系统性红斑狼疮合并弥漫性肺泡出血一例并文献复习
2017-05-12张利窦艳娜马爽肖静程根阳刘栋赵占正
张利 窦艳娜 马爽 肖静 程根阳 刘栋 赵占正
·论著·
系统性红斑狼疮合并弥漫性肺泡出血一例并文献复习
张利 窦艳娜 马爽 肖静 程根阳 刘栋 赵占正
目的 分析系统性红斑狼疮(systemic lupus erythematosus,SLE)合并弥漫性肺泡出血(diffuse alveolar hemorrhage,DAH)的临床特点,观察血浆置换联合激素救治该类患者的临床疗效,以提高对罕见病例的诊疗水平,避免误诊及延误治疗。方法 回顾性分析2015年8月12日郑州大学第一附属医院收治的1例SLE合并DAH患者的临床表现,观察血浆置换联合激素冲击治疗该患者的临床疗效,同时综合分析国内报道的101例SLE合并DAH患者的临床表现、治疗方案及其临床效果。结果 本例20岁女性患者,临床表现主要为发热,痰中带血,面颊部红斑,伴阴道出血;实验室检查结果提示抗核抗体(antinuclear antibodies ,ANA)1∶1000,抗双链DNA(anti double stranded DNA,ds-DNA)抗体阳性,抗Smith抗体阳性;贫血,血红蛋白进行性下降;胸部CT示两肺野见多发条片状,斑点状,结节状密度增高影,边缘模糊。诊断考虑SLE合并DAH,给予血浆置换联合激素冲击,同时给予人免疫丙种球蛋白应用,患者咯血停止,面颊部红斑消失,贫血较前明显改善,目前口服糖皮质激素并规律减量。我国文献报道类似病例101例,具体描述患者临床表现的有83例,这些患者中ANA均为阳性,抗ds-DNA抗体阳性者58例,咯血67例,发热61例,肾脏受累71例,血红蛋白下降74例,呼吸困难80例,低氧血症70例。影像学均显示肺部浸润影。通过血浆置换、激素冲击,免疫抑制剂等药物的应用,10例行血浆置换,7例有效;29例给予丙种球蛋白,21例有效;74例接受了大剂量激素冲击,47例有效;21例使用了机械通气,8例有效;49例给予免疫抑制剂,36例有效;12例使用了支气管肺泡灌洗,10例有效。结论 DAH是SLE罕见且威胁生命的并发症,尽早明确诊断,及时血浆置换联合激素冲击等对症支持治疗,积极防治并发症,可有效改善患者的临床表现及其预后。
系统性红斑狼疮; 弥漫性肺泡出血; 文献复习
弥漫性肺泡出血(diffuse alveolar hemorrhage,DAH)是系统性红斑狼疮(systemic lupus erythematosus,SLE)罕见而又威胁生命的并发症,此病病情进展迅速,病死率高,但其临床表现并不具有特异性,容易被误诊或漏诊。我们收治了1例SLE合并DAH的患者,本文通过分析此病的临床表现及诊疗经过,并复习了相关文献,讨论了此类疾病的临床表现及治疗措施,以提高对此类疾病的认识,及早有效地抢救患者的生命及改善预后。
