运动相关性肌肉痉挛的最新研究进展
2017-05-04康杰,张鹏
康 杰(美),张 鹏(译)
运动相关性肌肉痉挛的最新研究进展
康 杰(美)1,张 鹏(译)2
运动相关性肌肉痉挛(EAMC)是休闲运动和竞技运动中的常见病症,通常需要在运动中或运动后即刻就医。尽管EAMC发病率高,但对EAMC的病因仍然知之甚少,并且缺乏高水平的证据来指导这种病症的处理。先前关于EAMC如何产生的报告受到最新证据的挑战,这些证据表明了一种新的发生机制。本文旨在检验目前支持EAMC病因的各种观点的科学证据,着重分析有关这一复杂病症的最新观点。此外,还讨论了用于治疗和预防EAMC的各种策略,虽然其中大多数仍是观察报告,尚未通过研究实验证实。
运动相关性肌肉痉挛;机制;风险因素;治疗;预防
0 前言
运动相关性肌肉痉挛(Exercise-associated muscle cramping,EAMC)是在体育赛事中需要就医的常见病症,常见于参加长距离耐力赛的运动员中,如铁人三项、马拉松和超马拉松赛[1,2]。在其他许多运动中也有报道,包括篮球、足球、美式橄榄球、英式橄榄球、网球和自行车[2]。据报道,铁人三项选手的 EAMC发病率为 67%、马拉松运动员为30%~50%、橄榄球运动员为52%和自行车运动员为60%[1,2]。尽管EAMC具有高发病率,但研究人员对其风险因素和潜在原因尚未完全了解。肌肉痉挛可以作为各种医学病症的症状发生,包括遗传性疾病、肌肉疾病、内分泌代谢疾病、水电解质紊乱以及药物中毒等[3]。本文关注的是运动诱发的骨骼肌痉挛,不包括平滑肌痉挛或休息时发生的肌肉痉挛,以及与任何潜在疾病或药物相关的痉挛。
0 Introduction
Exercise-associated muscle cramping(EAMC)is a common condition that requires medical attention during sporting events.It is common among athletes who participate in long-distance endurance events,such as triathlon,marathon, and ultra-marathon[1,2].It is also documented in many other sports,including basketball,soccer,American football,rugby, tennis,and cycling[2].The prevalence of EAMC has been re ported for triathletes(67%),marathon runners(30%-50%),rug by players(52%)and cyclists(60%)[1,2].Despite the high prevalence of EAMC,its risk factors and underlying causes are not completely understood.Muscle cramping can occur as a symptom for a variety of medical conditions.These include genetic disorders,muscular diseases,endocrine and metabolic diseases,hydroelectrolyte disorders,and toxic and pharmacological agents[3].This review focuses on cramps that are exercise induced and excludes muscle cramping that occur in smooth muscle or at rest and cramping that is associated with any und erlying disease or drugs.
1 EAMC概述
1.1 EAMC的定义
EAMC被定义为在体育运动期间或运动后立即发生的、不自主的疼痛性骨骼肌痉挛综合征[4]。它表现为局部肌肉断续性痉挛,可发生在不同的肌肉群,通常在小腿、腘绳肌或股四头肌,其中发在生在小腿后群肌肉是最常见的[4]。
1.2 EAMC的症状
EAMC的临床症状为急性疼痛、僵硬、明显的肌肉突起,以及可能可持续几天的疼痛[5,6]。它可能没有任何预兆便突然发生,受影响的肌肉通常是随机的,当一束肌纤维松弛时,相邻束收缩,给人一种痉挛游走的印象[7,8],例如,抽搐首先可能出现在股四头肌中,随后出现在另一个肌肉群中[7]。大多数EAMC持续1~3 min,但运动员常诉说在运动后8 h仍然会发生EAMC症状[9]。这种运动后对EAMC易感性增加的时期被称为易痉挛状态[10]。EAMC可以使肌力下降[11,12],虽然在某些情况下EAMC似乎不影响运动成绩[13,14]。
1.3 风险因素
EAMC似乎在长时间、高强度赛事中发生得更为频繁。事实上,某些运动赛事的安排可能更易导致EAMC发生。在网球排名赛的多日比赛中,参赛选手通常每天不仅仅打一场比赛,而且每场比赛之间只有1 h的休息时间。这种竞赛模式易引起的肌肉疲劳,不利于每场比赛之间水和电解质的补充,并经常导致肌肉痉挛,从而影响运动比赛[15]。在对1 300名马拉松赛选手进行有关EAMC相关的风险因素的横向调查中发现,与EAMC相关的特定条件包括高强度跑步、长距离跑(>30 km)、主观肌肉疲劳,这些都反映高强度、疲劳性的体力输出。这项调查中发现的其他危险因素包括年龄较大、跑步年限较长、体重指数较高、日常拉伸运动时间较短、不良的拉伸习惯,以及痉挛的阳性家族史[16]。在一项对铁人三项运动员的前瞻性研究中,EAMC唯一的独立风险因素是在高强度比赛中发生痉挛的既往史[17]。一篇关于马拉松赛事中肌肉痉挛的综述也表明,EAMC易发生于有该病史的跑步者,并导致这些运动员过早出现肌肉疲劳[18]。
1 Overview of Exercise Associated Muscle Cramps (EAMC)
