Electroacupuncture at Fengchi (GB20) inhibits calcitonin gene-related peptide expression in the trigeminovascular system of a rat model of migraine
2017-06-05LuopengZhaoLuLiuPeiPeiZhengyangQuYupuZhuLinpengWang
Luo-peng Zhao, Lu Liu Pei Pei, Zheng-yang Qu Yu-pu Zhu, Lin-peng Wang
1 Department of Acupuncture and Moxibustion, Beijing Hospital of Traditional Chinese Medicine, Capital Medical University, Beijing, China
2 Beijing University of Chinese Medicine, Beijing, China
3 The First Affiliated Hospital of Anhui University of Chinese Medicine, Hefei, Anhui Province, China
Electroacupuncture at Fengchi (GB20) inhibits calcitonin gene-related peptide expression in the trigeminovascular system of a rat model of migraine
Luo-peng Zhao1,2, Lu Liu1, Pei Pei3, Zheng-yang Qu1, Yu-pu Zhu1,2, Lin-peng Wang1,*
1 Department of Acupuncture and Moxibustion, Beijing Hospital of Traditional Chinese Medicine, Capital Medical University, Beijing, China
2 Beijing University of Chinese Medicine, Beijing, China
3 The First Affiliated Hospital of Anhui University of Chinese Medicine, Hefei, Anhui Province, China
How to cite this article:Zhao LP, Liu L, Pei P, Qu ZY, Zhu YP, Wang LP (2017) Electroacupuncture at Fengchi (GB20) inhibits calcitonin gene-related peptide expression in the trigeminovascular system of a rat model of migraine. Neural Regen Res 12(5):804-811.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Funding:This study was supported by the National Natural Science Foundation of China, No. 81603683; a grant from the National Basic Research Program of China, No. 2014CB543203; a grant from the Beijing Municipal Science & Technology Commission of China, No. Z171100001017033.
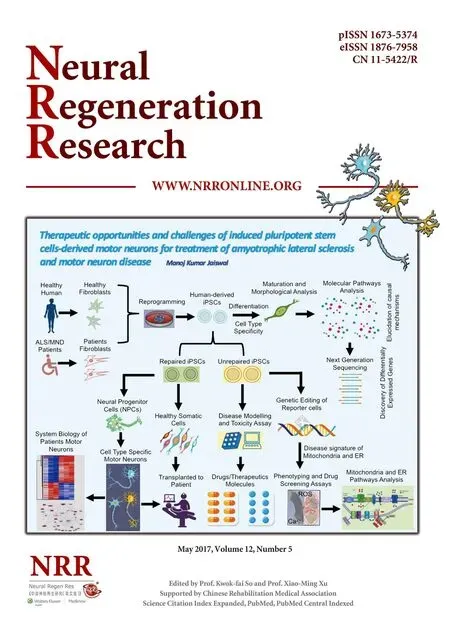
Graphical Abstract

Electroacupuncture treatment can ameliorate migraine by inhibiting calcitonin gene-related peptide expression
Most migraine patients suffer from cutaneous allodynia; however, the underlying mechanisms are unclear. Calcitonin gene-related peptide (CGRP) plays an important role in the pathophysiology of migraine, and it is therefore, a potential therapeutic target for treating the pain. In the present study, a rat model of conscious migraine, induced by repeated electrical stimulation of the superior sagittal sinus, was established and treated with electroacupuncture atFengchi(GB20) (depth of 2–3 mm, frequency of 2/15 Hz, intensity of 0.5–1.0 mA, 15 minutes/day, for 7 consecutive days). Electroacupuncture at GB20 significantly alleviated the decrease in hind paw and facial withdrawal thresholds and significantly lessened the increase in the levels of CGRP in the trigeminal ganglion, trigeminal nucleus caudalis and ventroposterior medial thalamic nucleus in rats with migraine. No CGRP-positive cells were detected in the trigeminal nucleus caudalis or ventroposterior medial thalamic nucleus by immunofluorescence. Our findings suggest that electroacupuncture treatment ameliorates migraine pain and associated cutaneous allodynia by modulating the trigeminovascular system ascending pathway, at least in part by inhibiting CGRP expression in the trigeminal ganglion.
nerve regeneration; electroacupuncture; migraine; calcitonin gene-related peptide; cutaneous allodynia; anti-nociceptive; Fengchi; trigeminal ganglion; neural regeneration
Introduction
Migraine is a common primary headache disorder that is characterized by recurrent, throbbing, unilateral headaches, and affects 14.7% of the population worldwide (Vos et al., 2012; Headache Classification Committee of the International Headache Society, 2013). Most migraines are accompanied by cutaneous allodynia, which is an altered sensory perception to innocuous stimuli (Lovati et al., 2009). According to the Global Burden of Disease Study in 2010, migraine ranked as the third most prevalent and seventh most disabling disease worldwide (Vos et al., 2012). Current anti-migraine drugs, including non-prescription painkillers, nonsteroidal anti-inflammatory drugs, triptans and ergot alkaloids, are unable to fully meet the needs of migraine sufferers because of their suboptimal efficacy, adverse effects, and contraindications (Reddy, 2013).