病 例 资 料
患者,女,20岁,因“间断发热1个月,不规则阴道出血4 d”于2015年8月12日入院。患者1个月前无明显诱因出现发热,体温最高达40 ℃,无明显咳嗽、咳痰,无口腔溃疡、脱发、面部皮疹等症状,于当地诊所给予退热药物应用,体温降至正常。4 d前无明显诱因出现轻度头痛,咳嗽,咳痰,痰中带血, 为鲜红色, 伴阴道出血,出血量大于月经量,色鲜红,伴血块及乏力。体检:体温39℃,血压78/38~102/67 mmHg,心率84次/min,双侧面部及鼻梁处可见散在红斑,心脏各瓣膜听诊区未闻及明显杂音,双肺听诊可闻及散在湿啰音,双肾区叩击痛阴性,阴道持续出血,色鲜红,如月经量。血常规:白细胞计数(white blood cell,WBC)7.3×109/L,红细胞计数(red blood cell,RBC) 3.97×1012/L,血红蛋白113 g/L,血小板计数33×109/L。1 d后RBC 2.69×1012/L,血红蛋白76 g/L(阴道出血量明显减少),11 h后血红蛋白降至54 g/L。尿常规:尿蛋白阴性,尿红细胞0.66/μl,尿白细胞8.58/μl,24 h尿蛋白定量为0.03 g,丙氨酸氨基转移酶175 U/L,天门冬氨酸氨基转移酶>1 333 U/L,血白蛋白22.7 g/L,血尿素氮10.16 mmol/L,血肌酐51 μmol/L,活化部分凝血活酶时间(activated partial thromboplastin time,APTT)78.1 s,凝血酶原时间(prothrombin time,PT) 11.6 s (5 d后APTT 34.8 s, PT 9.10 s),CD4为120,CD4/CD8为0.81,补体C3为0.25 g/L,补体C4为0.02 g/L,Ⅶ因子活性202.8%(50%~129%), 红细胞沉降率9.9 mm/h,C反应蛋白95.12 mg/L,降钙素原1.528 μg/L。抗核抗体(antinuclear antibodies,ANA)1∶1000, 抗双链DNA(anti double stranded DNA,ds-DNA)抗体, 抗Smith抗体阳性, ENA谱中其余抗体阴性。抗中性粒细胞胞质抗体、髓过氧化物酶、抗肾小球基底膜抗体、抗心磷脂抗体均阴性。影像学检查:腹部彩超示肝轻度弥漫性回声改变。心电图:窦性心动过速,ST-T改变。子宫彩超:宫颈处不均质稍高回声(考虑积血)。胸部CT示:两肺野见多发条片状,斑点状,结节状密度增高影,边缘模糊(见图1A)。系统性红斑狼疮疾病活动度评分(systemic lupus erythematosus disease activity index,SLEDAI)为20分。