不同评分系统对急性非静脉曲张性上消化道出血患者危险分层的预测价值
2017-05-24寿松涛王力军
曹 鑫,寿松涛*,赵 珍,王力军
·论著·
·急诊急救·
不同评分系统对急性非静脉曲张性上消化道出血患者危险分层的预测价值
曹 鑫1,寿松涛1*,赵 珍2,王力军1
背景 成年人急性非静脉曲张性上消化道出血(ANVUGIB)是常见的临床急症,起病急、病情变化快,严重者可危及生命。如何迅速、准确地评估病情,快速分诊,制定合理的治疗方案是高效应用现有医疗资源,改善ANVUGIB患者预后的关键。目的 探讨Glasgow-Blatchford评分(GBS)、AIMS65、Rockall评分系统对ANVUGIB患者危险分层评估的准确性和预测价值。方法 选取2013—2015年天津医科大学总医院急诊科收治并确诊为ANVUGIB的246例患者,收集患者基本信息,并采用GBS、AIMS65、Rockall评分系统对患者进行危险分层。评估3种评分系统预测ANVUGIB患者干预、再出血、死亡的灵敏度、特异度、阳性预测值、阴性预测值及受试者工作特征(ROC)曲线下面积(AUC)。结果 246例患者中干预95例(38.6%),再出血15例(6.1%),死亡4例(1.6%)。GBS<2分时,0例需干预、再出血和死亡;AIMS65评分<2分时,19例需干预,1例再出血,1例死亡;Rockall评分<2分时,6例需干预,1例再出血,0例死亡。当GBS、AIMS65、Rockall评分≤2分时,预测ANVUGIB患者需干预的灵敏度和特异度分别为100.0%、80.0%、93.7%和26.5%、45.7%、15.9%,阳性预测值和阴性预测值分别为46.1%、48.1%、41.2%和100.0%、78.4%、80.0%,AUC分别为0.675〔95%CI(0.580,0.679)〕、0.643〔95%CI(0.545,0.741)〕、0.653〔95%CI(0.553,0.752)〕;预测再出血的灵敏度和特异度分别为100.0%、93.3%、93.3%和17.3%、37.7%、12.6%,阳性预测值和阴性预测值分别为7.3%、8.9%、6.5%和100.0%、98.9%、96.7%,AUC分别为0.809〔95%CI(0.638,0.941)〕、0.720〔95%CI(0.643,0.873)〕、0.800〔95%CI(0.597,0.907)〕;预测死亡的灵敏度和特异度分别为100.0%、100.0%、75.0%和16.5%、36.0%、12.4%,阳性预测值和阴性预测值分别为1.9%、1.9%、1.8%和100.0%、98.9%、100.0%,AUC分别为0.848〔95%CI(0.707,0.930)〕、0.804〔95%CI(0.723,0.976)〕、0.838〔95%CI(0.597,0.968)〕。结论 GBS更适合急诊,GBS≤2分时,可被视为低风险患者,低风险患者可以接受门诊治疗,缓解住院压力和减少医疗资源浪费。
胃肠出血;急性非静脉曲张性上消化道出血;GBS;AIMS65;Rockall;危险分层
曹鑫,寿松涛,赵珍,等.不同评分系统对急性非静脉曲张性上消化道出血患者危险分层的预测价值[J].中国全科医学,2017,20(14):1759-1764.[www.chinagp.net]
CAO X,SHOU S T,ZHAO Z,et al.Predictive value of different scoring systems for risk stratification in patients with acute non-variceal upper gastrointestinal bleeding[J].Chinese General Practice,2017,20(14):1759-1764.