1.1 Defining exercise associated muscle cramps(EAMC)
EAMC is defined as a syndrome of involuntary painful skeletal muscle spasms that occur during or immediately after physical exercise[4].It presents as localized muscle cramping that happens spasmodically in different exercising muscle groups,usually the calf,hamstring or quadriceps muscles. The calf muscles are the most commonly affected[4].
1.2 Symptoms of EAMC
Clinically,EAMC may be recognized by acute pain, stiffness,visible bulging or knotting of the muscle,and possi ble soreness that can last for several days[5,6].It can occur suddenly with no warning.The affected muscles often appear to be randomly involved,and as one bundle of muscle fibers relax,an adjacent bundle contracts,giving the impression that the spasms wander[7,8].For example,twitches first may appear in the quadriceps and subsequently in another muscle group[7].Most EAMC incidents last 1-3 min,but athletes often complain of EAMC symptoms up to 8 hours after exercise[9]. This post-exercise period of increased susceptibility to EAMC has been termed as the cramp prone state[10].EAMC can be completely debilitating[11,12],although in some cases EAMC do not appear to affect athletic performance[13,14].
1.3 Risk factors
EAMC seems to be more frequent in long-duration, high-intensity events.Indeed,the competitive schedule of certain athletic events may predispose to EAMC.In multiday tennis tournaments,competitors often play more than one match a day,with only an hour between matches.This competition format induces muscle fatigue,impedes fluid and electrolyte replacement between matches,and often results in debilitating muscle cramps[15].Risk factors associated with EAMC in running have also been examined in a cross-sectional survey of 1 300 marathon runners.In this survey,thespecific conditions found to be associatedwith EAMC included high-intensity running,long distance running (>30 km),subjective muscle fatigue,all of which are intense and exhaustive physical efforts.Other risk factors identified in this survey were older age,a longer history of running,higher body mass index,shorter daily stretching time,irregular stretching habits, and a positive family history of cramping[16].In a prospective study of Ironman triathletes,the only independent risk factors for EAMC were a history of the condition and competing at a higherthan usualexercise intensity[17].A review on muscle cramping in marathonalso suggests that EAMC is associated with running conditions that can lead to premature muscle fatigue in runners who have a history of the condition[18].