Electroacupuncture (EA) is a promising complementary strategy for treating migraine. Some reviews have suggested that acupuncture is a treatment choice for migraineurs, with few adverse events, which could be used as a supplement to other non-pharmacologic treatment options (Endres et al., 2007; Linde et al., 2016). However, the mechanisms underlying the analgesic effect of EA on migraine are unknown. It is generally thought that the activation and sensitization of trigeminovascular system nociceptive pathways are responsible for migraine headaches and cutaneous allodynia (Pietrobon and Moskowitz, 2013). A recent study demonstrated that EA atFengchi(GB20) exerts antinociceptive effects by modulating serotonin (Liu et al., 2016). Advances in the understanding of the function of calcitonin gene-related peptide (CGRP) in trigeminovascular system nociceptive pathways suggest that CGRP is a promising target for migraine therapy (Pietrobon and Moskowitz, 2013). CGRP-targeting drugs developed for migraine, such as CGRP receptor antagonists and CGRP-blocking antibodies, were shown to be efficacious in treating migraine attacks in clinical trials (Russo, 2015).
We hypothesized that EA treatment at GB20 might modulate CGRP levels in the trigeminal ganglion, trigeminal nucleus caudalis and ventroposterior medial thalamic nucleus of the trigeminovascular system ascending pathway, and alleviate cutaneous allodynia. To test this hypothesis, an experimental rat model of migraine was established by repeated electrical stimulation of the superior sagittal sinus, which mimics migraine headache and cutaneous allodynia. Then, we evaluated cutaneous allodynia using electronic von Frey anesthesiometry and CGRP expression in the trigeminovascular system by western blot assay and immunofluorescence to explore the mechanisms underlying the effects of EA treatment on migraine and cutaneous allodynia.
Materials and Methods
Animals
This study was approved by the Beijing Institutional Review Board for Animal Experiments (Use Committee of Capital Medical University, Beijing; Approval number: AEEI 2015-075). Surgeries were performed under anesthesia, and all possible efforts were made to minimize suffering.
Forty male 6-week-old, specific-pathogen-free Sprague Dawley rats (Vital River Laboratories, No. 11400700103582, Beijing, China), weighing 210 ± 10 g, were used in this study. Rats were individually maintained in a climate-controlled laboratory environment (room temperature, 23 ± 2°C; humidity, 50 ± 10%) on a 12-hour light/dark cycle with unlimited access to water and food. The rats were acclimated to the new environment for 1 week before undergoing brain surgery to implant the electrodes required for electrical stimulation.
Group assignment
After the acclimation period, 40 animals were randomly divided into the following four groups (n= 10): a control group, which only received electrode implantation; a model group, which only received electrical stimulation of the superior sagittal sinus; an EA group, which received EA at GB20 after electrical stimulation of the superior sagittal sinus; and a non-acupuncture point electroacupuncture (NA) group, which received EA at a distant non-acupuncture point (approximately 10 mm above the iliac crest) after electrical stimulation of the superior sagittal sinus (Li et al., 2015). The experiment began on the first day after recovery and lasted 7 days. Three sessions of electrical stimulation were given to the EA, NA and model groups with a stimulator (YC-2 stimulator; Chengdu Instrument Factory, Chengdu, Sichuan Province, China) every other day (on days 1, 3 and 5). From day 1 to day 7, the EA and NA groups received EA after electrical stimulation for a total of seven sessions. The number of animals used in this study was 10 per group, estimated according to a power calculation described in a previous study (Gao et al., 2014). A diagram of the experimental protocol is shown in Figure 1.
Establishment of the rat model of conscious migraine

Figure 1 Diagram of the experimental protocol.

Table 1 Withdrawal thresholds in a rat migraine model treated with EA

Figure 2 CGRP protein expression levels in the trigeminovascular system assessed by western blot assay in a rat model of migraine treated with EA.
As described in a previous study (Pei et al., 2016), rats were anesthetized with an intraperitoneal injection of 60 mg/kg pentobarbital sodium (Sigma-Aldrich, St. Louis, MO, USA). Two holes (1 mm in diameter) were drilled in the midline suture of the skull with a saline-cooled drill (78001; RWD Life Science, Shenzhen, Guangdong Province, China) (Dong et al., 2011). One hole was located 4 mm anterior to the bregma, and the other was 6 mm posterior to the bregma. The cranial holes were located over the dura mater around the superior sagittal sinus. Two tailored electrode fixtures (Beijing Jiandeer, Beijing, China) were placed into the cranial holes such that they were contacting the superior sagittal sinus. A pair of screws (M1.4 × 2.8 mm) were implanted into the screw holes of each electrode fixture to stabilize the electrodes and then covered with dental cement (Shanghai New Century Dental Materials, Shanghai, China). To prevent clogging, the obturator was inserted into the external terminal of the electrode. The operation was performed under a surgical microscope. Penicillin (0.04 million IU/100 g; Harbin Pharmaceutical Group, China) was administered intramuscularly to prevent infection. All rats had a 7-day recovery period before the experiments began.
