血小板与淋巴细胞比值与NSTEMI患者冠状动脉病变严重程度的相关性研究
2017-07-01郭英杰宁彬葛慧娟庄晓赛
郭英杰,宁彬,葛慧娟,庄晓赛
• 论著 •
血小板与淋巴细胞比值与NSTEMI患者冠状动脉病变严重程度的相关性研究
郭英杰1,宁彬1,葛慧娟1,庄晓赛1
目的 研究血小板与淋巴细胞比值(PLR)与非ST段抬高型心肌梗死(NSTEMI)患者冠状动脉病变程度的关系。方法 选取2013年2月~2015年12月于阜阳市人民医院心血管内科住院的NSTEMI患者共92例,行冠状动脉造影检查并予SYNTAX评分系统评分,取同期该院临床怀疑冠心病而冠状动脉造影结果正常的非冠心病者82例作为对照组。所有患者检测外周静脉血小板计数及淋巴细胞计数,并计算PLR。比较各组患者PLR水平,分析其与冠状动脉病变严重程度SYNTAX评分的相关性。结果 对照组PLR显著低于NSTEMI组,差异有统计学意义(P<0.01)。PLR与SYNTAX评分呈显著正相关(r=0.522,P<0.01)。Logistic回归分析显示PLR是NSTEMI患者冠状动脉病变高SYNTAX评分的独立预测因子(OR=1.018,95%CI:1.006~1.029,P<0.01)。结论 非ST段抬高型心肌梗死患者PLR水平显著升高,PLR与冠状动脉病变严重程度相关,可作为NSTEMI患者冠状动脉病变的简单预测方法。
血小板;淋巴细胞;心肌梗死
心肌梗死是冠状动脉粥样硬化性心脏病(冠心病)患者的主要致死原因之一,虽然强化药物治疗和介入治疗已明显降低非ST段抬高型心肌梗死(NSTEMI)的发病率和死亡率[1],但在冠状动脉造影中冠状动脉病变的严重程度是决定治疗策略的主要因素,炎症反应过程在冠状动脉粥样硬化的发生和发展中起到重要作用。炎症标志物的升高与冠状动脉病变的严重程度和预后相关。近年来,血小板/淋巴细胞比值(PLR)作为一种新的炎症标志物,在心血管疾病风险评估中的价值受到广泛的关注。现有研究表明,血小板/淋巴细胞比值与机体的炎症、动脉粥样硬化和血小板活化有关[2-4]。本研究旨在探讨PLR与NSTEMI患者冠状动脉严重程度的关系。
1 资料和方法
1.1 研究对象 选择2013年2月~2015年12月于阜阳市人民医院心血管内科住院的拟诊为NSTEMI并行冠状动脉造影检查的患者92例;同期该院临床怀疑冠心病而冠状动脉造影正常的非冠心病者82例作为对照组。NSTEMI的诊断根据美国心脏病学会/美国心脏协会(ACC/AHA)2014年诊断指南[5]。所有入选者排除其他系统疾病或药物治疗影响血细胞计数的患者,如:严重心力衰竭、血液系统疾病、肝肾功能不全、急性感染、外伤、手术、恶性肿瘤、免疫性疾病及接受糖皮质激素治疗患者。
1.2 评价指标及方法
1.2.1 一般资料采集及生化指标 采集患者年龄、性别、高血压、糖尿病、吸烟等一般资料;于入院次日凌晨空腹采集外周静脉血,测定包括血肌酐(sCr)、尿酸(UA)、丙氨酸氨基转移酶(ALT)、三酰甘油(TG)、总胆固醇(TC)、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C);检测白细胞(WBC)计数、血小板计数及淋巴细胞计数,并计算PLR=血小板/淋巴细胞。
1.2.2 SYNTAX评分 患者进行冠状动脉造影,按SYNTAX评分要求(病变部位、 狭窄程度、病变长度、有无钙化或血栓、是否为闭塞、成角或分叉病变等)将结果逐项输入SYNTAX官方网站( www.syntaxscore.com)的SYNTAX评分计算器(2.1版本),计算出SYNTAX分值,SYNTAX评分≥23分为高分组,代表冠状动脉病变较重,SYNTAX评分<23分为低分组,代表冠状动脉病变较轻。
1.2.3 评价指标 比较NSTEMI组和对照组间一般资料、PLR及生化指标的差异,分析SYNTAX评分与年龄、性别、高血压、糖尿病、吸烟、ALT、PLR、sCr、UA、TG、TC、HDL-C、LDL-C 的相关性。