2 EAMC的历史和病因学
2.1 肌肉痉挛的早期报告
最早有关肌肉痉挛的报告来自100年前,当时工人在矿山和造船厂湿热的条件下患有痉挛疾病[19,20]。经进一步分析发现建筑工汗液中具有较高的氯化物水平。在这些报告中,发现肌肉痉挛不仅发生在高温条件下,而且痉挛时伴随大量出汗[20]。最近,通过监测美国橄榄球运动员的中暑疾病,Cooper等观察到95%的痉挛事件发生在高温月份,此时中暑疾病的风险被评定为“高”或“极高”[21]。 正是由于这些早期观察结果,“电解质紊乱和脱水”学说被确认为EAMC的基本病因。基本上,该学说表明过度出汗和由此产生的电解质丢失可以影响肌肉和神经功能障碍,从而产生肌肉痉挛。因此,目前已普遍认为EAMC发生是因为运动员在热环境中运动,电解质随汗液丢失,导致电解质紊乱和脱水,并伴随体温升高[22,23]。
2.2 电解质紊乱和脱水学说
电解质紊乱和脱水学说表明EAMC与出汗过多或过度消耗水分造成的血清电解质浓度降低有关,特别是钠和氯[4,8,24]。 的确,在单次训练比赛或重复运动后,当汗液氯化钠丢失明显超过盐摄入量时,总是产生全身可交换钠明显减少的现象[25,26]。据估计由出汗引起的钠离子池损失达到约 20%~30%便可导致严重的肌肉痉挛[15,27]。当疑似出现所谓的钠离子池不足时,汗液中其他较低程度的电解质损失,即钙、镁和钾也被认为与运动中或运动后肌肉痉挛有关[28-31]。电解质紊乱学说的主要前提是假定汗液钠浓度增高或“咸汗”导致钠消耗,从而引起EAMC[25,32]。然而,这一学说的病理生理学基础仍不明确。
由于汗液钠浓度总是低渗的[33,34],因此只有伴随着体液的大量丢失,才能通过汗液发生明显的钠丢失。这意味着运动员发生 EAMC时同时会出现脱水和明显的钠丢失。过度脱水会减少血容量,为补偿损失的血容量,组织液中的水将转移到血管内以维持中心血容量[35-37]。 随着继续出汗,组织间隙越来越收缩[35],由于运动后继续出汗,这一过程甚至可以在运动后持续进行,直至体温恢复到运动前水平[36]。由于组织间隙收缩,某些神经肌肉接点(尤其先发生在股四头肌或腘绳肌)可能由于机械变形而过度兴奋。所产生的机械压力变化可以诱发运动神经元自发性放电,从而导致痉挛[38,39]。图 1说明了出汗引起的脱水如何逐步触发EAMC的过程。
痉挛发作也可归因于以下事实:运动神经元轴突的末端分支,特别是无髓鞘的神经末梢,接触到水平增加的兴奋性细胞外物质,例如乙酰胆碱或电解质(即钠和钾)[40-42]。随着更多的水从组织间隙转移到血管内,毗邻的神经末梢和其它神经末梢及突触后膜同样受到影响。这可以解释为什么经常观察到痉挛游走现象,也就是痉挛在不同的肌肉纤维和肌肉束中交替发生[43]。
2.3 EAMC起始病因的反面证据
如上所述,对电解质紊乱和脱水学说的支持主要来自基于病例报告或观察的研究,并没有记录水合状态的实际测量。矿工出现痉挛是因为他们在湿热环境工作,出汗较多[20,39]。最近,对美式橄榄球运动员的研究表明,大多数痉挛发生在炎热的月份,运动员在该环境中发生中暑的风险很高[21]。这个学说的其他证据来自案例研究和观察工作,这些研究中运动员有大量出汗的情况[15,25,26]。
电解质紊乱和脱水学说似乎与许多最新的证据相矛盾。4项前瞻性队列研究显示在马拉松或铁人三项运动员中,血清电解质异常和 EAMC之间并不相关[6,13,14,44]。研究结果表明EAMC机制是汗液浓度增加(“咸汗”)导致钠消耗,而不是血清电解质浓度的变化[45,46]。然而,钠损耗如何导致EAMC仍没有生理学解释。由严重钠丢失引起的低钠血症与休息时的全身肌肉痉挛有关[47]。可是,如上所述,在患有EAMC的大多数运动员中,痉挛发生在运动期间重复收缩的局部肌群。对于电解质系统不平衡如何导致局部肌肉痉挛尚没有合理的生理学解释。
至于脱水,有人认为过度出汗是导致EAMC的主要原因[4]。然而在上述 4个前瞻性队列研究中,将计算出的体重变化、血容量或血浆容量用作身体水合状态的指标,发现当时发生痉挛的运动员脱水情况并不比未发生痉挛的运动员脱水情况严重。因而,脱水和肌肉痉挛之间的直接关系假设不被支持[6,13,14,44]。
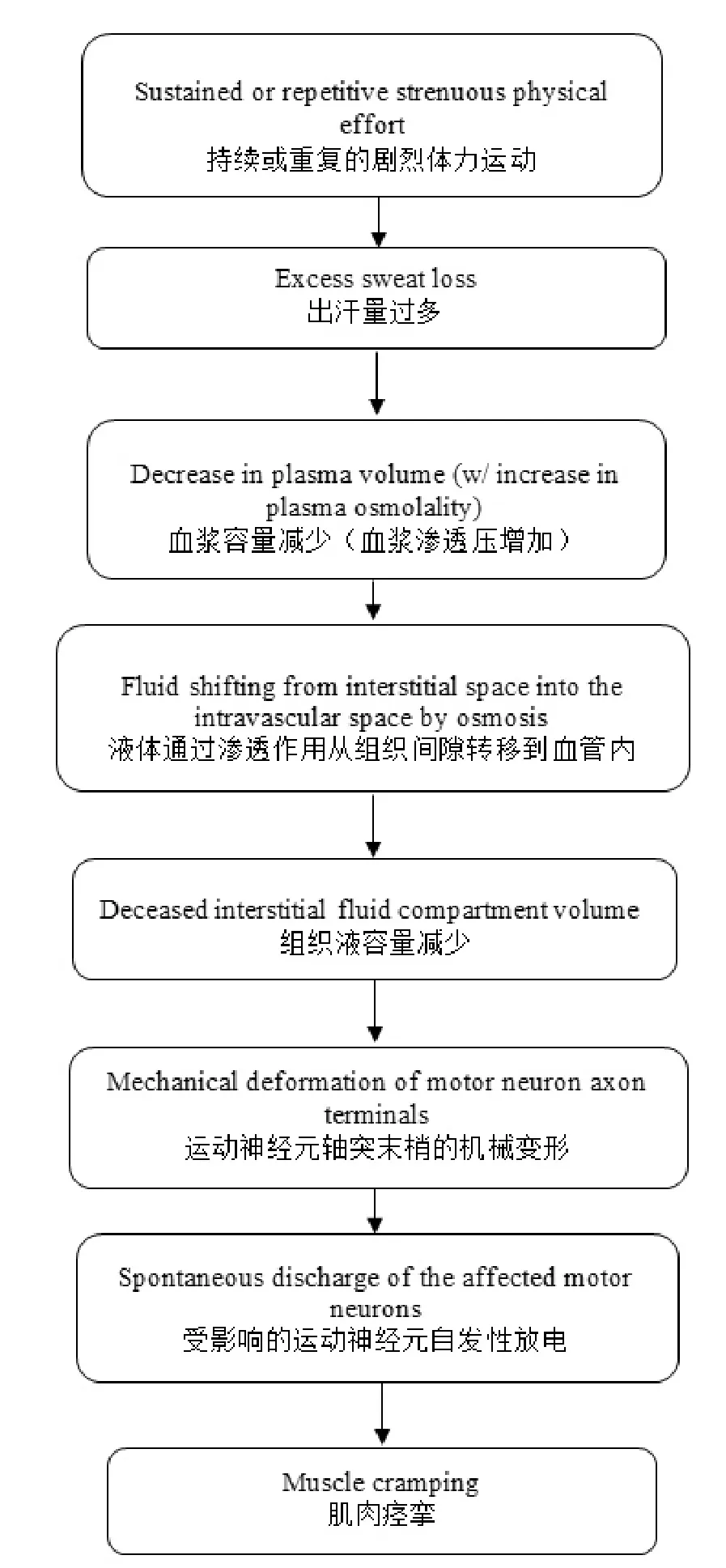
图1 EAMC的电解质紊乱和脱水学说的示意图Figure 1 Schematic Illustration of the Electrolyte Imbalance and Dehydration TheoryofExerciseAssociated Muscle Cramps(EAMC)
若运动员在凉爽和温度控制环境中运动时发生EMAC,使用电解质不平衡和脱水学说对其进行解释也不成立[13,48]。例如,Maughan报告称,即使环境温度为10~12℃,一些马拉松运动员(约18%)仍然产生EAMC[13]。因此,尽管EAMC可能在高温环境下更为频繁地发生,但是,湿热环境并不是发生EAMC的必要条件[21]。该研究还显示,在患有和未患EAMC的跑步者之间,血容量和体重的减少没有显著差异。
