地黄饮子对脑缺血再灌注大鼠海马脑源性神经营养因子和基质细胞衍生因子表达的影响
2017-07-18姚姝娱
姚姝娱
·基础医学· ·论著·
地黄饮子对脑缺血再灌注大鼠海马脑源性神经营养因子和基质细胞衍生因子表达的影响
姚姝娱
目的 探讨地黄饮子对脑缺血再灌注大鼠海马脑源性神经营养因子(brain derived neurotrophic factor, BDNF)和基质细胞衍生因子(stromal cell derived factor 1, SDF1)的表达及修复神经元的作用机制。方法 选取清洁级SD大鼠75只,按数字表法随机分为正常组、治疗组和缺血组,每组25只。10%水合氯醛麻醉,暴露并钳夹双侧颈总动脉40 min,造模使大鼠急性脑缺血。治疗组:造模后灌服地黄饮子汤36 g/kg;缺血组:造模后每日胃灌盐水1次;正常组:正常饮食。3周后,测量大鼠脑梗死面积,分别测定3组大鼠脑海马CA1区BDNF和SDF1蛋白表达情况。结果 正常组海马CA1区BDNF(99.25±9.48)和SDF1蛋白含量[(2.59±0.76) mg/L]均明显高于地黄饮子治疗组[BDNF:(79.98±10.68), SDF1蛋白含量: (3.68±0.96) mg/L]]和缺血组[BDNF:(59.59±13.73),SDF1蛋白含量:(0.93±1.24) mg/L],差异有统计学意义(P<0.05)。地黄饮子治疗组BDNF和SDF1蛋白含量明显高于缺血组,差异有统计学意义(P<0.05)。治疗组的脑梗死面积明显低于缺血组,差异有统计学意义(P<0.05)。结论 地黄饮子治疗可以提高BDNF和SDF1蛋白水平,增加内源性保护机制和神经干细胞增殖、迁移,保护神经元的功能。
脑缺血再灌注;大鼠海马;脑源性神经营养因子;基质细胞衍生因子
脑缺血再灌注是近年来医疗界非常重视的研究领域,为临床上脑血管急性缺血期的治疗提供有力的依据。脑缺血包括大脑的神经损伤和神经生长因子的修复、神经功能缺失[1-2]等,在临床上造成较高的致残率,甚至死亡,由缺血造成的脑血管病占所有脑血管病的80%[3],因此及时有效的治疗,可减少脑卒中的发生。脑源性神经营养因子(brain derived neurotrophic factor, BDNF)和基质细胞衍生因子的释放1(stromal cell derived factor 1, SDF1),都是神经营养家族的成员,都具有减少自由基、减少神经细胞凋亡、保护神经元等作用。本研究通过观察BDNF和SDF1蛋白表达情况,探讨BDNF和SDF1修复神经功能的作用机制。
1 资料与方法
1.1 实验动物及分组 健康清洁级成年SD大鼠75只,雌雄不限,体质量250~280 g,由中国医科大学动物部提供,动物合格证号:SCXK-LN2014-0007。按数字表法随机分为治疗组、缺血组和正常组,每组25只。治疗组:造模后灌服地黄饮子汤36 g/kg,连续3周。缺血组:造模后每日胃灌盐水1次,连续3周。正常组:正常饮食。本实验经医院伦理委员会批准,对实验动物的处置符合《善待实验动物指导意见》中相关规定。
1.2 动物模型的建造 参照文献[4]。
1.3 地黄饮子汤的配制 按照《黄帝素问宣明论方》记载的地黄饮子配制:熟地黄12 g、白茯苓12 g、山茱萸15 g、巴戟天15 g、麦门冬15 g、肉苁蓉15 g、石斛15 g、炮附子15 g、菖蒲12 g、官桂10 g、远志10 g、五味子10 g。用12倍量和10倍量水煎煮2次,每次1 h,将2次药液混合,用旋转仪蒸发浓缩,干燥密封备用。
1.4 BDNF和SDF1含量的测定 采用免疫组织化学测定海马CA1区BDNF和SDF1蛋白含量,对所有大鼠麻醉灌流固定大脑,石蜡包埋并石蜡切片。脱蜡、水化,灭活内源性过氧化物酶活性,抗原修复,滴加兔抗人BDNF多克隆抗体(北京博奥森生物有限科技公司,浓度1∶300),滴加鼠抗BrdU单克隆抗体(北京博奥森生物有限科技公司,浓度1∶50),湿盒中4 ℃冰箱过夜。SABC(1∶150)试剂盒检测大鼠脑CA1区BDNF和BrdU,DAB显色,最后脱水封片。具体步骤:(1)采用日本Olympus图像分析仪,400倍视野下计数BDNF和BrdU的阳性细胞数量。(2)用MetaMorph Offline 4.65图像分析鼠脑海马CA1区BDNF蛋白含量的平均积分光密度(IOD),选取平均测量值。(3)参照大鼠脑图谱,取大脑海马组织,加入体积比10∶1的PIPA裂解液中,分离的蛋白溶解,用ELISA测定脑组织蛋白中SDF1的含量(参照说明书步骤)。