急性上消化道出血是一种常见的潜在危及生命的临床急症,以发病率高、病情错综复杂、变化快为特点,需要快速评估和管理,选择高效、安全的评分系统对患者进行危险分层,将极大提高患者诊治效率。近几年已提出多个评估急性上消化道出血预后的评分系统,如Glasgow-Blatchford评分(GBS)、AIMS65、Rockall评分系统[1-8]。在不同国家,不同种族,乃至同一国家不同区域,不同评分系统对急性非静脉曲张性上消化道出血(ANVUGIB)患者预后评估价值不同[9-10]。本研究将围绕3种评分系统对急诊ANVUGIB患者干预、再出血和死亡风险评估能力进行阐述,以期更好地预测ANVUGIB患者的预后。
1 对象与方法
1.1 研究对象 采用回顾性分析方法,选取2013—2015年天津医科大学总医院急诊科收治并确诊为ANVUGIB的246例患者,排除大面积烧伤、创伤、急性心肌梗死等引起的应激性溃疡出血,疾病未得到完全控制出院和血液系统疾病引起的急性上消化道出血患者。
1.2 方法 收集患者一般资料,包括性别、年龄、入院前服用药物、伴随疾病、实验室检查、诊疗情况、住院天数、死亡和最后诊断。从上述资料中提取GBS、AIMS65和Rockall评分系统所需要的参数,结合患者一般资料进行评分。GBS:血红蛋白:男性120~129 g/L计1分、100~119 g/L计3分、<100 g/L计6分,女性100~119 g/L计1分、<100 g/L计6分;血尿素氮:6.5~7.9 mmol/L计2分、8.0~8.9 mmol/L计3分、9.0~24.9 mmol/L计4分、≥25.0 mmol/L计5分;收缩压:100~109 mm Hg(1 mm Hg=0.133 kPa)计1分、90~99 mm Hg计2分、<90 mm Hg计3分;心率≥100次/min计1分,黑便1分,晕厥2分,肝病2分,心力衰竭2分。以GBS评分0分、2分、6分、7分、8分、9分进行分组,0~2分为低危组,>2分为高危组。AIMS65评分:血浆清蛋白<30 g/L计1分,国际标准化比率(INR)>1.5计1分,格拉斯哥昏迷量表(GCS)评分<14分计1分,收缩压<90 mm Hg计1分,年龄>65岁计1分。以AIMS65评分0分、2分、3分、4分进行分组,0~2分为低危组,>2分为高危组。Rockall评分:年龄:<60岁计0分、60~79岁计1分、≥80岁计2分;休克状况:无休克计0分,心率≥100次/min计1分,收缩压≤100 mm Hg计2分;并发症:无计0分,心力衰竭、缺血性心脏病和其他重要并发症计2分,肝衰竭、肾衰竭和肿瘤播散计3分;内镜诊断:无病变、Mallory-Weiss综合征计0分,溃疡等其他病变计1分,上消化道恶性疾病计2分;内镜下出血征象:无计0分,上消化道血液潴留、黏附血凝块、血管暴露或喷血计2分。以Rockall评分0分、2分、6分、7分、8分、9分进行分组,0~2分为低危组,>2分为高危组。应用受试者工作特征(ROC)曲线分析GBS、AIMS65、Rockall评分系统对ANVUGIB患者危险分层评估的价值,绘制3种评分的ROC曲线,计算ROC曲线下面积(AUC);并计算3种评分系统的灵敏度、特异度、阳性预测值、阴性预测值。
1.3 定义 再出血的诊断指标:住院期间临床表现及生化指标转阴后再次出现呕血和黑便;红细胞计数、血红蛋白持续降低,而网织细胞持续升高;收缩压持续下降或心率增加;血尿素氮持续升高;内镜及手术探及上消化道出血;临床干预措施:输注血液成分;胃大部切除术;数字减影动脉、静脉栓塞术;内镜止血。