总的来说,电解质紊乱和脱水学说具有局限性。支持性证据来自于无法提供任何因果结论的病例报告或调查。虽然EAMC可能在运动期间存在显著电解质和/或液体丢失的情况下出现,但也可以归因于其它因素,例如代谢物的积累、能量不足、肌肉损伤,以及训练水平和/或环境适应能力欠缺。
2.4 热痉挛——用词不当
病例报告和观察记录经常将痉挛产生与在湿热环境下进行体力活动相关联,这导致了“热痉挛”或“运动性热痉挛”的名称的普遍使用。这些术语通常与EAMC同义使用[2,15,43,45,49]。 支持使用这一术语的更多实质性数据来自于一项流行病学研究,文中美国橄榄球运动员在热指数为“高”或“极高”环境中训练相比“低”或“中等”的环境中训练时,“热痉挛”的发生更加常见[21]。必须注意的是,这些炎热和潮湿的天气条件也发生在赛季训练的前2~3周,此时运动员很可能不能妥善调整状态和/或适应炎热的天气条件而容易导致疲劳。在适宜温度至凉爽温度下运动的人员也会发生 EAMC[13,48],在游泳运动员中发现极端寒冷的条件也与EAMC相关[50]。还有报道称,EAMC的发生与核心体温的升高没有直接关系[13]。显然,热本身不是运动中肌肉痉挛产生的直接原因。因此,术语“热痉挛”是不准确的,应当避免使用。
2 History and Original Etiology of EAMC
2.1 Early reports of muscle cramps
The earliest reports of muscle cramps come from 100 years ago,when labors in hot and humid conditions of the mines and shipyards suffered from cramps[19,20].Upon further analysis,it was noticed that the builders had a high chloride level in their sweat.In these reports,it was noted not only that muscle cramping occurred in the heat,but also that cramps were accompanied by profuse sweating[20].More re cently,by monitoring external heat illness among American football players,Cooper et al.observed that 95% of the cramping incidents occurred in hot months when the risk of developing heat illness was “high”or “extreme”[21].It was because of theseearly observations that the“electrolyte imbalance and dehydration”theory was developed as an underlying cause for EAMC.In principle,this theory suggests that overly sweating and thus loss of electrolytes can cause muscles and nerves that innovate them to malfunction,thereby producing muscle cramps.It is now a common belief that EAMC happens because athletes exercise in the heat,lose electrolytes in their sweat,and the resultingelectrolyte imbalance and dehydration combines with high body temperature[22,23].
2.2 The electrolyte imbalance and dehydration theory
