胆囊结石合并胆总管结石的微创治疗体会
2017-07-12孙举来赵中伟
徐 浩,孙举来,芮 翾,邵 远,赵中伟
(马鞍山市中心医院,安徽 马鞍山,243000)
胆囊结石合并胆总管结石的微创治疗体会
徐 浩,孙举来,芮 翾,邵 远,赵中伟
(马鞍山市中心医院,安徽 马鞍山,243000)
目的:比较腹腔镜胆囊切除术(laparoscopic cholecystectomy,LC)联合腹腔镜胆总管探查术(laparoscopic common bile duct exploration,LCBDE)与内镜逆行胰胆管造影(endoscopic retrograde cholangiopancreatography,ERCP)、内镜十二指肠乳头括约肌切开术(endoscopic sphincterotomy,EST)+LC治疗胆囊结石合并胆总管结石的临床疗效。方法:在2010年1月至2015年11月收治的胆囊结石合并胆总管结石患者中选取可耐受腹腔镜手术、ERCP且ASA分级为Ⅰ~Ⅱ级的成年患者作为研究对象,危急重症胆囊炎、急性胆管炎及要求保守治疗的患者未纳入研究。分为两组:LC+LCBDE组与ERCP/EST+LC组,比较分析两组患者术中出血量、手术时间、住院时间、住院费用及术后并发症等指标。结果:共纳入76例患者,30例行LC+LCBDE,其中2例中转开腹;46例行ERCP/EST+LC,其中2例因ERCP取石失败,不予统计。两组患者术中出血量、术后并发症差异无统计学意义,LC+LCBDE组手术时间、住院时间、住院费用优于ERCP/EST+LC组,差异有统计学意义。结论:两种术式治疗胆囊结石合并胆总管结石的疗效相当,但LC+LCBDE可能更加经济实惠。
胆囊结石病;胆总管结石;腹腔镜检查;内窥镜检查
胆囊结石伴胆总管结石是普通外科常见病,发病率为10%~15%,且发病率呈逐年增加的趋势[1]。目前认为胆总管结石形成的原因主要是胆囊内结石进入胆总管内及胆总管自发结石[2]。临床中胆囊结石伴胆总管结石往往起病急,症状明显,而且容易导致胆源性胰腺炎[3],因此需要积极治疗。目前治疗胆囊结石合并胆总管结石的主要方案包括:(1)传统开腹手术;(2)内镜逆行胰胆管造影(endoscopic retrograde cholangiopancreatography,ERCP)、内镜十二指肠乳头括约肌切开术(endoscopic sphincterotomy,EST)+腹腔镜胆囊切除术(laparoscopic cholecystectomy,LC);(3)LC联合腹腔镜胆总管探查术(laparoscopic common bile duct exploration,LCBDE)。随着内镜、腹腔镜技术的迅猛发展,微创技术的日益成熟,上述后两种治疗方案较传统开腹手术优势更加明显,是目前临床常用的方法[4]。本文分析2010年1月至2015年11月马鞍山市中心医院收治的76例患者,其中LC+LCBDE 30例,ERCP/EST+LC 46例,主要比较LC+LCBDE与ERCP/EST+LC治疗胆囊结石合并胆总管结石的疗效,现报道如下。
1 资料与方法
1.1 临床资料 选取2010年1月至2015年11月马鞍山市中心医院普通外科及消化内科收治的胆囊结石合并胆总管结石患者,其中可耐受腹腔镜手术、ERCP且ASA分级为Ⅰ~Ⅱ级的成年患者作为研究对象,危急重症胆囊炎、急性胆管炎及要求保守治疗的患者未纳入研究。患者术前均经肝胆胰脾彩超、上腹部核磁共振及磁共振胰胆管造影明确诊断,并排除肝内胆管结石。男31例,女45例;37~76岁,平均(54.29±10.72)岁,其中30例行LC+LCBDE(腹腔镜组),46例行ERCP/EST+LC(内镜组),随访2~24个月,患者资料见表1。