1.5 测量大鼠脑梗死面积 实验3周后,断头取脑,盐水冲洗大脑并吸干,将大脑冠状切片,加入1%2,3,5-三苯基四氮唑的磷酸缓冲液中进行染色,避光30 min,间隔6 min转动1次,脑片拍照,采用Imagepro Plus 6.0图像分析仪,计算脑梗死面积,脑梗死比例(%)=(白色的梗死面积/片子的总面积)×100%。
1.6 统计学处理 用SPSS 17.0统计学分析,多组间用单因素方差分析比较,P<0.05差异有统计学意义。
2 结果
2.1 地黄饮子对大鼠脑海马CA1区BDNFIOD值和SDF1蛋白含量的影响 正常组BDNFIOD值和SDF1蛋白表达明显高于治疗组和缺血组,差异有统计学意义(P<0.05)。治疗组BDNFIOD值和SDF1蛋白表达明显高于缺血组,差异有统计学意义(P<0.05)。见表1。
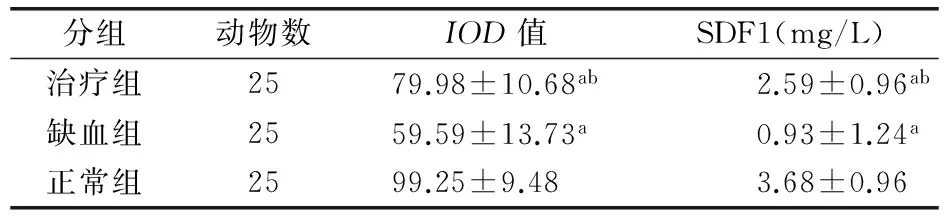
表1 3组大鼠脑海马CA1区BDNF蛋白IOD值和SDF1蛋白含量比较(x±s)
注:与正常组比较aP<0.05;与模型组比较bP<0.05。IOD:平均积分光密度,BDNF:脑源性神经营养因子,SDF1:基质细胞衍生因子
2.2 地黄饮子对大鼠脑梗死面积的影响 治疗组的脑梗死面积(16.84%)明显低于缺血组(37.58%),差异有统计学意义(P<0.05)。
2.3 3组大鼠脑海马CA1区免疫组化染色情况 图1可见SDF1蛋白圆形细胞核大,棕黄色圆形,正常组比治疗组和缺血组的SDF1蛋白含量高,治疗组比缺血组的蛋白含量高。图2可见BDNF蛋白多边形,细胞核大呈圆形,棕褐色椭圆形,正常组BDNF蛋白表达多于治疗组和缺血组,治疗组BDNF蛋白表达多于缺血组。

注:A:治疗组;B:缺血组;C:正常组。SDF1:基质细胞衍生因子图1 3组大鼠脑海马CA1区SDF1蛋白免疫组化图示(×400)

注:A:治疗组;B:缺血组;C:正常组。BDNF:脑源性神经营养因子图2 3组大鼠脑海马CA1区BDNF蛋白免疫组化图示(×400)
3 讨论
BDNF广泛分布在脑组织中,主要集中在大脑海马CA1区和大脑皮层,其含量直接影响神经系统的发育,对神经细胞的增殖、生长和分化起到促进作用,并有保护神经元、促进神经元再生等功能。BDNF通过与脑源性神经营养因子的受体(TrkA)结合,激活传导信号,促进神经细胞再生和保护神经元的作用;同时,BDNF还具有促进细胞增殖、形成新生血管、减少神经元损伤[5-6]、逆转神经细胞凋亡的传导通路、激活神经细胞再生[7]的作用。有研究表明[8],脑缺血再灌注后大鼠脑皮层的BDNF mRNA表达减少;同时,有研究[9-10]证实,大脑缺血区的BDNF减少,造成脑梗死面积增加,与本实验结果一致,可以得出结论脑缺血损伤造成了BDNF表达减少。
SDF1是增强神经信息传递、调节神经功能的重要因子,脑缺血发生后,脑细胞水肿的同时产生大量的自由基、细胞因子、炎性因子等,SDF1通过CXCR4传导信号,使海马区的神经干细胞诱导SDF1发生迁移、分化至缺血区,并分化为神经元,演变为神经细胞使受损的神经得到修复[11]。有研究表明[12],地黄饮子治疗后脑缺血区SDF1蛋白含量增加,神经干细胞迁移和增殖增多。本实验得出结果,大鼠脑缺血区海马SDF1蛋白含量明显低于正常组,经治疗后SDF1蛋白表达明显增高,脑梗死面积减少,提示得到修复的神经细胞和迁移的神经元增多,减轻了脑水肿和脑损伤,对脑组织起到有效的保护作用。
[1] 邹伟,于婷婷,王冬,等.头针透穴法对脑出血大鼠脑组织中β-catenin表达影响的实验研究[J].中医药信息,2014,31(1):76-79.
[2] 李林,李斌,叶翠飞,等. 中药复方962对老年大鼠学习记忆功能及兴奋性的影响[J]. 中国老年学杂志, 2000, 20(6): 364-366. DOI:10.3969/j.issn.1005-9202.2000.06.023.