The electrolyte imbalance and dehydration theorysuggests that EAMC is related to the decreased concentration of serum electrolytes,particularlysodium and chloride,resulting from excessive sweating or overconsumption of water[4,8,24].Indeed, a sizeable whole-body exchangeable sodium deficit always develops following a single long race,match,game,or training session or repeated exercisebouts when sweat sodium and chloride lossessignificantly exceed salt intake[25,26].An estimated sweat-induced loss of 20%-30%of the sodiumpool has been linked to severe muscle cramping[15,27].Other electrolytes lost in sweatto a much lesser degree,namelycalcium,magnesium,and potassium,have also been implicatedas the cause of muscle cramping during or afterexercise when purported deficiencies are suspected[28-31].The chiefpremise behind the electrolyte imbalance theory is to suggest that the mechanism for EAMC is increased sweat sodium concentrationor"salty sweating",resulting in sodium depletion,which then causes EAMC[25,32].However,the pathophysiologicalbasis for this hypothesis remains poorly defined.
Because sweat sodium concentration is always hypotonic[33,34],a significant loss of sodium through sweat can therefore only occur if there is an accompanying large loss of bodi ly fluid.This would mean that dehydration would accompanyany significant sodium loss in athletes experiencing with EAMC.Overly dehydration will reduce plasma volume.To compensate for the loss in plasma volume,water fromthe interstitial fluid compartment shifts to the intravascularspace to maintain central blood volume[35-37].As sweating continues,the interstitialfluid compartment becomes increasingly contracted[35].This can persist even after exercise as sweating continuesand body temperature returns to a pre-exercise level[36].Consequent to a contracted interstitial compartment,certain neuromuscular junctions (especially first in the quadriceps or hamstring muscles)could become hyper-excitable by mechanical deformation.The resulting change in mechanical pressure can induce spontaneous discharges of the affected motor neurons, thereby causing cramps[38,39].Figure 1 illustrates a step-by-step processofhow sweat-induced dehydration may trigger EAMC.