1.3 统计学处理 应用SPSS 19.0 统计软件。计量资料用均数±标准差(±s)表示,组间比较采用t检验。计数资料用例数/百分比表示,组间比较采用χ2检验。以 SYNTAX评分≥23分为高分组,SYNTAX评分<23分为低分组。以SYNTAX评分为因变量,将各变量先进行单因素Logistic回归分析。将单因素分析结果得出的相关变量:年龄、sCr、PLR、LDL-C,HDL-C纳入多因素回归分析变量进行Logistic回归分析,求比值比(OR值)及95%置信区间,分析各因素与SYNTAX评分的独立相关性,以OR>1,表示该因素为危险因素,OR<1,表示该因素为保护因素。以P <0.05为差异有统计学意义。
2 结果
2.1 两组患者基线资料比较 NSTEMI组男性少于对照组,年龄、sCr、PLR、LDL-C 均高于对照组, HDL-C低于对照组,差异有统计学意义(P均<0.05)。两组吸烟、高血压、糖尿病比例,TG,TC,尿酸组间比较差异均无统计学意义(P均>0.05)(表1)。
2.2 各因素与SYNTAX评分的相关性分析 单因素回归分析显示年龄、HDL-C、LDL-C、PLR、sCr、ALT与SYNTAX评分有相关性。将年龄、HDL-C、LDL-C、PLR、sCr纳入多因素 Logistic回归分析,结果示PLR是NSTEMI患者冠状动脉病变高SYNTAX评分的独立预测因子(OR=1.018,95%CI:1.006~1.026,P<0.01)(表2)。
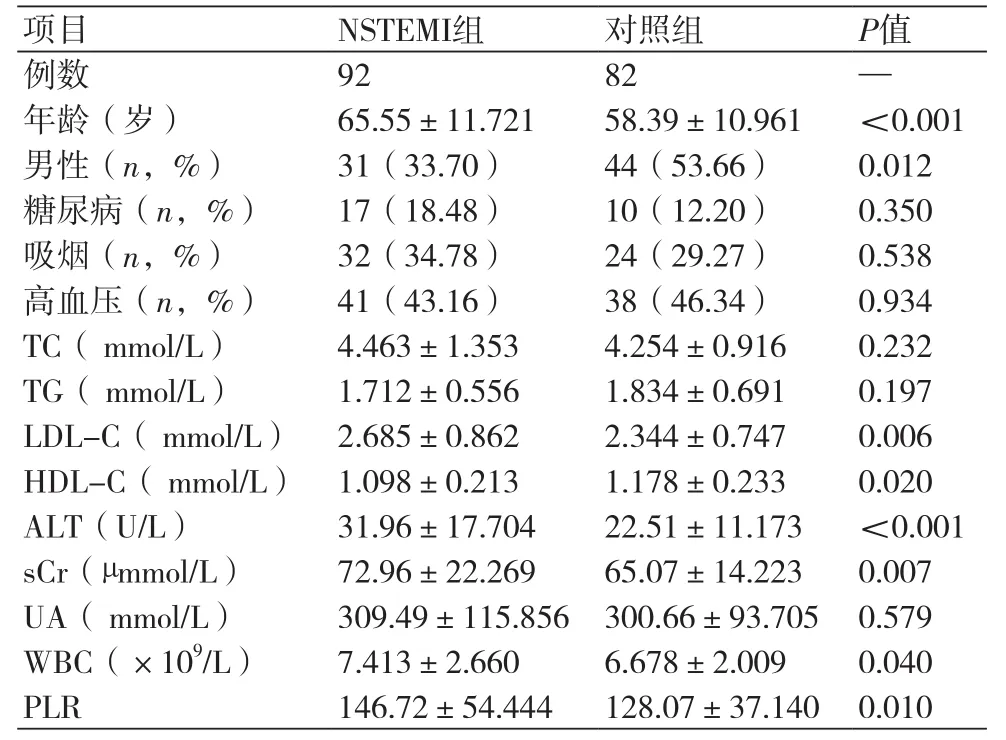
表1 NSTEMI组和对照组患者临床资料比较
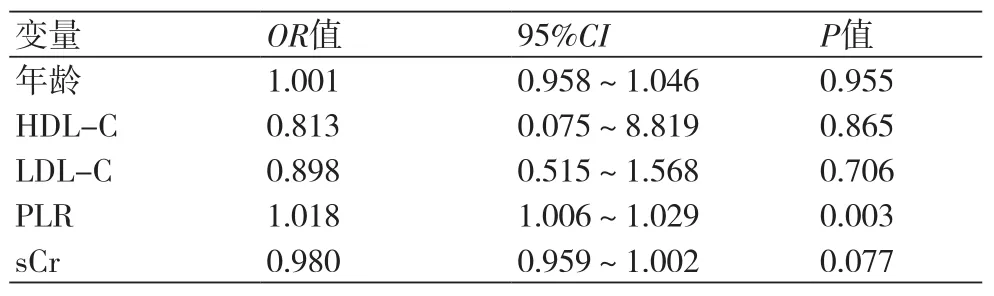
表2 冠状动脉病变程度SYNTAX评分的多因素Logistic回归分析
3 讨论
NSTEMI是冠心病最常见的发病形式之一,尽管NSTEMI患者的住院死亡率低于急性ST段抬高型心肌梗死,但6个月死亡率相同,4年死亡率是急性ST段抬高型心肌梗死的2倍[6-8]。因此,NSTEMI急性期的危险分层和长期随访对降低再发病率和死亡率至关重要。SYNTAX 评分是基于冠状动脉造影结果, 评价冠心病的复杂程度的指标。SYNTAX 评分有助于再灌注策略的选择,也可以预测冠心病的发病率和死亡率[9]。冠状动脉粥样硬化是一种慢性炎症性疾病,同时也是血栓性疾病[10,11]。血小板和淋巴细胞作为炎性细胞的重要组成部分,血小板-淋巴细胞的聚集在动脉粥样硬化的发生发展中起重要作用。在粥样斑块破裂或内皮损伤时,活化的血小板释放细胞因子和趋化因子诱导血栓形成,促进血栓性疾病的发生[12]。NSTEMI患者的冠状动脉通常不完全闭塞,冠状动脉内形成以血小板纤维蛋白原复合物为主要成分的白色血栓为主,血小板的活化在急性非ST抬高型心肌梗死的发生中可能起到更加重要的作用。本研究探讨了PLR与NSTEMI患者以SYNTAX 评分为代表的冠状动脉病变严重程度之间的关系。结果表明,PLR 在NSTEMI患者显著升高,NLR与 SYNTAX评分显著相关 (r=0.522,P<0.01)。通过多因素Logistic 回归分析显示 PLR是NSTEMI患者冠状动脉病变高SYNTAX评分的独立预测因子。
血小板/淋巴细胞比值(PLR)作为一种新的炎症标志物,高血小板、低淋巴细胞水平与不良心血管事件存在 一定关系[13-16]。PLR升高可在多种疾病中预测炎症和死亡率。血小板活化在冠心病和心血管疾病中起到重要作用[17],血小板计数基线水平升高是急性心肌梗死患者死亡的强力预测因子[18]。PLR升高增加非ST抬高型心肌梗死的长期死亡率[19],增加急性ST段抬高型心肌梗死患者急诊PCI的无复流现象和近、远期死亡率[20,21]。然而,既往的研究主要集中在PLR与心血管不良事件的关系方面。虽然最近也有关于PLR与冠状动脉Gensini积分的相关性研究。但PLR与NSTEMI冠状动脉SYNTAX评分的研究未见报道,这是本研究的新颖之处。鉴于该研究结果,通过测定PLR这种简单、经济的方法,对预测NSTEMI患者的冠状动脉病变程度,识别高危患者,从而选择更加积极有效的治疗策略有一定的临床价值。但该研究样本量相对偏少,且本研究属回顾性分析,不同组间一般资料及生化指标存在较多差异,有一定局限性,有待更大样本量的研究进一步探索PLR在NSTEMI的意义。