2 结果
2.1 一般临床特点 246例患者中男177例,女69例,男∶女为2.6∶1;年龄63(53,73)岁;伴随疾病:肝病42例(17.1%),恶性肿瘤34例(13.8%),心力衰竭12例(4.9%);入院前用药:阿司匹林29例(11.8%),氢氯吡格雷8例(3.2%),糖皮质激素3例(1.2%);内镜下所见:胃溃疡89例(36.2%),十二指肠溃疡66例(26.8%),贲门黏膜撕裂症29例(11.8%),胃癌27例(11.0%),糜烂性胃炎9例(3.7%),胃大部切除6例(2.4%),食管裂孔疝5例(2.0%),食管溃疡3例(1.2%),其他12例(4.9%);质子泵抑制剂218例(88.62%);干预:悬浮红细胞63例(25.6%),血浆19例(7.7%),血小板13例(5.3%),内镜止血3例(1.2%),数字减影1例(0.4%);再出血15例(6.1%);死亡4例(1.6%);住院天数(11.7±7.9)d。
2.2ANVUGIB患者在3种评分系统危险性积分中的临床情况分布 不同GBS、AIMS65、Rockall评分患者的临床资料分布见表1~3。
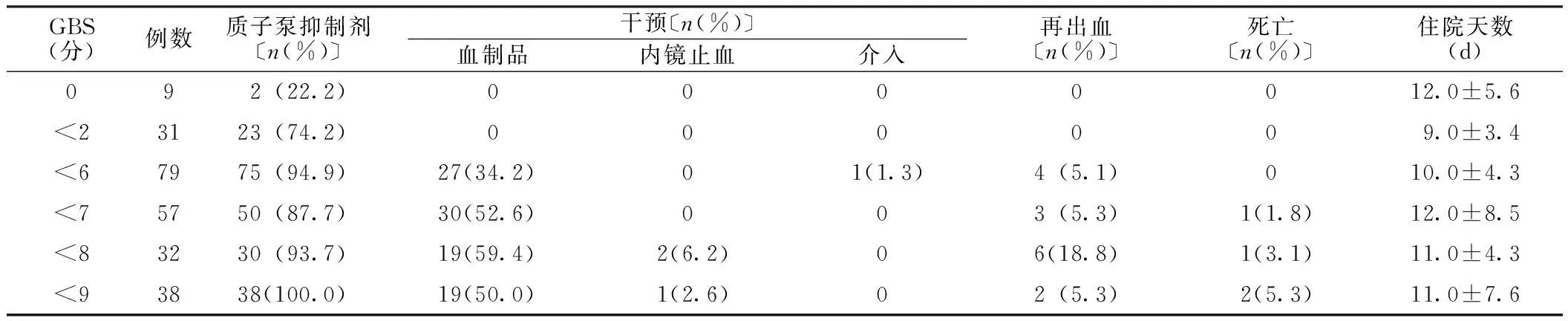
表1 不同GBS患者的临床情况分布
注:GBS=Glasgow-Blatchford评分
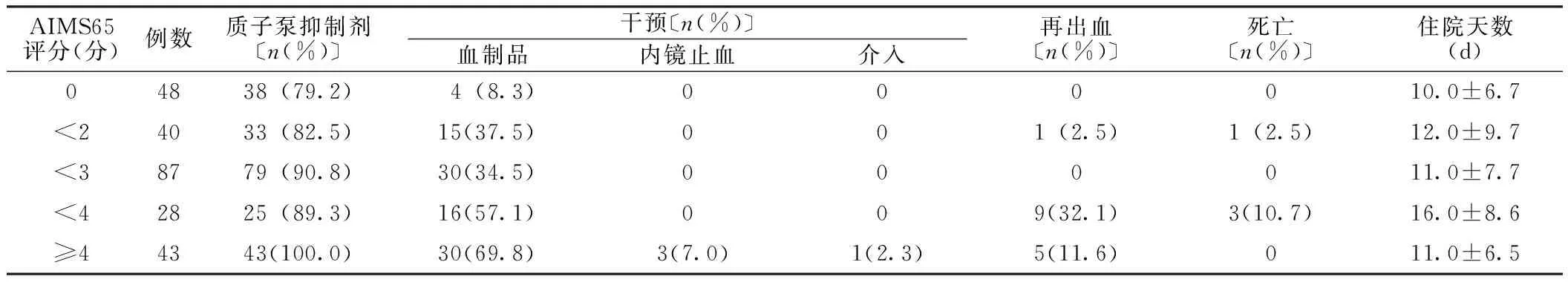
表2 不同AIMS65评分患者的临床情况分布
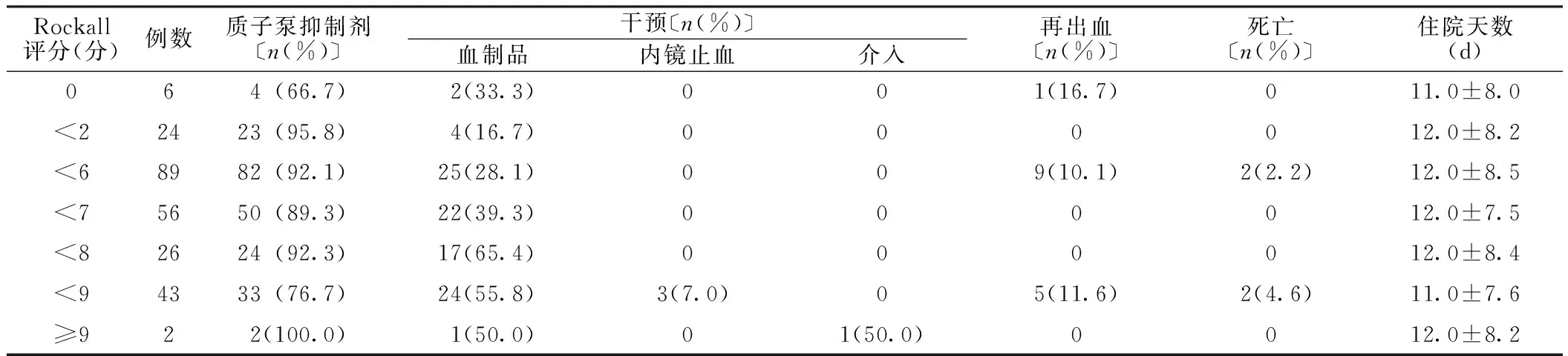
表3 不同Rockall评分患者的临床情况分布
2.3 3种评分系统对ANVUGIB患者危险分层评估比较 GBS≤2分时,预测ANVUGIB患者需干预的灵敏度为100.0%,特异度为26.5%,阳性预测值为46.1%,阴性预测值为100.0%,AUC为0.675〔95%CI(0.580,0.679)〕;预测ANVUGIB患者再出血的灵敏度为100.0%,特异度为17.3%,阳性预测值为7.3%,阴性预测值为100.0%,AUC为0.809〔95%CI(0.638,0.941)〕;预测ANVUGIB患者死亡的灵敏度为100.0%,特异度为16.5%,阳性预测值为1.9%,阴性预测值为100.0%,AUC为0.848〔95%CI(0.707,0.930)〕。AIMS65评分≤2分时,预测ANUVGIB患者需干预的灵敏度为80.0%,特异度为45.7%,阳性预测值为48.1%,阴性预测值为78.4%,AUC为0.643〔95%CI(0.545,0.741)〕;预测ANVUGIB患者再出血的灵敏度为93.3%,特异度为37.7%,阳性预测值为8.9%,阴性预测值为98.9%,AUC为0.720〔95%CI(0.643,0.873)〕;预测ANVUGIB患者死亡的灵敏度为75.0%,特异度为36.0%,阳性预测值为1.9%,阴性预测值为98.9%,AUC为0.804〔95%CI(0.723,0.976)〕。Rockall评分≤2分时,预测ANVUGIB患者需干预的灵敏度为93.7%,特异度为15.9%,阳性预测值为41.2%,阴性预测值为80.0%,AUC为0.653〔95%CI(0.553,0.752)〕;预测ANVUGIB患者再出血的灵敏度为93.3%,特异度为12.6%,阳性预测值为6.5%,阴性预测值为96.7%,AUC为0.800〔95%CI(0.597,0.907)〕;预测ANVUGIB患者死亡的灵敏度为100.0%,特异度为12.4%,阳性预测值为1.8%,阴性预测值为100.0%,AUC为0.838〔95%CI(0.597,0.968)〕(见图1~3)。