诊断为:①系统性红斑狼疮合并弥漫性肺泡出血;②功能失调性子宫出血;③失血性低血压。给予3次血浆置换,血浆置换量为2 600 ml每次(根据体质量45 kg和红细胞比容0.17计算),同时给予隔天应用甲泼尼龙0.5 g,3次,期间给予甲泼尼龙40 mg,每天2次,静脉滴注;人免疫球蛋白针20 g,连用3 d;同时给予输注红细胞、缩宫素、比阿培南(后根据血培养结果改为莫西沙星)。患者咯血量较前减少,血红蛋白趋于正常。入院2 d后患者阴道出血量减少并逐渐停止,但仍有间断痰中带血症状,遂于入院后第13天再次给予甲泼尼龙0.5 g,隔天应用,连用3次;人免疫球蛋白针12.5 g,连用3 d。同时行气管镜检查,未见出血点,气管活检提示真菌感染。
出院后患者规律服用泼尼松60 mg/d(3个月后减为50 mg/d,之后每1周减10 mg。现为60 mg,隔天1次),以及伏立康唑片0.2 g,口服,每天2次,共服1周。复查结果如表1及图1B、图1C、图1D。
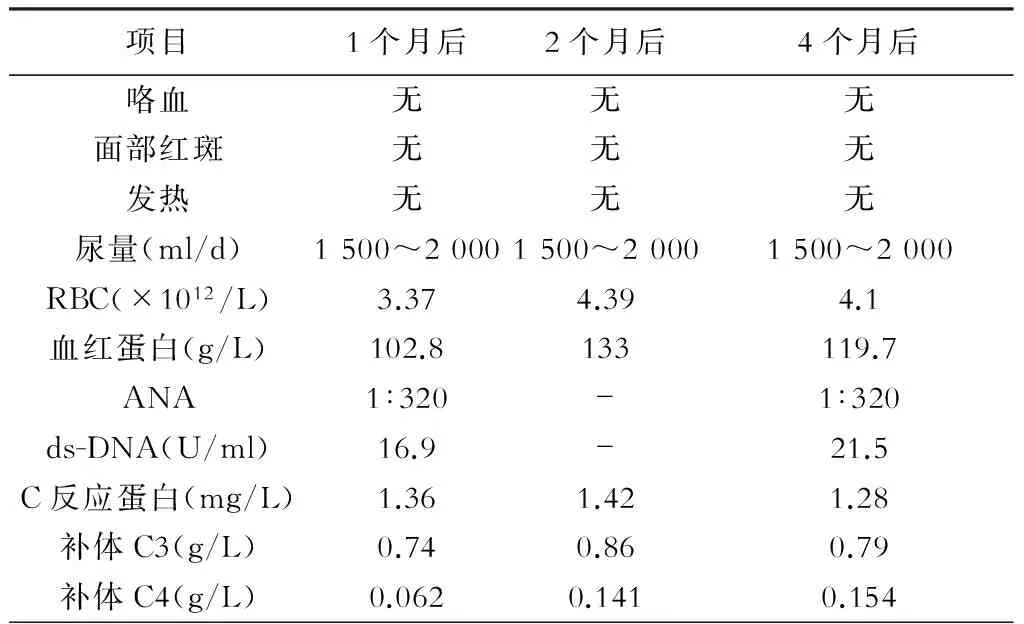
表1 患者随访结果
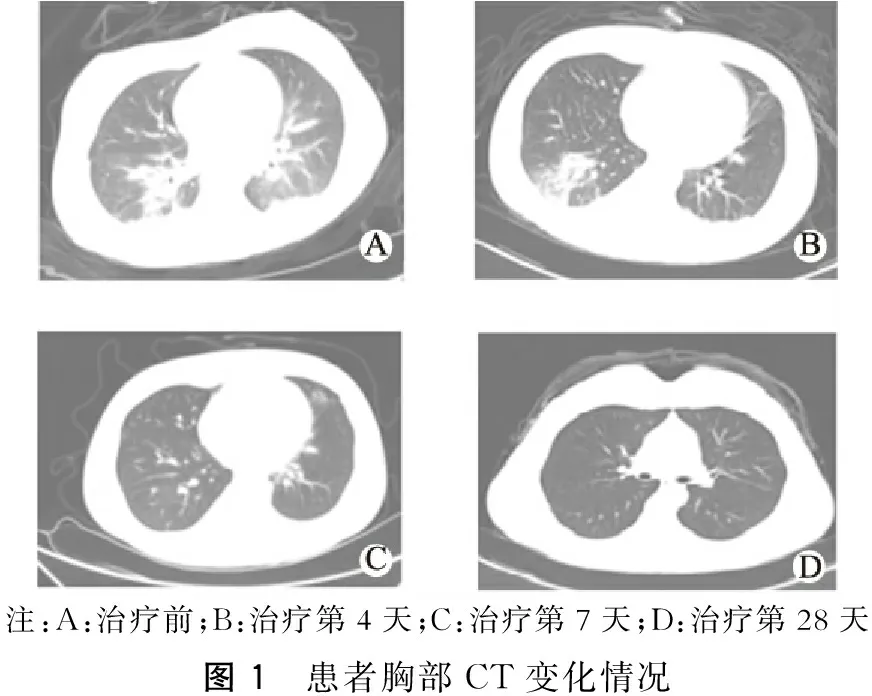
注:A:治疗前;B:治疗第4天;C:治疗第7天;D:治疗第28天图1 患者胸部CT变化情况
讨 论
DAH是SLE患者罕见却威胁生命的并发症,最早于1904年由Osler[1]报道。在SLE患者中的发病率为0.52%~5.7%[2-5],其发病机制目前尚不明确,可能与免疫复合物导致肺泡毛细血管基底膜损伤和血管炎有关,还可能与继发感染﹑充血性心力衰竭﹑神经源性肺水肿﹑肾衰竭和颅内高压有关[6]。
SLE患者符合以下4条标准中的至少3条即可诊断为SLE合并DAH:①肺部症状:咯血,呼吸困难,低氧血症;②肺部影像学:新出现的肺部浸润影;③原因不明情况下的血红蛋白快速下降,24~48 h内下降>15 g/L,且与咯血量不匹配;④支气管镜或支气管肺泡灌洗液显示出血或有含铁血黄素巨噬细胞。本例患者临床表现有发热,面颊部红斑,实验室检查示ANA 1∶1000,ds-DNA 抗体阳性,贫血等,符合SLE诊断,另患者痰中持续带血,低氧血症,胸部CT示两肺野多发条状、斑片状﹑结节状密度增高影。患者血红蛋白在12 h内下降23 g/L。临床排除了心力衰竭,肺栓塞及出凝血障碍,符合SLE合并DAH的诊断。
回顾性分析1996年至2012年我国文献报道的101例SLE合并DAH,其中38例行支气管镜或支气管肺泡灌洗,提示肺泡出血或含铁血黄素巨噬细胞。研究表明SLEDAI大于10分可作为SLE合并DAH的独立危险因素[5],本例患者SLEDAI评分为20分。