Cramp discharges may also be attributed to the fact that terminal branches of motor axons,especially those that are unmyelinated,are exposed to increased levels of excitatory extracellular substances such as acetylcholine or electrolytes(i. e.,sodium and potassium)[40-42].As more water is shifted away from the interstitial compartment to the intravascular space, adjacent and other nerve terminals and post-synaptic membranes could be similarly affected.This may explain why cramping is often observed in various muscle fibers and bundles alternately contracting and relaxing[43].
2.3 Evidence against the original etiology of EAMC
As mentioned earlier,support for the electrolyte imbalance and dehydration theory comes mainly from research based on case report or observations with no actual measures of hydration status reported.Miners develop cramps because of their sweat losses while working in hot and humid conditions[20,39].More recently,research on American football re vealed that most crampingincidents occurred in hot months when football players trained in an environment where the risk of developing heat illness was high[21].Other evidence for this theory comes from case studies and observational work in which large sweat losses occurred in exercising athletes[15,25,26].
The electrolyte imbalance and dehydration theory seems to contradict many recent evidences.Four prospective cohort studies have shown no relationship between serum electrolyte abnormalities and EAMC in marathon runners or triathletes[6,13,14,44].The findings have led to the suggestion that increased sweat concentration (‘salty sweating’)resulting in sodium depletion,rather than changes in serum electrolyte concentrations,is the mechanism for EAMC[45,46].However,the physiologicalexplanation for how sodium depletion may cause EAMC remains unavailable.Hyponatremia resulting from a significant loss of sodium has been associated with general-ized muscle cramping at rest[47].However,as mentioned earlier,in most athletes experiencing EAMC,cramping occurs in the localized muscle groups involved in repetitive contractions during exercise.There is no plausible physiological explanation of how a systemic imbalance of electrolytes could result in localized muscle cramps.
As for dehydration,it has been argued that excessive sweating is the primary cause of EAMC[4].However,in the four prospective cohort studies mentioned above in which calculated body weight changes and volume of blood or plasma were used as indicators of hydration status,it was found that cramping athletes at the time of were not more dehydrated than non-cramping athletes.Thus.the hypothesis of a direct relationship between dehydration and muscle cramping was not supported[13,6,14,44].
The electrolyte imbalance and dehydration theory also does not stand when it is usedto explain EAMC that occurs in athletes exercising in cool and temperature-controlled environ ments[13,48].Forexample,Maughan[13]reported that somemarathoners (~18%)still developed EAMC even though the ambient temperature was 10 to 12℃.Thus,it is unlikely that a hot and humid environment is required for the development of EAMC,although EAMC may occur more frequently under conditions of elevated ambient temperatures[21].This same study also revealed no significant differences inlosses of plasma volume and body weight between runners with and without EAMC.
Overall,the dehydration-electrolyte imbalance theory has limitations.Supporting evidence wasbased on case report or surveys that could not provide any cause-effect conclusions. Although EAMC may appear in the presence of significant electrolyte and/or fluid losses during exercise,it can also be attributedto other factors such as accumulation of metabolites, fuel deficiency,muscle damage,and a lack of conditioning and/or acclimatization.
2.4 “Heat cramps”-a misnomer
Case reports and anecdotal observationsoften related the development of cramping to physical activity performed in hot and humid conditions,and this has led to the use of"heat cramps"or"exertional heat cramps".These terms areoften used synonymously with EAMC[2,15,43,45,49].More substantive data to support the use of this terminology came from an epidemiological study in which the term"heat cramps"was reported to be more common when American football players trained in an environment where the heat index was"high"or "extreme"compared with"low"or"moderate"[21].Itmust be noted that these hot and humid weather conditionsalso occurred during the first 2-3 weeks of training in a season when players were also most likely less well-conditioned and/or acclimatized to the heat.EAMC is also known to occur in individu-als exercising in moderate to cool temperatures[13,48]and exposure to extreme cold has also been associated with EAMC in swimmers[50].It has also been reported that the development of EAMC is not directly related to an increased core temperature[13].Clearly,heat alone is not a direct cause of muscle cramping during exercise.As such,the term"heat cramps"is inaccurate and its use should be discouraged.