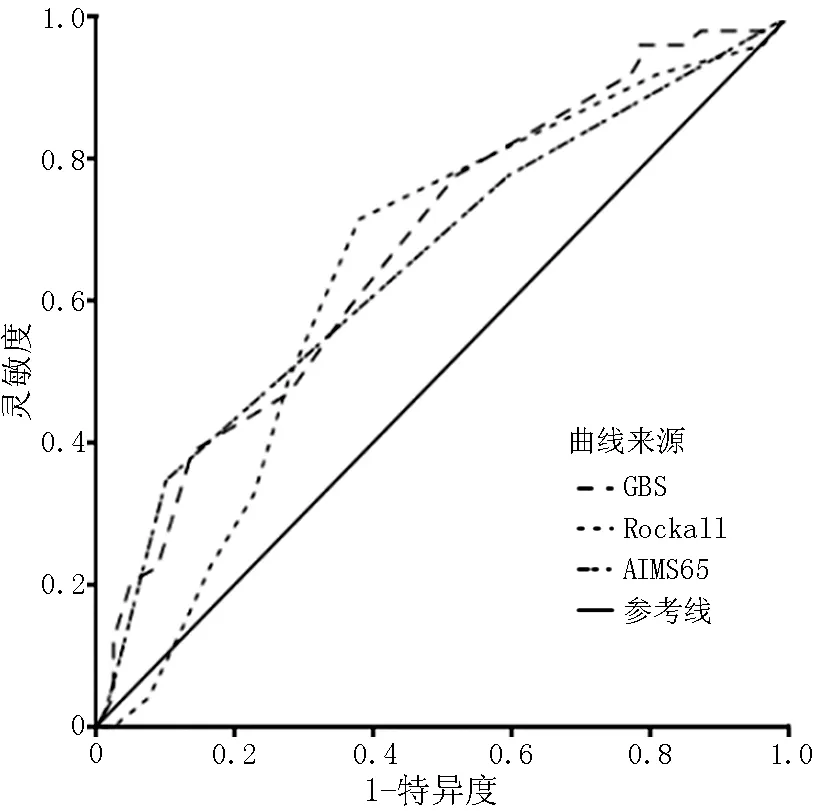
注:GBS=Glasgow-Blatchford评分
图1 3种评分系统预测ANVUGIB患者需干预的ROC曲线
Figure 1 ROC curve of 3 scoring systems for predicting the probability of needing reinterventions in the ANVUGIB patients
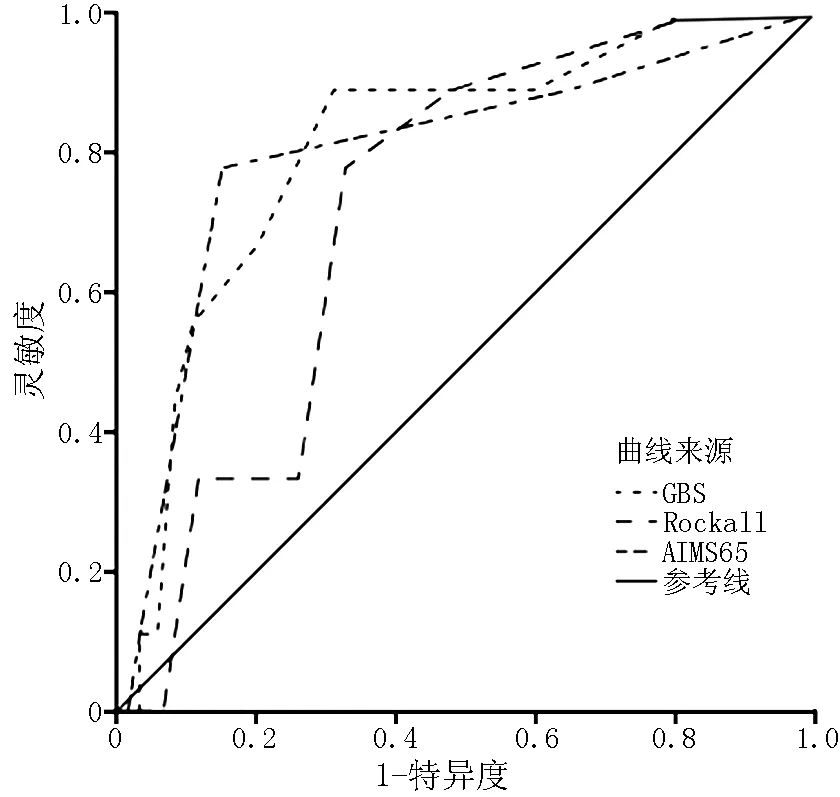
图2 3种评分系统预测ANVUGIB患者再出血的ROC曲线
Figure 2 ROC curve of 3 scoring systems for predicting the probability of rebleeding in the ANVUGIB patients
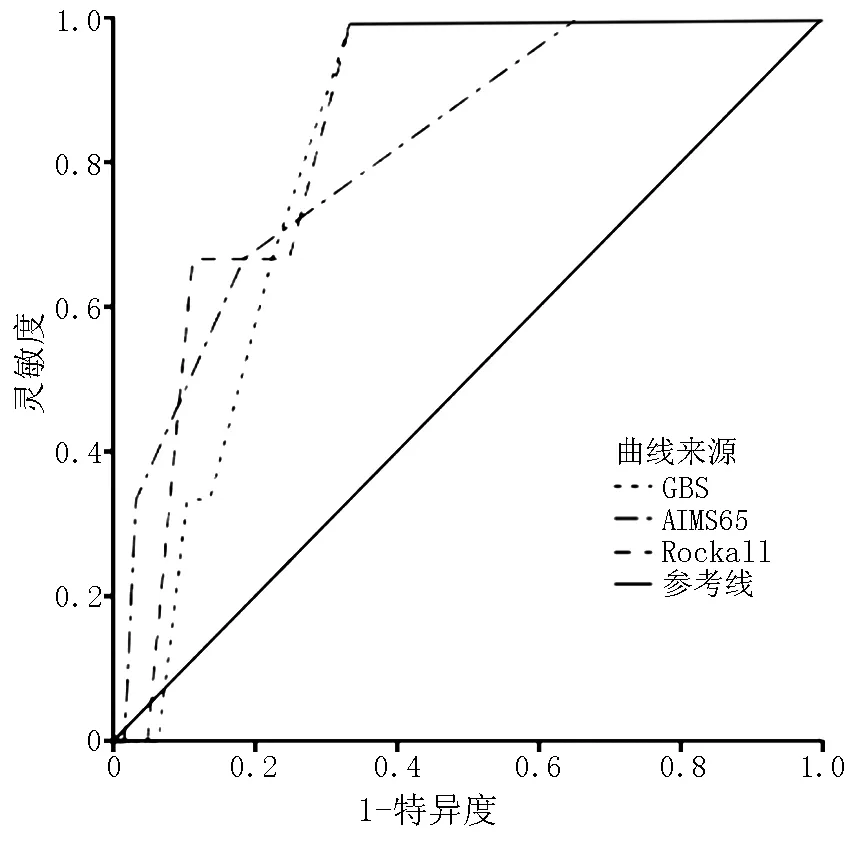
图3 3种评分系统预测ANVUGIB患者死亡的ROC曲线
Figure 3 ROC curve of 3 scoring systems for predicting the probability of death in the ANVUGIB patients
3 讨论
本研究结果显示,ANVUGIB患者男女性别之比为2.6∶1,50%以上患者年龄>60岁,消化性溃疡出血占主要原因,其中以胃溃疡多见,老年患者多伴有心脑血管等基础疾病和多有口服阿司匹林等病史,该病因结构可能与我国老年男性多有吸烟、饮酒史,可增加血管动脉粥样硬化的风险和老年患者长期服用心脑血管药物,可影响胃黏膜保护机制有关,与国内文献报道一致[11]。
本组资料显示,患者再出血率(6.1%)较国外文献(10%~30%)低[12],患者病死率(1.6%)较国外文献(6%~8%)低[13],可能与本次病例采集均为剔除了病死率、再出血率较高的食管胃底静脉曲张出血的上消化道出血患者和未进行出院后30 d随访有关。
本研究结果显示,GBS<2分时,0例患者需干预、再出血和死亡;AIMS65评分<2分时,19例患者输血,1例再出血和1例死亡;Rockall评分<2分时,6例患者输血,1例再出血。当GBS、AIMS65、Rockall评分≤2分时,预测ANVUGIB患者需干预的灵敏度和特异度分别为100.0%、80.0%、93.7%和26.5%、45.7%、15.9%,再出血的灵敏度和特异度为100.0%、93.3%、93.3%和17.3%、37.7%、12.6%,死亡的灵敏度和特异度为100.0%、100.0%、75.0%和16.5%、36.0%、12.4%。GBS预测危险分层灵敏度较高,与邵颖等[14]研究结果一致,而特异度较低,这可能与GBS指标涵盖面广有关。当GBS、AIMS65、Rockall评分≤2分时,预测ANVUGIB患者需干预的阳性预测值和阴性预测值为46.1%、48.1%、41.2%和100.0%、78.4%、80.0%,再出血的阳性预测值和阴性预测值为7.3%、8.9%、6.5%和100.0%、98.9%、96.7%;死亡的阳性预测值和阴性预测值为1.9%、1.9%、1.8%和100.0%、98.9%、100.0%。3种评分系统阳性预测值低而阴性预测值较高,可能与ANVUGIB患者干预率、再出血率、病死率低及低危患者例数较少有关。