组别例数(n)性别(n)男女年龄(岁)最大结石直径(cm)总胆红素(μmol/L)血淀粉酶(U/L)白细胞(×109/L)谷丙转氨酶(U/L)腹腔镜组30131753.17±8.740.52±0.2634.48±16.92112.96±33.947.97±2.24119.29±18.36内镜组46182855.02±9.960.60±0.3936.38±20.40116.55±29.806.95±1.32124.43±21.59χ2/t值0.133⁃0.830⁃0.988⁃0.424⁃0.4862.499⁃1.074P值0.7160.4090.3260.6730.6290.0150.286
1.2 手术方法 手术均由副主任医师或以上职称医师担任主刀。(1)腹腔镜组:全麻满意后,于常规穿刺点穿刺Trocar。置入腹腔镜探查各脏器,分离胆囊周围组织,游离出胆囊管、胆囊动脉,胆囊端用钛夹夹闭,胆总管端用Hem-o-lok夹闭,最后切除胆囊。确定胆总管位置后,于胆总管上段切开,胆道镜直视下取尽结石,放置T管引流胆汁,术后1~2周行T管造影,正常情况下于术后1~3个月返院拔除T管。1例患者因组织粘连导致胆囊暴露困难及胆囊三角解剖关系模糊,术中分离造成了出血、胆管损伤;1例胆总管直径约0.75 cm,手术难度非常大,难以放置T管中转开腹(数据不计入统计)。术后予以吸氧、心电监护、抗炎、抑酸等对症治疗,常规监测血糖及血压24 h,q4 h,并及时处理。嘱患者术后8 h下床活动(长期卧床病例除外),术后8 h闻及肠鸣音后进少量饮水,24 h后可进食流质。(2)内镜组:由消化内科医师行ERCP+EST。麻醉满意后常规行ERCP,了解胆总管结石情况,并根据术中所见选择网篮碎石后行Oddi括约肌切开取石或直接Oddi括约肌切开取石,EST取石术后7~10 d内转普通外科行LC。其中2例患者因ERCP取石失败,改行传统开腹取石手术(数据不计入统计)。

2 结 果
两组患者性别、年龄、最大结石直径、总胆红素量、血淀粉酶、白细胞计数、谷丙转氨酶差异无统计学意义,两组研究是在同一基线上,具有可比性。见表1。两组患者术中出血量差异无统计学意义(P>0.05),手术时间、住院时间、住院费用两组相比差异有统计学意义(P<0.05)。见表2。两组患者术后并发症如胆道感染、胰腺炎、术后结石残余、胆漏、肠穿孔发生率差异无统计学意义(P>0.05)。见表3。

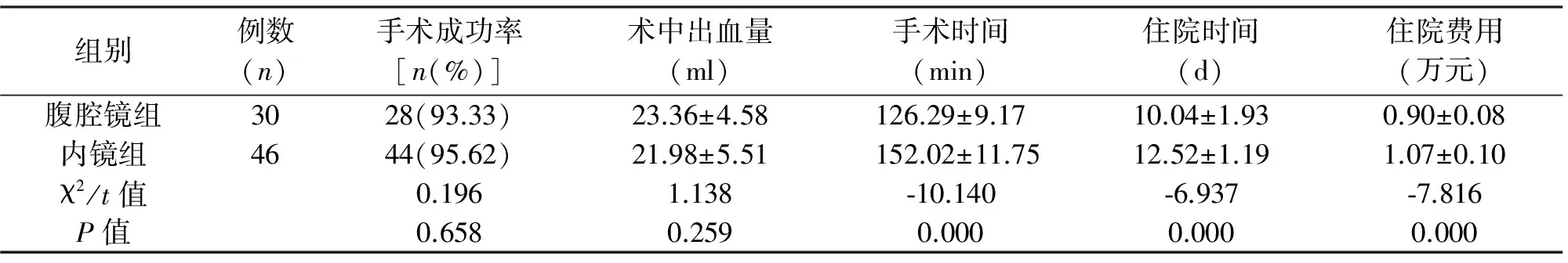
组别例数(n)手术成功率[n(%)]术中出血量(ml)手术时间(min)住院时间(d)住院费用(万元)腹腔镜组3028(93.33)23.36±4.58126.29±9.1710.04±1.930.90±0.08内镜组4644(95.62)21.98±5.51152.02±11.7512.52±1.191.07±0.10χ2/t值0.1961.138⁃10.140⁃6.937⁃7.816P值0.6580.2590.0000.0000.000
表3 两组患者术后并发症的比较(n)

组别胆道感染胰腺炎术后结石残余胆漏肠穿孔腹腔镜组30210内镜组32101χ2值0.352P值0.553
3 讨 论
传统开腹手术治疗胆囊结石合并胆总管结石是行胆管切开取石、T管引流术,其疗效确切,结石清除率高,手术彻底且费用低,操作简便,易于在基层医院推广[5]。但其缺点同样很明显,手术创伤大,患者痛苦多,住院时间长,美观效果差,术后并发症多等。