Before dural electrical stimulation, each rat was placed in a transparent cage (diameter, 40 cm; height, 17.5 cm) and allowed to habituate for 20 minutes. The obturator was removed from the electrode fixtures, and a delivery electrode tip that was connected to the current source output of the electrical stimulator was inserted. Based on previous studies, dural electrical stimuli, which consisted of 0.5-ms monophasic square-wave pulses of 1.8–2.0 mA (intensity) and 20 Hz (frequency) were given to the rats in the EA, NA and model groups for a 15-minute period every other day for a total of three sessions (Pei et al., 2016). Rats in the control group were connected to the stimulator, but were given no stimulation.
EA at GB20


Figure 3 Immunofluorescence distribution of CGRP-positive cells in the trigeminal ganglion of a rat model of migraine treated with EA.
Each rat was consciously placed into a tailored fixture that restricted movement and exposed the head and neck. According to the WHO Standard Acupuncture Point Locations (World Health Organization Regional Office for the Western Pacific, 2008), GB20 is located “in the anterior region of the neck, inferior to the occipital bone, in the depression between the origins of sternocleidomastoid and the trapezius muscles”. The anatomical location of GB20 in rats is similar to that in humans—3 mm lateral to the midpoint of a line joining the two ears at the back of the head (Siu et al., 2005). For rats in the EA group, a pair of stainless steel acupuncture needles (diameter, 0.25 mm; length, 25 mm; Suzhou Medical Appliance Factory, Suzhou, Jiangsu Province, China) were inserted into GB20 to a depth of 2–3 mm in the direction of the opposite eye, bilaterally. The needle handle was then connected to an electrical stimulator (Han’s acupuncture point nerve stimulator HNAS-200E; Nanjing, Jiangsu Province, China) for 15 minutes/day. EA was applied at a frequency of 2/15 Hz (amplitude-modulated wave) and an intensity of 0.5–1.0 mA (depending on the reaction of the rat) (Pei et al., 2016). For rats in the NA group, needles were inserted bilaterally at distant non-acupuncture points (approximately 10 mm above the iliac crest) to a depth of 2–3 mm, and EA was performed with the same parameters as in the EA group. Animals in the control and model groups were similarly placed into fixtures for 20 minutes, but no acupuncture was applied.
Behavioral testing of the allodynia response
An electronic von-Frey anesthesiometer (Model 2390, IITC Life Science, Woodland Hills, CA, USA) was used to test facial and hind paw withdrawal thresholds. The von Frey anesthesiometry probe was applied vertically to the skin of the face or hind paw until the rat made an escape movement. When the escape response occurred, the maximum force was recorded as the withdrawal threshold by the device. All measurements of withdrawal threshold were made by the same operator, who was blinded to the reading until an escape response was elicited (Moore et al., 2013).
Facial allodynia
Rats were placed in a tailored plastic tube restraint (length, 25 cm; inner diameter, 8 cm) with a mesh inlay at the front, so that the periorbital region was easily accessed. After a 30-minute habituation period, the von Frey anesthesiometry tip was applied to the periorbital region with steady vertical pressure until an escape movement occurred. A total of three trials were completed with 30-second intervals. The mean value of the trials was considered the withdrawal threshold.
Hind paw allodynia
Rats were placed separately under transparent plastic boxes on an elevated mesh platform for 30 minutes. The von Frey anesthesiometry probe was inserted through the mesh to prod the hind paw until the paw was withdrawn from the tip or lifted off the mesh floor. The assay was performed three times with 30-second intervals. The mean value of the trials was used to determine the withdrawal threshold.
Western blot assay
Rats were anesthetized with 10% chloral hydrate (15 mL/kg,intraperitoneally), and the brains and trigeminal ganglia were rapidly removed, frozen in liquid nitrogen, and stored at −80°C until dissection. A week later, the trigeminal nucleus caudalis and ventroposterior medial thalamic nucleus were dissected on a frozen microtome. Using a magnifying glass, bilateral tissue punches from the ventroposterior medial thalamic nucleus and trigeminal nucleus caudalis regions were taken from frontal brain sections (300 μm) with a stainless steel cannula (inner diameter, 1,000 μm) and pooled (Paxinos and Watson, 1998). Samples were placed into 1.8-mL prechilled tubes and stored at −80°C. For western blot assay, total tissue samples from different regions were collected and homogenized in radioimmunoprecipitation assay buffer (70-WB019; MultiSciences, Hangzhou, China) with an ultrasonic cell crusher. The homogenate was centrifuged at 13,000 ×gfor 15 minutes at 4°C, and 300 μL of the supernatant was collected and stored at −20°C until analysis.
The protein concentration of the samples was determined by bicinchoninic acid assay using the Micro BCA Protein Assay Kit (Thermo Scientific, Rockford, IL, USA). Proteins were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (12% gradient gels), using 50 µg of protein per well, and then transferred to a polyvinylidene difluoride membrane. The polyvinylidene difluoride blots were blocked in 10% skim milk for 1 hour at room temperature. Membranes were incubated with either a rabbit anti-CGRP polyclonal antibody (Ab139264, Abcam, Cambridge, UK; 1:1,000) or a mouse β-actin polyclonal antibody (4967 CST, Cell Signaling Technology, Boston, MA, USA; 1:1,000) overnight at 4°C. Horseradish peroxidase-conjugated secondary antibody, goat anti-rabbit IgG (H+L) (111-035-003, Jackson ImmunoResearch Laboratories, West Grove, PA, USA; 1:10,000) or goat anti-mouse IgG (H+L) (115-035-003, Jackson ImmunoResearch Laboratories; 1:10,000), was diluted in 10% skim milk/Tris-buffered saline/Tween 20 (TBST) prior to use at room temperature. All between-incubation washes were in TBST. Signals were detected using the enhanced chemiluminescence kit (WBKLS0500, Millipore Corporation, Billerica, MA, USA) and Kodak film (Eastman Kodak, Rochester, NY, USA). The integrated optical density values of the detected proteins were analyzed using Quantity One software (Bio-Rad Laboratories, Hercules, CA, USA). CGRP was expressed as a ratio to β-actin (the loading control).