3 有关EAMC的最新发现
3.1 异常神经肌肉控制学说
在体育竞赛和训练或其他各种剧烈的体力活动中,所涉及的肌肉受到长期反复的负荷,可导致肌肉或肌腱劳损和局部疲劳。异常神经肌肉控制学说表明,肌肉疲劳破坏了外周肌肉感受器的正常功能,因此导致肌梭的兴奋性传入活动的增加,而高尔基腱器官的抑制性传入活动降低,两者共同导致α运动神经元向肌肉纤维放电的增加,从而产生局部肌肉痉挛[4]。这一学说可以通过动物研究予以支持, 此研究在离体的猫腓肠肌上使用了肌电图记录[51,52]。在这些研究中,通过电刺激使肌肉产生疲劳,发现随着肌肉疲劳的发展,肌梭的 Ia和 II型传入纤维冲动发放增加,并且来自高尔基腱器官的Ib型传入纤维冲动发放减少[51,52]。换句话说,肌肉痉挛可以被视为持续的α运动神经元放电的结果,这种现象发生时,肌梭的兴奋性活动增强触发了非自主肌肉收缩,且不能被抑制这种肌肉反应的高尔基腱器官所拮抗。图2基于异常神经肌肉控制学说对肌肉痉挛的产生做出了更详细的解释。
值得注意的是,当肌肉在已经收缩的状态继续缩短时,更容易发生局部痉挛[4,41]。这是因为当肌肉处于缩短状态时,高尔基腱器官的抑制活动将比正常情况减少更多,从而导致α运动神经元的抑制和兴奋之间更大的不平衡[53]。这也许可以解释为什么小腿肌肉痉挛在游泳运动员中如此普遍。这是因为在大多数游泳比赛中,游泳运动员的踝关节必须跖屈,而这需要小腿肌肉保持适度收缩。 至于过度负荷和疲劳所引起的肌肉痉挛,其潜在风险因素包括年龄较大、拉伸习惯差、调节功能不足、痉挛既往史、过度的运动强度、过长的持续时间以及相关的代谢紊乱(即,肌糖原耗竭)[18,54]。

图2 EAMC异常神经肌肉控制学说的示意图Figure 2 Schematic Illustration of the Altered Neuromuscular Control Theory of Exercise Associated Muscle Cramps(EAMC)
3.2 支持异常神经肌肉控制学说的证据
这一学说首先于 20世纪 90年代初通过观察性研究提出,研究中1 383名马拉松运动员对关于EAMC的问卷做出了回答[16]。在这些跑步者中,536名(26%)报告了EAMC病史,其中大多数(60%)表示肌肉疲劳与EAMC的发病相关。这一发现与Maughan的研究一致,他也发现EAMC的发生在马拉松赛的后期更为常见[13]。关于运动强度增加和EAMC相关的更具说服力的证据来自对铁人三项运动员进行的前瞻性队列研究[17]。在这项研究中,参加铁人三项比赛的 210名铁人三项运动员为受试者,对所有受试者的训练历史、个人最好成绩,以及比赛之前的痉挛病史进行了调查。结果表明,与没有发生EAMC的运动员相比,发生EAMC(N=44)的运动员在比赛期间的运动强度更高,并且比赛用时较少,尽管他们的准备过程和历史成绩近似。这些结果表明,痉挛组中更少的比赛用时(或运动强度增加)是这些铁人三项运动员发生EAMC的独立危险因素。在一项使用专门设计的用于引起小腿肌肉疲劳的运动方案的研究中,记录了运动期间肌肉痉挛的高发生率[55]。 这项研究还表明,与无液体补充相比,口服补充碳水化合物和电解质在使用小腿疲劳方案后导致EAMC的发作延迟。看来为运动员提供更多的碳水化合物可以减轻EAMC。
肌电图(EMG)的使用使研究人员更确信EAMC是由异常神经肌肉控制介导这一观点。 在上述讨论的研究[51,52]中,肌电图用于在EAMC发生时客观地跟踪疲劳肌肉中α运动神经元的放电。例如,在肌电图中观察到,EAMC发生之前,肌肉抽搐情况增加。然而,随着疲劳运动继续,肌电图中出现一个更大的变化并且与肌肉完全痉挛同时发生。通过使用肌电图来比较发生和没有发生EAMC的铁人三项运动员,Sulzer等人发现,患有EAMC的铁人三项运动员的肌电图基线活动在痉挛肌中明显高于非痉挛肌[44]。有趣的是,在这些受试者中,EAMC与电解质消耗或脱水并不相关。
被动拉伸是最常见和有效的缓解急性肌肉痉挛的疗法[53,56-58]。 支持电解质紊乱和脱水学说的那些人也认为它是有效的治疗方法[43,59]。 被动拉伸增加肌肉的张力,从而增加高尔基腱器官对 α运动神经元的抑制性控制[52,53]。这一机制对异常神经肌肉控制介导EAMC的假说提供了进一步支持。
3.3 EAMC中的其他病因学因素
已推测出在脊髓水平改变神经肌肉控制的其他促进EAMC发展的因素。首先是由疲劳运动引起的肌肉损伤,导致反射性“痉挛”,从而引起持续的非自主收缩。第二种可能性是来自其它外周感受器 (例如肌肉内化学感受器、压力感受器或疼痛感受器)的信号改变,可引起来自中枢神经系统的反应,从而改变神经肌肉控制[53]。在一项涉及铁人三项运动员的前瞻性队列研究中,与EAMC相关的一个独立危险因素是具有EAMC既往史[17]。此外,如前所述,一项横向研究调查了 1 383名马拉松跑步者[16],痉挛阳性家族史也被报告为EAMC的风险因素。在这种情况下,不能排除EAMC的遗传倾向。其他提出EAMC病因学的理论是碳水化合物摄入量不足、糖原耗尽、生物力学或跑姿不正确、丘陵地带或凹凸不平的地形,以及在比赛前和比赛中缺乏足够的按摩[4]。
3 Recent Discoveries on EAMC
3.1 The altered neuromuscular control theory