GBS、AIMS65、Rockall评分预测需干预的AUC为0.675、0.653、0.643,GBS对ANVUGIB患者需干预评估AUC最大,与赖晓波等[15]研究结果一致。GBS是2000年在苏格兰地区前瞻性收集1 748例包含静脉曲张出血的ANVUGIB患者,进行多因素分析后制订的,目前证实该评分系统对ANVUGIB患者干预、再出血、死亡评估具有预测价值,并被2015年急性上消化道出血急诊诊治流程专家共识所推荐[16-24];荷兰的一项研究提示,GBS预测ANVUGIB患者需干预能力较消化科专业医师经验评估需干预能力准确性高[25];此外,GBS不包括胃镜检查结果、年龄范畴及计算GCS评分,仅包含临床和实验室因素(收缩压、心率、黑便、晕厥、肝病、心力衰竭、血尿素氮),简单、易获和经济,因此GBS更适合急诊,GBS≤2分时,ANVUGIB患者被定义为低风险,与AQUARIUS等[16]研究结果一致。本研究亦存在不足之处,观察例数相对较少,有可能导致结果偏倚;本研究没有进行出院后随访,不排除部分患者出院后有疾病复发甚至加重风险,可能导致再出血率、病死率降低,因此需要大样本研究,并进行随访,制定满足急诊科需求的评分系统。
作者贡献:曹鑫、寿松涛进行文章的构思与设计、研究的实施与可行性分析、对文章整体负责;曹鑫进行数据收集、结果的分析与解释、撰写论文;曹鑫、赵珍进行数据整理、统计学处理;寿松涛、王力军进行论文修订;寿松涛负责文章的质量控制及审校。
本文无利益冲突。
[1]DE GROOT N,VAN OIJEN M,KESSELS K,et al.Prediction scores or gastroenterologists′ Gut Feeling for triaging patients that present with acute upper gastrointestinal bleeding[J].United European Gastroenterol J,2014,2(3):197-205.DOI:10.1177/2050640614531574.
[2]WANG C Y,QIN J,WANG J,et al.Rockall score in predicting outcomes of elderly patients with acute upper gastrointestinal bleeding[J].World J Gastroenterol,2013,19(22):3466-3472.DOI:10.3748/wjg.v19.i22.3466.
[3]STANLEY A J,ASHLEY D,DALTON H R,et al.Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage:multicentre validation and prospective evaluation[J].Lancet,2009,373(9657):42-47.DOI:10.1016/s0140-6736(08)61769-9.
[4]THANDASSERY R B,SHARMA M,JOHN A K,et al.Clinical application of AIMS65 scores to predict outcomes in patients with upper gastrointestinal hemorrhage[J].Clin Endosc,2015,48(5):380-384.DOI:10.5946/ce.2015.48.5.380.