根据既往的文献报道,SLE合并DAH的发病年龄为11~62岁,平均年龄(29±14)岁,以青年女性多见,男女发病比例为4∶13[7]。回顾性分析上述101例SLE并DAH患者,其中男性23例,女性78例,男女比例约为3∶10,其中年龄最小者为12岁男孩。本例患者为女性,发病年龄21岁,较平均年龄明显提前。
SLE合并DAH的临床表现多种多样,其中文献中具体描述患者临床表现的有83例,这些患者中ANA均为阳性,抗ds-DNA抗体阳性者58例,咯血67例,发热61例,肾脏受累71例,血红蛋白下降74例,呼吸困难80例,低氧血症70例。影像学均显示肺部浸润影。本例患者有咯血,发热,ANA阳性,抗ds-DNA抗体阳性,并有头痛,低氧血症,血红蛋白在24 h内下降超过15 g/L。
SLE合并DAH患者的治疗主要是激素联合免疫抑制剂,多数专家推荐大剂量激素冲击疗法,接着是逐渐减量至维持口服激素剂量。免疫抑制剂首选环磷酰胺,推荐剂量为2 mg·kg-1·d-1,可维持使用数周,但应注意其不良反应[8],吗替麦考酚酯在维持疾病缓解中有一定作用[9]。有报道提出使用利妥昔单抗治疗对常规免疫抑制剂耐药的患者有效[10-14]。大剂量免疫球蛋白静脉注射疗法可作为一种强有力的辅助治疗措施,其原理目前尚未明确,多与激素﹑免疫抑制剂及血浆置换等联用有关[15-16]。 对于有持续性肺泡出血的患者可采用血浆置换术,其原理为清除其特异性自身抗体﹑可溶性免疫复合物以及参与组织损伤的非特异性炎症介质和免疫活性物质,阻止上述物质所导致的疾病进程,但Badsha等[17]指出血浆置换并不能提高SLE并DAH的生存率。表2为我们搜集的此类患者治疗措施与预后的关系。
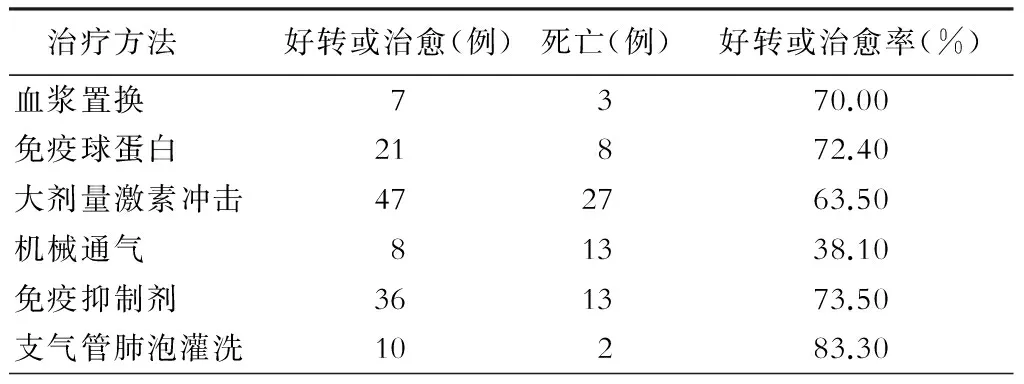
表2 不同治疗方法对SLE合并DAH的治疗效果
注:101例SLE合并DAH患者中,有些病例接受了以上6种治疗方法中的几种治疗措施
SLE合并DAH的预后不良,可能与机械通气,合并感染,激素及免疫抑制剂等药物及SLEDAI有关[18]。另外,Claridge等[19]指出液体负荷量过多会使DAH加重,此时,应谨慎增加液体负荷,以免使病情恶化。
总之,SLE合并DAH病情凶险,早期诊断、早期治疗极为重要。对于不明原因发热、出血的患者,进行免疫学血清指标检查排除SLE,有助于早期明确诊断,病情危重者使用血浆置换可以改善患者的预后。
[1] Osler W. On the visceral manifestations of the erythema group of skin diseases [Third Paper.]1904[J].Am J Med Sci,2009,338(5):396-408.