Immunofluorescence analysis
Rats were anesthetized with an intraperitoneal injection of 10% chloral hydrate (15 mL/kg) and perfused through the ascending aorta with 100 mL of 0.1 M PBS, followed by 500 mL of 4% paraformaldehyde in phosphate buffered saline (PBS). Brains and trigeminal ganglia were removed and post fixed in 4% paraformaldehyde/PBS overnight at 4°C, and then transferred to 30% sucrose/PBS for cryopreservation and incubated for 72 hours. A week later, the trigeminal ganglia and brains were sectioned coronally (25-mm-thick slices) through the thalamus and trigeminal nucleus caudalis with a cryostat (CM3050S, Leica, Wetzlar, Germany). Sections were incubated with a rabbit anti-CGRP polyclonal antibody (ab81887, Abcam, Cambridge, UK; 1:200) overnight at 4°C, and then with Alexa 488 goat anti-rabbit secondary antibody (111-545-003, Jackson ImmunoResearch Laboratories; 1:500) for 2 hours at room temperature. The sections were then mounted, dehydrated, and cover-slipped with anti-fade reagent (AR1109; Boster Bioengineering, Wuhan, China). Sections were imaged using a Leica DM5500 B semi-automatic light microscope, and cells were counted on a grid using the 40× objective lens. Cell counts per 100 µm2(CGRP-positive cell density) in the trigeminal ganglion, trigeminal nucleus caudalis and ventroposterior medial thalamic nucleus were determined by an observer blinded to the groupings using ImageJ software. Anatomical boundaries were determined according to a rat brain atlas (Paxinos and Watson, 1998).
Statistical analysis
Data are shown as the mean ± SD. Withdrawal thresholds were analyzed using repeated measures analysis of variance. All other data were analyzed using one-way analysis of variance using SPSS v12.0 software (SPSS, Chicago, IL, USA).Post-hoctesting was performed using Bonferroni (homogeneity of variance) or Tamhane (heterogeneity of variance) test. Differences withPvalues less than 0.05 were considered significant.
Results
EA inhibited the reduction in facial and hind paw withdrawal thresholds in a rat model of conscious migraine
To evaluate the effect of EA at GB20 on cutaneous allodynia in our rat model, von Frey anesthesiometry was used to assess facial and hind paw withdrawal thresholds. For the facial withdrawal threshold, there were no significant differences in the baseline among the four groups (P> 0.05; Table 1). Repetitive dural electrical stimulation significantly decreased the facial withdrawal threshold of the model group compared with the control group (P< 0.001). The withdrawal threshold was significantly higher in the EA group than in the model group (P< 0.001). The facial withdrawal threshold in the NA group did not differ significantly from that in the model group (P> 0.05).
For the hind paw withdrawal threshold, no significant difference was observed at baseline among the four groups (P> 0.05; Table 1). However, after repeated dural electrical stimulation, the hind paw withdrawal threshold was significantly lower in the model group than in the control group (P< 0.001). The hind paw withdrawal threshold was significantly higher in the EA group than in the model group, suggesting that EA at GB20 attenuates the decrease in withdrawal threshold induced by dural electrical stimulation (P< 0.001). The hind paw withdrawal thresholds in the NA and model groups did not differ significantly (P> 0.05).
EA decreased CGRP levels in the trigeminal ganglion, trigeminal nucleus caudalis and ventroposterior medial thalamic nucleus in a rat model of conscious migraine
Western blot assay for CGRP
To investigate the effect of EA on CGRP levels, western blotassay was performed to examine the levels of CGRP in the trigeminal ganglion, trigeminal nucleus caudalis, and ventroposterior medial thalamic nucleus in all groups. In all three regions examined, CGRP protein levels in brain lysates from the model group (after repeated dural electrical stimulation) were significantly higher than those in the control group (n= 5;P< 0.001). In contrast, the EA group had significant lower CGRP protein levels compared with the model group (P< 0.05), while the levels in the NA group did not differ significantly compared with the model group (P> 0.05; Figure 2).
Immunofluorescence analysis of CGRP-positive cells
In the trigeminal ganglion, immunofluorescence analysis revealed that the model group contained significantly more CGRP-positive cells than the control group (n= 5;P< 0.10). The mean number of CGRP-positive cells in the EA group was significantly lower than that in the model group (P< 0.05), whereas the numbers of CGRP-positive cells in the NA and model groups did not differ (P> 0.05). No significant difference was observed between the control and EA groups (P> 0.05; Figure 3). However, no CGRP-positive cells were detected in the trigeminal nucleus caudalis or ventroposterior medial thalamic nucleus (data not shown).