[5]DICU D,POP F,IONESCU D,et al.Comparison of risk scoring systems in predicting clinical outcome at upper gastrointestinal bleeding patients in an emergency unit[J].Am J Emerg Med,2013,31(1):94-99.DOI:10.1016/j.ajem.2012.06.009.
[6]WANG C H,CHEN Y W,YOUNG Y R,et al.A prospective comparison of 3 scoring systems in upper gastrointestinal bleeding[J].Am J Emerg Med,2013,31(5):775-778.DOI:10.1016/j.ajem.2013.01.007.
[7]许勤,胡乃中,刘衡,等.急性非静脉曲张上消化道出血风险评估的临床研究[J].中华消化杂志,2010,30(11):828-831.DOI:10.3760/cma.j.issn.0254-1432.2010.11.011. XU Q,HU N Z,LIU H,et al.Clinical research of risk assessment of acute nonvariceal upper gastrointestinal bleeding[J].Chinese Journal of Digestion,2010,30(11):828-831.DOI:10.3760/cma.j.issn.0254-1432.2010.11.011.
[8]陈剑,唐帅,唐小华.AIMS65评分系统在急性上消化道出血患者中的应用研究[J].中国医学创新,2016,13(1):47-49.DOI:10.3969/j.issn.1674-4985.2016.01.013. CHEN J,TANG S,TANG X H.The applications of AIMS65 score in acute upper gastrointestinal bleeding[J].Medical Innovation of China,2016,13(1):47-49.DOI:10.3969/j.issn.1674-4985.2016.01.013.
[9]PANG S H,CHING J Y,LAU J Y,et al.Comparing the Blatchford and pre-endoscopic Rockall score in predicting the need for endoscopic therapy in patients with upper GI hemorrhage[J].Gastrointest Endosc,2010,71(7):1134-1140.DOI:10.1016/j.gie.2010.01.028.
[10]NAKAMURA S,MATSUMOTO T,SUGIMORI H,et al.Emergency endoscopy for acute gastrointestinal bleeding:prognostic value of endoscopic hemostasis and the AIMS65 score in Japanese patients[J].Dig Endosc,2014,26(3):369-376.DOI:10.1111/den.12187.