[3] Durukan A, Tatlisumak T. Acute ischemic stroke: overview of major experimental rodent models, pathophysiology, and therapy of focal cerebral ischemia[J]. Pharmacol Biochem Behav, 2007, 87(1): 179-197. DOI:10.1016/j.pbb.2007.04.015.
[4] 宫健伟,叶蕾,樊巧玲. 地黄饮子对脑缺血再灌注模型大鼠Bax,Bcl-2,Caspase-3 蛋白表达的影响[J]. 中国实验方剂学杂志, 2013, 19(5): 248-251.
[5] Wei OY, Huang YL, Da CD, et al. Alteration of basic fibroblast growth factor expression in rat during cerebral ischemia[J]. Acta Pharmacol Sin, 2000, 21(4): 296-300.
[6] Saarelainen T, Lukkarinen JA, Koponen S, et al. Transgenic mice overexpressing truncated trkB neurotrophin receptors in neurons show increased susceptibility to cortical injury after focal cerebral ischemia[J]. Mol Cell Neurosci, 2000, 16(2): 87-96. DOI:10.1006/mcne.2000.0863.
[7] Jin K, Minami M, Lan JQ, et al. Neurogenesis in dentate subgranular zone and rostral subventricular zone after focal cerebral ischemia in the rat[J]. Proc Natl Acad Sci USA, 2001, 98(8): 4710-4715. DOI:10.1073/pnas.081011098.
[8] 肖爱娇,陈日新,康明非,等. 脑缺血再灌注损伤模型大鼠大脑皮质BDNF mRNA表达减少[J]. 中风与神经疾病杂志, 2012, 29(2): 122-125.
[9] Lee CH, Park JH, Yoo KY, et al. Pre- and post-treatments with escitalopram protect against experimental ischemic neuronal damage via regulation of BDNF expression and oxidative stress[J]. Exp Neurol, 2011, 229(2): 450-459. DOI:10.1016/j.expneurol.2011.03.015.
[10] Li H, Park JH, Yan B, et al. Neuroprotection of Alpinia katsumadai Seed Extract against Neuronal Damage in the Ischemic Gerbil Hippocampus is Linked to Altered Brain-Derived Neurotrophic Factor[J]. Lab Anim Res, 2011, 27(1): 67-71. DOI:10.5625/lar.2011.27.1.67.
[11] 陈东风,杜少辉,李伊为,等. 龟板含药血清体外诱导成年大鼠骨髓间充质干细胞分化为神经元[J]. 广州中医药大学学报, 2003, 20(3): 224-226.
[12] 蔡光先,林琳,刘柏炎,等. 地黄多糖诱导骨髓间充质干细胞分化为神经样细胞的效应[J]. 中国临床康复, 2005, 9(17): 46-47. DOI:10.3321/j.issn:1673-8225.2005.17.028.
(本文编辑:林永丽)
Expression and significance of brain derived neurotrophic factor and stromal cell derived factor 1 in the hippocampus of rats with cerebral ischemia reperfusion
YaoShuyu
(AffiliatedHospitalofLaoningChineseHerbalMedicineUniversity,Shenyang110032,China)
Objective To explore the expression of brain derived neurotrophic factor (BDNF) and stromal cell derived factor 1(SDF1) in the hippocampus of rats following cerebral ischemia reperfusion, and the mechanism involved in the repair of neurons.Methods Seventy-five SD rats were randomly divided into the normal group, the treatment group and the ischemia group, each consisting of 25 animals. Chloral hydrate at a concentration of 10% was used to induce anesthesia. Bilateral common carotid artery was exposed and clipped for 40 minutes to develop an acute cerebral ischemia model. Following development of the model, the treatment group was given rehmannia Yinzi liquid by gavage at a dosage of 36 g/kg, while the ischemia group received physiological saline also by gavage once a day. The normal group was given normal feed. Three weeks later, the areas of cerebral infarction were detected, and the expression levels of BDNF and SDF1 were respectively detected in CA1 of the hippocampus.Results The levels of BDNF (99.25±9.48) and SDF1 [(3.68±0.96) mg/L] in CA1 in the animals of the normal group were all significantly higher than those of the treatment group [ (79.98±10.68) and (2.59±0.76) mg/L] and the ischemia group [ (59.59±13.73) and (0.93±1.24) mg/L], and statistical significance could be seen, when comparisons were made between them (P<0.05). The levels of BDNF and SDF1 in the rehmanniae Yinzi treatment group were also obviously higher than those of the ischemic group, also with statistical significance (P<0.05). The area of cerebral infarction of the treatment group was significantly smaller than that of the ischemia group, also with statistical significance (P<0.05).Conclusion Rehmannia Yinzi liquid could increase the levels of BDNF and SDF1, improve the endogenous protective effect, enhance the proliferation and migration of stem cells, and had the function to protect neurons.
Cerebral ischemia reperfusion; Hippocampus; Brain derived neurotrophic factor; Stromal cell derived factor 1
110032 沈阳,辽宁中医药大学附属医院
Q95-33
A
10.3969/j.issn.1009-0754.2017.03.012
2016-04-08)