Discussion
The current findings show that EA at GB20 alleviates cutaneous allodynia in a recurrent migraine model and reduces CGRP levels in the trigeminovascular system ascending pathway. CGRP has been considered a potential new therapeutic target for migraine. Our findings suggest that EA relieves migraine pain and cutaneous allodynia by reducing CGRP levels.
GB20 and migraine
In this study, we chose GB20 to treat migraine and cutaneous allodynia. According to traditional acupuncture theory, migraine is related to dysfunction of the Gallbladder Meridian (Wu, 2009). GB20 is a point in the Gallbladder Meridian located near the region of migraine headache (World Health Organization Regional Office for the Western Pacific, 2008). Therefore, stimulation of GB20 should modulate the function of the Gallbladder Meridian and relieve migraine headache. Indeed, GB20 is one of the most commonly used acupuncture points for migraine in clinical practice and clinical trials (Zheng et al., 2010; Linde et al., 2016).
Trigeminovascular neurons and migraine
Activation and sensitization of the trigeminovascular pain pathway are implicated in the pathophysiology of migraine and cutaneous allodynia (Pietrobon and Moskowitz, 2013). In the present study, we focused on three groups of trigeminovascular neurons in the trigeminovascular system ascending pathway (trigeminal ganglion, trigeminal nucleus caudalis and ventroposterior medial thalamic nucleus) (Noseda and Burstein, 2013). The trigeminal ganglion neurons have sensory fibers that innervate meningeal vessels and afferent projections which synapse with the trigeminal nucleus caudalis neurons. The trigeminal nucleus caudalis conveys signals from the trigeminal ganglion, while sensory signals from the trigeminal nucleus caudalis and extracephalic skin converge onto ventroposterior medial thalamic nucleus neurons. The nociceptive input is transmitted to cortical areas where the perception of the migraine headache and cutaneous allodynia is recognized (Pietrobon and Moskowitz, 2013).
EA at GB20 significantly alleviated dural electrical stimulation-induced cutaneous allodynia
Approximately two-thirds of migraineurs suffer from cutaneous allodynia after migraine attacks, which is characterized by a decreased threshold for the perception of pain induced by non-noxious stimuli (Burstein et al., 2000; Lipton et al., 2008; Louter et al., 2013). Studies have shown that sensitization of the trigeminovascular system can lead to cephalic and extracephalic allodynia (Burstein et al., 1998, 2010). Facial and hind paw withdrawal threshold is a commonly used indicator of mechanical allodynia in migraine research (Romero-Reyes and Ye, 2013). In this study, the decreased withdrawal thresholds in the face and hind paw mimicked cutaneous allodynia.
Central sensitization of trigeminovascular neurons is thought to be the main mechanism of cutaneous allodynia (Bernstein and Burstein, 2012). Accumulating evidence indicates that cephalic cutaneous allodynia results from sensitization of trigeminal nucleus caudalis neurons, while extracephalic cutaneous allodynia represents sensitization of ventroposterior medial thalamic nucleus neurons (Pietrobon and Moskowitz, 2013). In this study, dural electrical stimulation decreased the facial and hind paw withdrawal thresholds, which mimic cephalic and extracephalic cutaneous allodynia, respectively. After sensitization, these neurons exhibited hypersensitivity to cephalic or extracephalic stimuli. EA at GB20 significantly ameliorated these reductions in withdrawal threshold, whereas EA at a distant, non-acupuncture point (NA group) failed to do so, indicating that improvement of these behavioral measures was specific to EA treatment at GB20.
EA at GB20 decreased CGRP levels in the trigeminal ganglion, trigeminal nucleus caudalis and ventroposterior medial thalamic nucleus
In the peripheral trigeminovascular system, CGRP is involved in the activation of meningeal nociceptors during migraine attacks. Neurogenic inflammation is thought to be a key mechanism in the activation and sensitization of perivascular meningeal afferents (Uddman et al., 1985). Accumulating evidence indicates that CGRP plays an important role in this inflammatory response. CGRP directly dilates the meningeal arteries (Brain and Grant, 2004), triggers the release of pro-inflammatory substances from mast cells, and increases substance P release to promote inflammation (Zhang et al., 2007; Lennerz et al., 2008). In the trigeminovascular system, cell bodies in the trigeminal ganglion are the main source of CGRP (Uddman et al., 1985; Durham, 2006). Our results suggest that repeated dural electrical stimulation significantly in-creases CGRP levels and the number of CGRP-positive cells in the trigeminal ganglion. EA at GB20, but not at the NA point, led to a decrease in CGRP expression and the number of CGRP-positive cells within the trigeminal ganglion, suggesting that it inhibits CGRP-mediated inflammation.