自1968年ERCP问世以来,1974年EST开创了治疗胆总管结石的先河,目前已日益发展成熟,并得到推广普及,是治疗胆总管结石的标准模式[6]。自1987年首例LC由Mouret完成至今[7],腹腔镜技术得到了长足发展、广泛普及,腹腔镜手术已成为治疗很多常见疾病(如胆囊结石、阑尾炎、胃癌、结直肠癌等)的首选方案[8]。腹腔镜与内镜联合的阶梯治疗已成为微创治疗胆石症的主要方式,然而腹腔镜与内镜联合包括LC联合术前、术中、术后EST等三种不同方式,其中腹腔镜联合术前EST是目前外科最常用的治疗手段,其优点为:(1)经ERCP明确肝内外胆管的病变情况,一旦发现胆管结石或狭窄等,即行EST切开狭窄与取石治疗。(2)经ERCP可获得良好的胆道影像学资料,同时术后常规置入鼻胆引流管,既保证胆道引流通畅,又可减少术后胆道系统感染等并发症的发生,避免胆管损伤。(3)术前通过ERCP/EST迅速解除胆道梗阻,引流胆汁减轻炎症反应,为LC的顺利开展奠定了基础。(4)即使术前ERCP/EST取石失败,也可改LC为传统开腹手术。但腹腔镜联合内镜的阶梯治疗也存在一定缺点:(1)患者需承受至少2次的有创操作,总住院时间较长。(2)胆囊结石可能再次进入胆总管。(3)一些较大的结石难以通过ERCP/EST取出。(4)十二指肠括约肌功能遭到破坏,可能存在长期风险[9-10]。
近年,有学者提出了完全腹腔镜手术治疗胆囊结石合并胆总管结石,此治疗方案完全摆脱了ERCP/EST,一次麻醉、一次操作就能较彻底地解决患者的痛苦,手术安全、微创、疗效佳,并发症发生率低,患者术后康复快[11-14]。
本研究中,手术时间、住院时间、住院费用方面两组差异有统计学意义(P<0.05);但在术中出血量、术后并发症(如胆道感染、胰腺炎、术后结石残余、胆漏、肠穿孔)发生率方面差异无统计学意义(P>0.05)。我们在实际操作过程中也存在以下问题:(1)胆总管直径>1 cm的患者手术难度非常大,难以放置T管,导致1例手术失败,且术后并发胆总管狭窄;(2)胆总管切开后给患者带来的创伤较大,相应的禁饮食时间较长;(3)患者需长时间带T管(1~3个月),给患者带来了极大的痛苦与不便。在总结经验教训后,我们认为术前影像学资料显示胆总管内径<1.0 cm、结石嵌顿在胆管下段或胆管下端欠通畅时,对于年龄大、病情重或重度梗阻性黄疸患者可考虑首选ERCP/EST,能迅速解除胆管梗阻,通畅引流,改善患者肝功能及全身情况,ERCP/EST+LC更具优势。还有学者认为,腹腔镜胆总管一期缝合术也是治疗肝外胆管结石理想的微创术式[15],但作为基层医院的笔者,本研究中患者均留置T管,后期手术中可尝试行胆总管一期缝合,以减少留置T管带来的痛苦。
综上所述,笔者认为LCBDE+LC的手术方案较ERCP/EST+LC联合阶梯治疗具有一定优势,如果患者胆总管内径>1.0 cm,且病情较轻,无重度梗阻性黄疸可优选LCBDE治疗胆囊结石合并胆总管结石。目前LCBDE已开辟了治疗胆囊结石合并胆管结石的新途径,具有安全、微创、疗效佳、并发症发生率低、术后康复快的特点,因而值得临床推广与普及。但本研究病例数较少,且未进行随机对照研究,各种术式都有其适应证与不足,如何根据患者病情选择合适的方式仍需要大量随机对照临床试验。
[1] Qiu Y,Yang Z,Li Z,et al.Is preoperative MRCP necessary for patients with gallstones?An analysis of the factors related to missed diagnosis of choledocholithiasis by preoperative ultrasound[J].BMC Gastroenterol,2015,15:158.
[2] Al-Mulhim AS,Al-Mulhim AA.Laparoscopic cholecystectomy in 427 adults with sickle cell disease:a single-center experience[J].Surg Endosc,2009,23(7):1599-1602.
[3] 朱杰高,韩威,张忠涛,等.胆囊结石合并胆总管结石的治疗新进展[J].中国全科医学,2013,16(5):1702-1704.