[2] Canas C, Tobon GJ, Granados M, et al. Diffuse alveolar hemorrhage in Colombian patients with systemic lupus erythematosus[J]. Clin Rheumatol, 2007, 26(11): 1947-1979.
[3] Shen M, Zeng X, Zhang F, et al. Diffuse alveolar hemorrhage in systemic lupus erythematosus:a retrospective study in China[J]. Lupus, 2010, 19(11):1326-1330.
[4] Chang MY, Fang JY, Chen YC, et al. Diffuse alveolar hemorrhage in systemic lupus erythematosus:a single center retrospective study in Taiwan[J]. Ren Fail, 2002, 24(6): 791-802.
[5] Kwok SK, Moon SJ, Ju JH, et al. Diffuse alveolar hemorrhage in systemic lupus erythematosus:risk factors and clinical outcome:results from affiliated hospitals of Catholic University of Korea[J]. Lupus, 2011, 20(1): 102-107.
[6] 王俊, 黄芳, 付建红, 等. 以肺泡出血为首发症状的系统性红斑狼疮病例分析并文献复习[J]. 中国血液流变学杂志, 2013, 23(4): 645-647, 650.
[7] 沈敏, 曾学军,范洪伟,等. 系统性红斑狼疮合并弥漫肺泡出血17例临床分析[J]. 中华医学杂志, 2009, 89(3): 201-203.
[8] Ioachimescu OC, Stoller JK. Diffuse alveolar hemorrhage:diagnosing it and finding the cause[J]. Cleve Clin J Med, 2008, 75(4):258, 260, 264-265.
[9] Al Rashidi A, Alajmi M, Heqazi MO. Hegazi, Mycophenolate mofetil as a maintenance therapy for lupus-related diffuse alveolar hemorrhage:a case report[J]. Lupus, 2011, 20(14): 1551-1553.
[10]Martinez-Martinez MU, Abud-Mendoza C. Recurrent diffuse alveolar haemorrhage in a patient with systemic lupus erythematosus:long-term benefit of rituximab[J]. Lupus, 2012, 21(10): 1124-1127.
[11]Nellessen CM, Pge U, Brensing KA, et al. Diffuse alveolar haemorrhage in a systemic lupus erythematosus patient successfully treated with rituximab:a case report[J]. Nephrol Dial Transplant, 2008, 23(1): 385-386.
[12]Pinto LF, Candia L, Garcia P, et al. Effective treatment of refractory pulmonary hemorrhage with monoclonal anti-CD20 antibody (rituximab)[J]. Respiration, 2009, 78(1): 106-109.
[13]Martinez-Martinez MU, Abud-Mendoza C.Predictors of mortality in diffuse alveolar haemorrhage associated with systemic lupus erythematosus[J].Lupus, 2011, 20(6): 568-574.
[14]Pottier V, Pierrot M, Subra JF, et al. Successful rituximab therapy in a lupus patient with diffuse alveolar haemorrhage[J].Lupus, 2011, 20(6): 656-659.
[15]Hoshi K, Matsuda M, Ishikawa M, et al. Successful treatment of fulminant pulmonary hemorrhage associated with systemic lupus erythematosus[J].Clin Rheumatol, 2004, 23(3): 252-255.