[1] Terkelsen CJ,Lassen JF,Norgard BL,et al. Mortality rates in patients with ST-elevation vs. Non-STelevation acute myocardial infarcton:observation from an unselected cohort[J]. Eur Heart J,2005,26(1):18-26.
[2] Balta S,Demirkol S,Kucuk U. The platelet lymphocyte ratio may be useful inflammatory indicator in clinical practice[J]. Hemodial Int,2013,17(4):668-9.
[3] Jennings LK. Mechanisms of platelet activation: Need for new strategies to protect against platelet-mediated atherothrombosis[J]. Thromb Haemost,2009,102(2):248-57.
[4] Ayca B,Akin F,Celik O,et al. Platelet to lymphocyte ratio as a prognostic marker in primary percutaneous coronary intervention[J]. Platelets,2014,26(7):638-44.
[5] Amsterdam EA,Wenger NK,Brindis RG,et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines[J]. Circulation,2014,130(25): 2354-94.
[6] Yeh RW,Sidney S,Chandra M,et al. Population trends in the incidence and outcomes of acute myocardial infarction[J]. N Engl J Med,2010,362(23): 2155-65.
[7] Mandelzweig L,Battler A,Boyko V,et al. The second Euro Heart Survey on acute coronary syndromes: Characteristics,treatment,and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004[J]. Eur Heart J,2006,27(19):2285-93.
[8] Terkelsen CJ,Lassen JF,Nørgaard BL,et al. Mortality rates in patients with ST-elevation vs. non-STelevation acute myocardial infarction: observations from an unselected cohort[J]. Eur Heart J,2005,26(1):18-26.