[4] Varban O,Assimos D,Passman C,et al.Laparoscopic common bile duct exploration and holmium laser lithotripsy:a novel approach to the management of common bile duct stones[J].Surg Endosc,2010,24(7):1759-1764.
[5] Ko CW,Lee SP.Epidemiology and natural history of common bile duct stones and prediction of disease[J].Gastrointest Endosc,2003,56(6 Suppl):165-169.
[6] 中华医学会消化内镜分会ERCP学组,胡冰,麻树人,等.内镜下逆行胆胰管造影术(ERCP)诊治指南(2010版)[S].中国继续医学教育,2010,2(6):1-20.
[7] Mouret P.How I developed laparoscopic cholecystectomy[J].Ann Acad Med Singapore,1996,25(5):744-747.
[8] 尚进才,李永武,李艳美.腹腔镜技术的研究进展[J].医学理论与实践,2013,26(16):2137-2138.
[9] Tzovaras G,Baloyiannis I,Zachari E,et al.Laparoendoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis:interim analysis of a controlled randomized trial[J].Ann Surg,2012,255(3):435-439.
[10] Oh HC,Cheon YK,Cho YD,et al.Use of udenafil is not associated with a reduction in post-ERCP pancreatitis:results of a randomized,placebo-controlled,multicenter trial[J].Gastrointest Endosc,2011,74(3):556-562.
[11] Rogers SJ,Cello JP,Horn JK,et al.Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease[J].Arch Surg,2010,145(1):28-33.
[12] 胡三元,张阳德.腹腔镜经胆囊管胆总管探查取石术临床研究(附186例报告)[J].中国内镜杂志,2011,17(3):286-288.[13] Lee HM,Min SK,Lee HK.Long-term results of laparoscopic common bile duct exploration by choledochotomy for choledocholithiasis:15-year experience from a single center[J].Ann Surg Treat Res,2014,86(1):1-6.
[14] 李凤鸣.十二指肠镜联合腹腔镜治疗胆囊结石合并胆总管结石[J].腹腔镜外科杂志,2016,21(7):540-542.
[15] 刘威,沈根海,高泉根,等.腹腔镜胆总管一期缝合术与T管引流术治疗肝外胆管结石的疗效比较[J].腹腔镜外科杂志,2016,21(7):543-546.
(英文编辑:柳俏然)
Clinical trials of the efficiency of mini-invasive treatment for cholecystolithiasis and choledocholithiasis
XUHao,SUNJu-lai,RUIXuan,etal.
DepartmentofGeneralSurgery,theCentralHospitalofMaAnShan,MaAnShan243000,China
Objective:To compare the clinical efficacy between laparoscopic cholecystectomy (LC)+laparoscopic common bile duct exploration (LCBDE) and endoscopic retrograde cholangiopancreatography (ERCP)/endoscopic sphincterotomy (EST)+LC for cholecystolithiasis and choledocholithiasis.Methods:Patients who were diagnosed with gallbladder stones with common bile duct stones from Jan.2010 to Nov.2015 were selected,of whom the adult patients who were classified as ASA Ⅰ-Ⅱ and could tolerate abdominal surgery and ERCP were chosen as research objects.Patients who had critical cholecystitis,acute cholangitis or required conservative treatment were excluded.The patients were divided into two groups:the patients treated by LC+LCBDE were named as laparoscopic group and the patients treated by ERCP/EST+LC were named as endoscopic group.The indicators such as blood loss,operation time,hospital stay,hospitalization costs and postoperative complications were compared between the two groups.Results:Of the 76 included patients,30 cases belonged to laparoscopic group,in which 2 cases were not taken in to account for conversion to laparotomy;and 46 cases belonged to endoscopic group,of which 2 cases were excluded for conversion to laparotomy after failure of ERCP.There was no statistically significant difference in blood loss and postoperative complications in two groups.But the laparoscopic group was superior to endoscopic group in operation time,hospital stay as well as hospitalization costs,and the differences were statistically significant.Conclusions:The efficacy of LC+LCBDE vs.ERCP/EST+LC for gallbladder stones with common bile duct stone is equivalent,while the former one is much more affordable.
Cholecystolithiasis;Choledocholithiasis;Laparoscopy;Endoscopy
1009-6612(2017)05-0352-04
10.13499/j.cnki.fqjwkzz.2017.05.352
徐 浩(1980—)男,安徽省马鞍山市中心医院普通外科主治医师,主要从事肝胆外科的研究。
R657.4
A
2016-06-12)
* 通讯作者:赵中伟,E-mail:zzwzzw71@sina.com