In the central trigeminovascular system, CGRP is a neuromodulator at second- and third-order trigeminovascular neurons that are involved in central sensitization (Raddant and Russo, 2011). In the trigeminal nucleus caudalis, CGRP is released from the central terminals of trigeminal ganglion neurons (Jenkins et al., 2004; Fischer, 2010). Expression studies have shown CGRP immunoreactivity in presynaptic afferent terminals, but not in the neuronal bodies, and CGRP receptor components (RAMP1 and CLR) have been detected in the spinal trigeminal tract region (Eftekhari and Edvinsson, 2011). Furthermore, microiontophoresis of α-CGRP excites some trigeminal nucleus caudalis neurons, and CGRP receptor antagonists block the enhanced nociceptive trigeminovascular transmission in the trigeminal nucleus caudalis (Storer et al., 2004; Summ et al., 2010). In the ventroposterior medial thalamic nucleus, the presence of CGRP receptors has been demonstrated, and microiontophoresis of CGRP increases the spontaneous firing of ventroposterior medial thalamic nucleus neurons, which can be suppressed by the CGRP receptor antagonist CGRP 8–37 (Summ et al., 2010).
In present study, repeated dural electrical stimulation significantly increased CGRP levels in the trigeminal nucleus caudalis and ventroposterior medial thalamic nucleus, as shown by western blot assay. These increases were largely blocked by EA at GB20. Consistent with previous studies, we did not detect CGRP-positive cells in the trigeminal nucleus caudalis or ventroposterior medial thalamic nucleus using immunofluorescence.
CGRP in the ventroposterior medial thalamic nucleus may come from the trigeminal ganglion
It has been demonstrated that some CGRP in the trigeminal nucleus caudalis is released from the trigeminal ganglion; however, the origin of CGRP in the ventroposterior medial thalamic nucleus is unclear (Eftekhari and Edvinsson, 2011). A previous study showed that inflammatory soup-induced CGRP release into the jugular vein and cerebrospinal fluid is mainly derived from primary trigeminal afferents (Hoffmann et al., 2012). Plasma CGRP is unlikely to reach the ventroposterior medial thalamic nucleus because of poor penetration of the blood-brain barrier (Edvinsson, 2015a). Therefore, it is likely that ventroposterior medial thalamic nucleus neurons are modulated by CGRP in the cerebrospinal fluid. Moreover, the majority of CGRP mRNA is synthesized in the trigeminal ganglion, which is the major source of CGRP in the trigeminovascular system (Durham, 2006; Bhatt et al., 2014).
CGRP is a potential new therapeutic target for migraine treatment (Edvinsson, 2015a). Previous studies have shown that pain relief is accompanied by normalization of CGRP levels, and CGRP-targeting drugs are effective in clinical trials, although the sites of action are still unclear (Edvinsson, 2015b). In this study, EA at GB20 significantly reduced CGRP levels in the trigeminovascular system ascending pathway and reversed the hypersensitivity caused by dural electrical stimulation. EA at a non-acupuncture point failed to normalize CGRP levels and the withdrawal threshold. Thus, the anti-migraine effect of EA appears to be specific to GB20.
Here, we observed an inhibitory effect of EA at GB20 on CGRP expression in the trigeminal ganglion. However, the underlying mechanism is still unclear. Previous studies have demonstrated that CGRP expression within the trigeminal ganglion is involved in the activation of MAPK signaling pathways (Durham and Russo, 2003; Bellamy et al., 2006; Bowen et al., 2006; Dieterle et al., 2011). Furthermore, the MAPK signaling pathway has been shown to play a role in acupuncture-induced analgesia (Fang et al., 2013; Du et al., 2014; Park et al., 2014). Therefore, it is possible that the inhibition by EA of CGRP expression in the trigeminal ganglion modulates the MAPK signaling pathway. Uncovering the cell and molecular mechanisms within the trigeminal ganglia that underlie the EA-induced analgesic effect will require additional research.
In conclusion, EA treatment ameliorates migraine pain and the associated cutaneous allodynia by inhibiting CGRP expression in the trigeminal ganglion to modulate the trigeminovascular system ascending pathway. A limitation of our study is that we used withdrawal thresholds to evaluate sensitization of trigeminovascular system neurons without direct evidence of sensitization. Additional CGRP receptor and signaling pathway studies are required to elucidate the mechanisms underlying the effects of EA on migraine.
Author contributions:LPZ and PP conducted the experiments. LPZ, PP and LL interpreted the data and wrote the manuscript. ZYQ and YPZ revised the manuscript. LPW supervised the research program and contributed to integration of the research team. All authors have read and approved the final manuscript.
Conflicts of interest:None declared.
Plagiarism check:This paper was screened twice using CrossCheck to verify originality before publication.
Peer review:This paper was double-blinded and stringently reviewed by international expert reviewers.
Bellamy J, Bowen EJ, Russo AF, Durham PL (2006) Nitric oxide regulation of calcitonin gene-related peptide gene expression in rat trigeminal ganglia neurons. Eur J Neurosci 23:2057-2066.
Bernstein C, Burstein R (2012) Sensitization of the trigeminovascular pathway: perspective and implications to migraine pathophysiology. J Clin Neurol 8:89-99.
Bhatt DK, Gupta S, Ploug KB, Jansen-Olesen I, Olesen J (2014) mRNA distribution of CGRP and its receptor components in the trigeminovascular system and other pain related structures in rat brain, and effect of intracerebroventricular administration of CGRP on Fos expression in the TNC. Neurosci Lett 559:99-104.