[9] Van Gaal WJ,Ponnuthurai FA,Selvanayagam J,et al. The Syntax score predicts peri-procedural myocardial necrosis during percutaneous coronary intervention[J]. Int J Cardiol,2009,135(1): 60-5.
[10] Lievens D,von Hundelshausen P. Platelets in atherosclerosis[J]. Thromb Haemost,2011,106(5):827-38.
[11] Libby P,Ridker PM,Hansson GK. Progress and challenges in translating the biology of atherosclerosis[J]. Nature,2011,473(7347): 317-25.
[12] Demirtas S,Karahan O,Yazici S,et al. The relationship between complete blood count parameters and Fontaine’s Stages in patients with peripheral arterial disease[J]. Vascular,2014,22(6):427-31.
[13] Nagasawa A,Matsuno K,Tamura S,et al. The basis examination of leukocyte-platelet aggregates with CD45 gating as a novel platelet activation marker[J]. Int J Lab Hematol,2013,35(5):534-41.
[14] Spectre G,Zhu L,Ersoy M,et al. Platelets selectively enhance lymphocyte adhesion on subendothelial matrix under arterial flow conditions[J]. Thromb Haemost,2012,108(2):328-37.
[15] Zamora C,Canto E,Nieto JC,et al. Functional consequences of platelet binding to T lymphocytes in inflammation[J]. J Leukoc Biol,2013,94(3):521-9.
[16] Hu H,Zhu L,Huang Z,et al. Platelets enhance lymphocyte adhesion and infiltration into arterial thrombus[J]. Thromb Haemost,2010,104(6): 1184-92.
[17] Kurtul A,Yarlioglues M,Murat SN,et al. Usefulness of the plateletto-lymphocyte ratio in predicting angiographic reflow after primary percutaneous coronary intervention in patients with acute STsegment elevation myocardial infarction[J]. Am J Cardiol,2014,114(3):342-7.
[18] Nikolsky E,Grines CL,Cox DA,et al. Impact of baseline platelet count in patients undergoing primary percutaneous coronary intervention in acute myocardial infarction (from the CADILLAC trial) [J]. Am J Cardiol,2007,99(8):1055-61.
[19] Azab B,Shah N,Akerman M,et al. Value of platelet/ lymphocyte ratio as a predictor of all-cause mortality after non-STelevation myocardial infarction[J]. J Thromb Thrombolys,2012,34(3):326-34.
[20] Çiçek G,Açkgoz SK,Bozbay M,et al. Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio combination can predict prognosis in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. Angiology,2014,66(5):441-7.
[21] Yildiz A,Yuksel M,Oylumlu M,et al. The utility of the plateletlymphocyte ratio for predicting no reflow in patients with ST-segment elevation myocardial infarction[J]. Clin Appl Thromb Hemost,2015,21 (3):223-8.
本文编辑:张磊,姚雪莉
Correlation between platelet and lymphocyte ratio and severity of coronary artery lesions in patients withnon-ST-segment elevation myocardial infarction
GUO Ying-jie*, NING Bin, GE Hui-juan, ZHUANG Xiaosai.*Department of Cardiovascular Diseases, People's Hospital of Fuyang City, Fuyang 236001, China.
GUO Ying-jie, E-mail: 478595575@qq.com
Objective To study the correlation between platelet and lymphocyte ratio (PLR) and severity of coronary artery lesions in patients with non-ST-segment elevation myocardial infarction (NSTEMI). Methods NSTEMI patients (n=92) were chosen as NSTEMI group from the Department of Cardiovascular Diseases of People’s Hospital of Fuyang City from Feb. 2013 to Dec. 2015, and given examination of coronary angiography (CAG) and the results were graded by using SYNTAX scoring system. At the same time, the patients with suspected coronary heart disease and normal CAG results (n=82) were chosen as control group. The counts of peripheral venous platelet and lymphocytes were detected and PLR was calculated in all patients. The level of PLR was compared between 2 groups, and correlation between PLR and SYNTAX scores of severity of coronary artery lesion was analyzed. Results The level of PLR was significantly lower in control group than that in NSTEMI group (P<0.01), and PLR was positively correlated to SYNTAX scores (r=0.522, P<0.01). Logistic regression analysis showed that PLR was an independent predictive factor for higher SYNTAX scores of coronary artery lesions in NSTEMI patients (OR=1.018, 95%CI: 1.006-1.029, P<0.01). Conclusion The level of PLR increases significantly, and PLR is correlated to the severity of coronary artery lesions in NSTEMI patients, which can be taken as a simple method for predicting coronary artery lesions.
Platelet; Lymphocyte; Myocardial infarction
R541.4
A
1674-4055(2017)05-0600-03
1236001 阜阳,阜阳市人民医院心血管内科
郭英杰,E-mail:478595575@qq.com
10.3969/j.issn.1674-4055.2017.05.24