[16]陈光星, 董怡, 鞠中斌.弥漫性结缔组织病并发弥漫性肺泡出血32例临床分析[J]. 中华内科杂志, 2008, 47(5): 362-365.
[17]Badsha H, Teh CL, Kong KO, et al. Pulmonary hemorrhage in systemic lupus erythematosus[J]. Semin Arthritis Rheum. 2004. 33(6): 414-421.
[18]Isono M, Araki H, Haitani T, et al. Diffuse alveolar hemorrhage in lupus nephritis complicated by microscopic polyangiitis[J].Clin Exp Nephrol, 2011, 15(2): 294-298.
[19]Claridge S, Das P, Dorling A, et al. Plasmapheresis as rescue therapy for systemic lupus erthymatosus-associated diffuse alveolar heamorrhage[J]. BMJ Case Reports, 2011, 2: 3893
A case report and literature review of systemic lupus erythematosus with diffuse alveolar hemorrhage
ZHANGLi,DOUYan-na,MAShuang,XIAOJing,CHENGGen-yang,LIUDong,ZHAOZhan-zheng.
TheNephrologyCenteroftheFirstAffiliatedHospitalofZhengzhouUniversity,Zhengzhou450052,China
LIUDong,E-mail:liudong030@163.com
Objective To analyze the clinical characteristics of systemic lupus erythematosus (SLE) with diffuse alveolar hemorrhage (DAH), and to study the efficacy of plasmapheresis combined with hormone in SLE with DA in order to improve the level of diagnosis and treatment of rare cases, and avoid misdiagnosis and delayed treatment. Methods The clinical manifestations of 1 case of SLE with DAH in our hospital were reported, and the clinical effect of plasma exchange combined with corticosteroid for treatment of the patients was observed at the same time. A comprehensive analysis was done on DAH clinical manifestations, treatment and clinical effects of 101 Chinese SLE patients. Results This patient was a 20-year old female, and the main clinical manifestations were fever, bloody sputum, facial erythema, accompanied by vaginal bleeding. The laboratory test showed that the titer of anti-nuclear antibody (ANA) was 1:1000, anti-double stranded DNA (ds-DNA) antibody and anti-Smith antibody were both positive, and hemoglobin was progressively reduced. The chest CT showed two lung fields displayed more spiral shape and spot shape, nodule density increased shadow, and edge was blur. A diagnosis of SLE combined with DAH was made. She was given plasmapheresis combined with glucocorticoid, while giving the human normal immunoglobulin. Thereafter, hemoptysis stopped, facial erythema disappeared, anemia was significantly improved, and now she was given glucocorticoids and got reduction regularly. In our country, 101 cases were reported, and the specific clinical manifestations were described in 83 cases. These patient's ANA was all positive, 58 cases were positive for anti ds-DNA antibody, 67 cases presented with hemoptysis, 61 cases presented with fever, 71 cases presented with renal involvement, hemoglobin decreased in 74 cases, there were 80 cases of dyspnea, and 70 cases of hypoxemia. The imaging examination showed pulmonary infiltration. Through the treatment with plasmapheresis, hormone shock, immune inhibitors and other drugs, 10 patients underwent plasma exchange, 7 cases were effective; 29 cases were treated with gamma globulin, 21 cases were effective; 74 patients received high-dose corticosteroid, 47 cases were effective; 21 cases were given mechanical ventilation, 8 cases were effective; 49 cases were treated with immunosuppressive drugs, 36 cases were effective; 12 cases received the bronchoalveolar lavage, 10 cases were effective. Conclusions DAH is a rare and life-threatening complications of SLE. Early diagnosis, the use of plasmapheresis combined with hormone shock and other supportive treatment, preventing and treating the complications actively, will improve the patient’s clinical manifestations and prognosis effectively.
Systemic lupus erythematosus; Diffuse alveolar hemorrhage; Literature review
10.3969/j.issn.1671-2390.2017.03.006
河南省科技计划项目(No.142300410232)
450052 郑州,郑州大学第一附属医院肾脏病中心 郑州大学肾脏病研究所
刘栋,E-mail:liudong030@163.com
2016-04-09
2016-11-07)
