemi Z,Samimi M,Tabassi Z,et al.Vitamin D supplementation affects serum high-sensitivity C-reactive protein,insulin resistance and biomarkers of oxidative stress in pregnant women[J].The Journal of Nutrition,2013,143(9):1432-1438.
[6] Laird E,Ward M,Mcsorley E,et al.Vitamin D and bone health:potential mechanisms[J].Nutrients,2010,2(7):693-724.
[7] Levin GP,Robinson Cohen C,De Boer IH,et al.Genetic variants and associations of 25-hydroxy vitamin D concentrations with major clinical outcomes[J].The Journal of the American Medical Association,2012,308(18):1898-1905.
[8] Lee P,Eisman JA,Center JR.Vitamin D deficiency in critically ill patients[J].The New England Journal of Medicine,2009,360(18):1912-1914.
[9] Lee P.How deficient are vitamin D deficient critically ill patients[J].Critical Care,2011,15(2):154.
[10] Zhen Donghu,Liu Lijuan,Guan Conghui,et al.High prevalence of vitamin D deficiency among middle-aged and elderly individuals in northwestern China:its relationship to osteoporosis and lifestyle factors[J].Bone,2015,71:1-6.
[11] Venkatram S,Chilimuri S,Adrish M,et al.Vitamin D deficiency is associated with mortality in the medical intensive care unit[J].Critical Care,2011,15(6):292.
[12] Arnson Y,Gringauz I,Itzhaky D,et al.Vitamin D deficiency is associated with poor outcomes and increased mortality in severely ill patients[J].International Journal of Medicine,2012,105(7):633-639.
[13] Knaus WA,Draper EA,Wagner DP,et al.APACHE Ⅱ:a severity of disease classification-system [J].Critical Care Medicine,1985,13(10):818-829.
[14] 孙师元APACHEⅡ评分系统对机械通气患者预后病情评估[J].河北医药,2003,5(2):342.
[15] 胡杰妤,陈朝彦,覃桦,等.危重症患者维生素D缺乏及其对预后的影响[J].中华内分泌代谢杂志,2013,29(10):827-829.
[16] Lee P,Eisman JA,Center JR.Vitamin D deficiency in critically ill patients[J].New England Journal of Medicine,2009,360(18):1912-1914.
[17] Lee P.Vitamin D metabolism and deficiency in critical illness[J].Best Practice & Research Clinical Endocrinology & Metabolism,2011,25(5):769-781.
[18] Wejse C,Gomes VF,Rabna P,et al.Vitamin D as supplementary treatment for tuberculosis:a double-blind,randomized,placebo-controlled trial[J].American Journal of Respiratory and Critical Care Medicine,2009,179(9):843-850.
[19] Urashima M,Segawa T,Okazaki M,et al.Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren[J].The American Journal of Clinical Nutrition,2010,91(5):1255-1260.
[20] Jnijni A,Hancock RE.The roles of cathelicidin LL-37 in immune defences and novel clinical applications[J].Curt Opin Hematol,2009,16(1):41-47.
[21] 丁晓飞,张青丽,郝莉,等.1,25(OH)-2D-3对巨噬细胞吞噬金黄色葡萄球菌过程的影响[J].营养学报,2010,32(2):130.
Relationship between APACHE II scores and vitamin D levels in critical ill patients
YANG Shaobing1, CAI Qing2, LI Shasha3, WANG Xiaohong1, DING Huan1, YANG Xiaojun1.
1.Department of Critical Care Medicine, General Hospital of Ningxia Medical University, Yinchuan 750004, China;2.Maternal and Child Health Hospital of Yinchuan City, Yinchuan 750001, China;3.Medical Experimental Center, General Hospital of Ningxia Medical University, Yinchuan 750004, China
YANG Xiaojun,Email: yxjicu@163.com
Objective To investigate the relationship between serum 25-hydroxyvitamin D and different APACHE Ⅱ scores in critically ill patients.Methods The data of patients aged over 18 years who were admitted to ICU from August 2014 to April 2015 in General Hospital of Ningxia Medical University were collected for observation. (APACHE Ⅱ score <20, APACHE Ⅱ score> or = 20) were divided into two groups according to the acute physiology and chronic health evaluation Ⅱ (APACHE Ⅱ) scores within 24 hours after admission. The serum 25- vitamin D levels, lactic acid levels and ICU stay time, 28-day mortality and other indicators were collected, and selected outpatient with physical examination as a normal group, the 25-hydroxy vitamin D levels was compared between healthy people and critically ill patients.Results A total of 114 patients were enrolled in the study. There were 74 patients with APACHE Ⅱ score <20 and 40 patients with APACHE Ⅱ score ≥20. The levels of serum vitamin D3 were respectively (7.77±4.30) ng/mL, (4.95±2.29) ng/mL in two groups (P<0.05). The lactic acid levels were(2.17±1.4)mmol/L and(3.76±2.8)mmol/L (P<0.05). The ICU stay time was(5.19±2.73)days and(7.20±3.03)days (P<0.05), and the 28-day mortality rates were 0% and 20%, respectively. There was a significant difference between the two groups (r= -0.275,P<0.05), and there was a significant negative correlation between the serum 25-hydroxyvitamin D and the APACHE Ⅱ score. Sixty patients were randomly selected for the same period, the serum Vitamin D3level was 16.48 ng/mL, which was significantly different with critically ill patients.Conclusion Healthy people, critically ill patients generally insufficiency or deficiency of 25-hydroxyvitamin D level, and critically ill patients are more obviously. With the severity of the disease increasing, the level of vitamin D3 gradually are decreasing.
Criticallyillpatients;APACHEⅡscore; 25-hydroxyvitaminDlevel
10.13621/j.1001-5949.2017.07.0591
宁夏医科大学科学研究基金资助项目(XM201452)
1.宁夏医科大学总医院重症医学科,宁夏 银川 750004 2.宁夏银川市妇幼保健院妇保科,宁夏 银川 750001 3.宁夏医科大学总医院医学实验中心,宁夏 银川 750004
杨绍兵(1984-),男,大学本科,主要从事重症医学工作。
杨晓军,Email:yxjicu@163.com
http://kns.cnki.net/kcms/detail/64.1008.R.20170720.1011.002.html
R459
A
2016-10-04 [责任编辑]李 洁