Bowen EJ, Schmidt TW, Firm CS, Russo AF, Durham PL (2006) Tumor necrosis factor-alpha stimulation of calcitonin gene-related peptide expression and secretion from rat trigeminal ganglion neurons. J Neurochem 96:65-77.
Brain SD, Grant AD (2004) Vascular actions of calcitonin gene-related peptide and adrenomedullin. Physiol Rev 84:903-934.
Burstein R, Yamamura H, Malick A, Strassman AM (1998) Chemical stimulation of the intracranial dura induces enhanced responses to facial stimulation in brain stem trigeminal neurons. J Neurophysiol 79:964-982.
Burstein R, Yarnitsky D, Goor‐Aryeh I, Ransil BJ, Bajwa ZH (2000) An association between migraine and cutaneous allodynia. Annals of neurology 47:614-624.
Burstein R, Jakubowski M, Garcia-Nicas E, Kainz V, Bajwa Z, Hargreaves R, Becerra L, Borsook D (2010) Thalamic sensitization transforms localized pain into widespread allodynia. Ann Neurol 68:81-91.
Dieterle A, Fischer MJ, Link AS, Neuhuber WL, Messlinger K (2011) Increase in CGRP- and nNOS-immunoreactive neurons in the rat trigeminal ganglion after infusion of an NO donor. Cephalalgia 31:31-42.
Dong Z, Jiang L, Wang X, Wang X, Yu S (2011) Nociceptive behaviors were induced by electrical stimulation of the dura mater surrounding the superior sagittal sinus in conscious adult rats and reduced by morphine and rizatriptan benzoate. Brain Res 1368:151-158.
Du JY, Fang JQ, Liang Y, Fang JF (2014) Electroacupuncture attenuates mechanical allodynia by suppressing the spinal JNK1/2 pathway in a rat model of inflammatory pain. Brain Res Bull 108:27-36.
Durham PL (2006) Calcitonin gene-related peptide (CGRP) and migraine. Headache 46 Suppl 1:S3-8.
Durham PL, Russo AF (2003) Stimulation of the calcitonin gene-related peptide enhancer by mitogen-activated protein kinases and repression by an antimigraine drug in trigeminal ganglia neurons. J Neurosci 23:807-815.
Edvinsson L (2015a) The Journey to establish cgrp as a migraine target: a retrospective view. Headache 55:1249-1255.
Edvinsson L (2015b) CGRP receptor antagonists and antibodies against CGRP and its receptor in migraine treatment. Br J Clin Pharmacol 80:193-199.
Eftekhari S, Edvinsson L (2011) Calcitonin gene-related peptide (CGRP) and its receptor components in human and rat spinal trigeminal nucleus and spinal cord at C1-level. BMC Neurosci 12:112.
Endres HG, Diener HC, Molsberger A (2007) Role of acupuncture in the treatment of migraine. Expert Rev Neurother 7:1121-1134.
Fang JQ, Du JY, Liang Y, Fang JF (2013) Intervention of electroacupuncture on spinal p38 MAPK/ATF-2/VR-1 pathway in treating inflammatory pain induced by CFA in rats. Mol Pain 9:13.
Fischer MJ (2010) Calcitonin gene-related peptide receptor antagonists for migraine. Expert Opin Investig Drugs 19:815-823.
Gao Z, Liu X, Yu S, Zhang Q, Chen Q, Wu Q, Liu J, Sun B, Fang L, Lin J, Zhu BM, Yan X, Liang F (2014) Electroacupuncture at acupoints reverses plasma glutamate, lipid, and LDL/VLDL in an acute migraine rat model: a (1) H NMR-based metabolomic study. Evid Based Complement Alternat Med 2014:659268.
Headache Classification Committee of the International Headache Society (IHS) (2013) The International Classification of Headache Disorders, 3rdedition (beta version). Cephalalgia 33:629-808.
Hoffmann J, Wecker S, Neeb L, Dirnagl U, Reuter U (2012) Primary trigeminal afferents are the main source for stimulus-induced CGRP release into jugular vein blood and CSF. Cephalalgia 32:659-667.
Jenkins DW, Langmead CJ, Parsons AA, Strijbos PJ (2004) Regulation of calcitonin gene-related peptide release from rat trigeminal nucleus caudalis slices in vitro. Neurosci Lett 366:241-244.
Lennerz JK, Ruhle V, Ceppa EP, Neuhuber WL, Bunnett NW, Grady EF, Messlinger K (2008) Calcitonin receptor-like receptor (CLR), receptor activity-modifying protein 1 (RAMP1), and calcitonin gene-related peptide (CGRP) immunoreactivity in the rat trigeminovascular system: differences between peripheral and central CGRP receptor distribution. J Comp Neurol 507:1277-1299.
Li QQ, Shi GX, Yang JW, Li ZX, Zhang ZH, He T, Wang J, Liu LY, Liu CZ (2015) Hippocampal cAMP/PKA/CREB is required for neuroprotective effect of acupuncture. Physiol Behav 139:482-490.
Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Vertosick EA, Vickers A, White AR (2016) Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev:CD001218.
Lipton RB, Bigal ME, Ashina S, Burstein R, Silberstein S, Reed ML, Serrano D, Stewart WF (2008) Cutaneous allodynia in the migraine population. Ann Neurol 63:148-158.