[11]陈建梅,柴艳芬.不同群组上消化道出血相关危险因素及危险度评估[J].当代医学,2015,21(10):19-21.DOI:10.3969/j.issn.1009-4393.2015.10.012. CHEN J M,CHAI Y F.Risk assessment of upper gastrointestinal bleeding in different groups and risk factors[J].Contemporary Medicine,2015,21(10):19-21.DOI:10.3969/j.issn.1009-4393.2015.10.012.
[12]BARKUN A,SABBAH S,ENNS R,et al.The Canadian Registry on Nonvariceal Upper Gastrointestinal Bleeding and Endoscopy(RUGBE):endoscopic hemostasis and proton pump inhibition are associated with improved outcomes in a real-life setting[J].Am J Gastroenterol,2004,99(7):1238-1246.DOI:10.1111/j.1572-0241.2004.30272.x.
[13]BARKUN A,BARDOU M,MARSHALL J K,et al.Consensus recommendations for managing patients with nonvariceal upper gastrointestinal bleeding[J].Ann Intern Med,2003,139(10):843-857.DOI:10.7326/0003-4819-139-10-200311180-00012.
[14]邵颖,魏晟,谭漫红,等.Blatchford危险评分系统对老年人急性非静脉曲张上消化道出血的评估价值[J].中华老年医学杂志,2015,34(1):62-66.DOI:10.3760/cma.j.issn.0254-9026.2015.01.016. SHAO Y,WEI S,TAN M H,et al.Prognostic value of Blatchford score system in acute non-variceal upper gastrointestinal bleeding in elderly patients[J].Chinese Journal of Geriatrics,2015,34(1):62-66.DOI:10.3760/cma.j.issn.0254-9026.2015.01.016.
[15]赖晓波,聂玉强,李瑜元,等.四种非静脉曲张上消化道出血危险性评分系统的对比分析[J].现代消化及介入诊疗,2010,15(5):277-280.DOI:10.3969/j.issn.1672-2159.2010.05.003. LAI X B,NIE Y Q,LI Y Y,et al.Comparison of four different risk score systems in non-variceal upper gastrointestinal bleeding[J].Modern Digestion & Intervention,2010,15(5):277-280.DOI:10.3969/j.issn.1672-2159.2010.05.003.
[16]AQUARIUS M,SMEETS F G,KONIJN H W,et al.Prospective multicenter validation of the Glasgow Blatchford bleeding score in the management of patients with upper gastrointestinal hemorrhage presenting at an emergency department[J].Eur J Gastroenterol Hepatol,2015,27(9):1011-1016.DOI:10.1097/meg.0000000000000402.
[17]NAKAMURA S,MATSUMOTO T,SUGIMORI H,et al.Emergency endoscopy for acute gastrointestinal bleeding:prognostic value of endoscopic hemostasis and the AIMS65 score in Japanese patients[J].Dig Endosc,2014,26(3):369-376.DOI:10.1111/den.12187.
[18]BLATCHFORD O,MURRAY W R,BLATCHFORD M.A risk score to predict need for treatment for upper-gastrointestinal haemorrhage[J].Lancet,2000,356(9238):1318-1321.DOI:10.1016/s0140-6736(00)02816-6.
[19]QUACH D T,DAO N H,DINH M C,et al.The performance of a modified Glasgow blatchford score in predicting clinical interventions in patients with acute nonvariceal upper gastrointestinal bleeding:a vietnamese prospective multicenter cohort study[J].Gut Liver,2016,10(3):375-381.DOI:10.5009/gnl15254.
[20]SCHIEFER M,AQUARIUS M,LEFFERS P,et al.Predictive validity of the Glasgow Blatchford Bleeding Score in an unselected emergency department population in continental Europe[J].Eur J Gastroenterol Hepatol,2012,24(4):382-387.DOI:10.1097/MEG.0b013e3283505965.
[21]钱洁,陈怡,仲敏,等.Rockall与Blatchford评分系统评估急性上消化道出血的比较研究[J].胃肠病学,2011,16(11):644-648.DOI:10.3969/j.issn.1008-7125.2011.11.002. QIAN J,CHEN Y,ZHONG M,et al.Comparative study of Rockall and Blatchford risk scoring systems in assessment of acute upper gastrointestinal bleeding[J].Chinese Journal of Gastroenterol,2011,16(11):644-648.DOI:10.3969/j.issn.1008-7125.2011.11.002.
[22]SALTZMAN J R,TABAK Y P,HYETT B H,et al.A simple risk score accurately predicts in-hospital mortality,length of stay,and cost in acute upper GI bleeding[J].Gastrointest Endosc,2011,74(6):1215-1224.DOI:10.1016/j.gie.2011.06.024.
[23]ROCKALL T A,LOGAN R F,DEVLIN H B,et al.Risk assessment after acute upper gastrointestinal haemorrhage[J].Gut,1996,38(3):316-321.DOI:10.1136/gut.38.3.316.