Liu L, Pei P, Zhao LP, Qu ZY, Zhu YP, Wang LP (2016) Electroacupuncture pretreatment at GB20 exerts antinociceptive effects via peripheral and central serotonin mechanism in conscious migraine rats. Evid Based Complement Alternat Med 2016:1846296.
Louter MA, Bosker JE, van Oosterhout WP, van Zwet EW, Zitman FG, Ferrari MD, Terwindt GM (2013) Cutaneous allodynia as a predictor of migraine chronification. Brain 136:3489-3496.
Lovati C, D’Amico D, Bertora P (2009) Allodynia in migraine: frequent random association or unavoidable consequence? Expert Rev Neurother 9:395-408.
Moore SA, Hettlich BF, Waln A (2013) The use of an electronic von Frey device for evaluation of sensory threshold in neurologically normal dogs and those with acute spinal cord injury. Vet J 197:216-219.
Noseda R, Burstein R (2013) Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain 154 Suppl 1:S44-53.
Park JY, Park JJ, Jeon S, Doo AR, Kim SN, Lee H, Chae Y, Maixner W, Lee H, Park HJ (2014) From peripheral to central: the role of ERK signaling pathway in acupuncture analgesia. J Pain 15:535-549.
Paxinos G, Watson C (1998) The Rat Brain Atlas in Stereotaxic Coordinates. San Diego: Academic.
Pei P, Liu L, Zhao L, Cui Y, Qu Z, Wang L (2016) Effect of electroacupuncture pretreatment at GB20 on behaviour and the descending pain modulatory system in a rat model of migraine. Acupunct Med 34:127-135.
Pietrobon D, Moskowitz MA (2013) Pathophysiology of migraine. Annu Rev Physiol 75:365-391.
Raddant AC, Russo AF (2011) Calcitonin gene-related peptide in migraine: intersection of peripheral inflammation and central modulation. Expert Rev Mol Med 13:e36.
Reddy DS (2013) The pathophysiological and pharmacological basis of current drug treatment of migraine headache. Expert Rev Clin Pharmacol 6:271-288.
Romero-Reyes M, Ye Y (2013) Pearls and pitfalls in experimental in vivo models of headache: conscious behavioral research. Cephalalgia 33:566-576.
Russo AF (2015) Calcitonin gene-related peptide (CGRP): a new target for migraine. Annu Rev Pharmacol Toxicol 55:533-552.
Siu FK, Lo SC, Leung MC (2005) Electro-acupuncture potentiates the disulphide-reducing activities of thioredoxin system by increasing thioredoxin expression in ischemia-reperfused rat brains. Life Sci 77:386-399.
Storer RJ, Akerman S, Goadsby PJ (2004) Calcitonin gene-related peptide (CGRP) modulates nociceptive trigeminovascular transmission in the cat. Br J Pharmacol 142:1171-1181.
Summ O, Charbit AR, Andreou AP, Goadsby PJ (2010) Modulation of nocioceptive transmission with calcitonin gene-related peptide receptor antagonists in the thalamus. Brain 133:2540-2548.
Uddman R, Edvinsson L, Ekman R, Kingman T, McCulloch J (1985) Innervation of the feline cerebral vasculature by nerve fibers containing calcitonin gene-related peptide: trigeminal origin and co-existence with substance P. Neurosci Lett 62:131-136.
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, AlMazroa MA, Alvarado M, Anderson HR, Anderson LM, Andrews KG, et al. (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2163-2196.
World Health Organization Regional Office for the Western Pacific (2008) WHO Standard Acupuncture Point Locations in the Western Pacific Region. Geneva: World Health Organization.
Wu GC (2009) Acupuncture analgesia in migraine. Chin J Integr Med 15:248-250.
Zhang Z, Winborn CS, Marquez de Prado B, Russo AF (2007) Sensitization of calcitonin gene-related peptide receptors by receptor activity-modifying protein-1 in the trigeminal ganglion. J Neurosci 27:2693-2703.
Zheng H, Chen M, Wu X, Li Y, Liang FR (2010) Manage migraine with acupuncture: a review of acupuncture protocols in randomized controlled trials. Am J Chin Med 38:639-650.
Copyedited by Patel B, Yajima W, Yu J, Li CH, Qiu Y, Song LP, Zhao M
*< class="emphasis_italic">Correspondence to: Lin-peng Wang, wlp5558@sina.com.
Lin-peng Wang, wlp5558@sina.com.
orcid: 0000-0002-0775-9939 (Lin-peng Wang)
10.4103/1673-5374.206652
Accepted: 2017-04-25
杂志排行
中国神经再生研究(英文版)的其它文章
- Cerebral mechanism of puncturing at He-Mu point combination for functional dyspepsia: study protocol for a randomized controlled parallel trial
- Efficacy of intraorbital electroacupuncture for diabetic abducens nerve palsy: study protocol for a prospective single-center randomized controlled trial
- Stem cell transplantation for spinal cord injury: a meta-analysis of treatment effectiveness and safety
- The brain activation pattern of the medial temporal lobe during chewing gum: a functional MRI study
- Correlation between photoreceptor injuryregeneration and behavior in a zebrafish model
- Correlation between white matter damage and gray matter lesions in multiple sclerosis patients