[24]中国医师协会急诊医师分会.急性上消化道出血急诊诊治流程专家共识[J].中国急救医学,2015,35(10):961-970.DOI:10.3969/j.issn.1002-1949.2015.10.000. Chinese Medical Association Emergency Physician Branch.Expert consultation on emergency diagnosis and treatment of acute upper gastrointestinal bleeding[J].Chinese Journal of Critical Care Medicine,2015,35(10):961-970.DOI:10.3969/j.issn.1002-1949.2015.10.000.
[25]BRYANT R V,KUO P,WILLIAMSON K,et al.Performance of the Glasgow-Blatchford score in predicting clinical outcomes and intervention in hospitalized patients with upper GI bleeding[J].Gastrointest Endosc,2013,78(4):576-583.DOI:10.1016/j.gie.2013.05.003.
(本文编辑:贾萌萌)
Predictive Value of Different Scoring Systems for Risk Stratification in Patients with Acute Non-variceal Upper Gastrointestinal Bleeding
CAOXin1,SHOUSong-tao1*,ZHAOZhen2,WANGLi-jun1
1.TianjinMedicalUniversityGeneralHospital,Tianjin300070,China2.BeijingCharityHospital,ChinaRehabilitationResearchCenter,Beijing100068,China
*Correspondingauthor:SHOUSong-tao,Chiefphysician;E-mail:stshou66@sina.com
Background Acute non-variceal upper gastrointestinal bleeding (ANVUGIB) in adults is a common clinical emergency characterized by acute onset,fast-changing conditions,and threatening life when it is serious.How to quickly and accurately assess the condition,rapid diagnosis,and develop a reasonable treatment regimen is the key to improving the prognosis of ANVUGIB patients by effectively utilizing existing medical resources.Objective To compare the accuracy of Glasgow-Blatchford bleeding score(GBS),AIMS65 and Rockall scoring systems for the risk prediction of outcome in ANVUGIB patients.Methods We conducted the risk stratification of 246 patients with ANVUGIB admitted in Department of Emergency,Tianjin Medical University General Hospital from 2013 to 2015 by using GBS,AIMS65,Rockall scoring systems,respectively based on analyzing the baseline characteristics of the patients.We compared the sensitivity,specificity,positive predictive value,negative predictive value and area under the curve(AUC) of the receiver operating characteristic (ROC) of these 3 scoring systems in the prediction of the probability of needing interventions,rebleeding and death.Results Of the 246 patients,95(38.6%) received interventions,15(6.1%) had rebleeding,and 4(1.6%) died.When the patients had GBS <2 points,no one needed interventions,had rebleeding and died;when the patients had AIMS65 score <2 points,19 patients needed interventions,1 had rebleeding and 2 died;but when the patients had Rockall score <2 points,6 needed interventions,1 had rebreeding and no one died.When the GBS,AIMS65 score and Rockall score of the patients were all ≤2 points,in terms of predicting the probability of needing interventions in the ANVUGIB patients,the sensitivity of GBS,AIMS65 and Rockall scoring systems were 100.0%,80.0%,93.7%,respectively,the specificity of them were 26.5%,45.7%,15.9%,respectively,positive predictive value of them were 46.1%,48.1%,and 41.2%,respectively,negative predictive value of them were 100.0%,78.4%,80.0%,respectively,AUC of them were 0.675〔95%CI(0.580,0.679)〕,0.643〔95%CI(0.545,0.741)〕,0.653〔95%CI(0.553,0.752)〕,respectively;in regard to predicting the probability of rebleeding in the ANVUGIB patients,the sensitivity of GBS,AIMS65 and Rockall scoring systems were 100.0%,93.3%,93.3%,respectively,the specificity of them were 17.3%,37.7%,12.6%,respectively,positive predictive value of them were 7.3%,8.9%,6.5%,respectively,negative predictive value of them were 100.0%,98.9% and 96.7%,respectively,AUC of them were 0.809〔95%CI(0.638,0.941)〕,0.720〔95%CI(0.643,0.873)〕,0.800〔95%CI(0.597,0.907)〕,respectively;in the aspect of predicting the probability of death in the ANVUGIB patients,the sensitivity of GBS,AIMS65 and Rockall scoring systems were 100.0%,100.0%,and 75.0%,respectively,the specificity of them were 16.5%,36.0%,12.4%,respectively,positive predictive value of them were 1.9%,1.9%,and 1.8%,respectively,negative predictive value of them were 100.0%,98.9% and 100.0%,respectively,AUC of them were 0.848〔95%CI(0.707,0.930)〕,0.804〔95%CI(0.723,0.976)〕,0.838〔95%CI(0.597,0.968)〕,respectively.Conclusion GBS is more suitable for emergency predicting the risk of outcome in patients with ANVUGIB.Patients with GBS ≤2 points can be considered as low-risk patients.They can receive outpatient treatment,by which bed shortages can be relieved and medical resources can be saved to some extent.
Gastrointestinal hemorrhage;ANVUGIB;GBS;AIMS65;Rockall;Risk stratification
R 573.2
A
10.3969/j.issn.1007-9572.2017.14.021
2016-12-16;
2017-03-09)
1.300070天津市,天津医科大学总医院
2.100068北京市,中国康复研究中心北京博爱医院
*通信作者:寿松涛,主任医师;E-mail:stshou66@sina.com