During sports competition and training or a variety of other intense physical activities,repeated or extended loading on selected muscles can lead to muscle or tendon strain and localized fatigue.The altered neuromuscular control theory suggests that muscle fatigue disrupts the normal functioning of peripheral muscle receptors and thus causes an increase in excitatory afferent activity within the muscle spindle and a decrease in inhibitory afferent activity within the Golgi tendon organ,both of which then lead toan increase in alpha motor neuron discharge to the muscle fibers,producing a localized muscle cramp[4].This theory can be supported by animal studies that used isolated gastrocnemius muscles derived from cats and electromyographic recordings[51,52].In these studies, muscle fatigue was introduced via electric stimulation.It was found that as muscle fatigue developed,there was an in creased firing rate of the muscle spindle’s type Ia and II afferents concomitant with a decrease in the type Ib afferent activity from the Golgi tendon organ[51,52].In other words,muscle cramps can be viewed as a consequence of a sustainedalpha motor neuron discharge that occurs when the enhanced excitatory activity of the muscle spindle that triggers an involuntary muscle contraction is unopposed by Golgi tendon organsdesigned to inhibit such a muscular response.Figure 2 ill ustrates more detailed explanations of how muscle cramps may come about based on the altered neuromuscular control theory.
It is worth noting that these localized cramps are more likely to occur when the muscle is contracting in an already-shortened position[4,41].This is because when muscle is in a shortened position,the inhibitory active of the Golgi tendon organ will reduce even more than normal,causing a greater imbalance between inhibitory and excitatory drives to the alpha motor neuron[53].This may explain why calf muscle cramps are so prevalent in swimmers.This is because in most swimming races swimmer must swim with the ankles being planter flexed,which requires calf muscles to remain modestly contracted.The potential risk factors associated with overload and fatigue-related muscle cramping also include older age,poor stretching habits,insufficient conditioning,cramping history,excessive exercise intensity and duration,and related metabolic disturbances (i.e.,muscle glycogen depletion)[54,18].
3.2 Evidence supporting the altered neuromuscular control theory
The theory may be first brought up in the early 1990s by an observational study in which 1383 marathon runners responded to a questionnaire on EAMC[16].Of these runners, 536(26%)reported a history of EAMC and a majority(60%) of them indicated that muscle fatigue was associatedwith the onset of EAMC.This finding concurs with those ofMaughan[13]who also discovered that development of EAMC was more common in the latter stages of a marathon race.Stronger evidence linking increased exercise intensity and EAMC comes from a prospective cohortstudy in Ironman triathletes[17].In this study,210 triathletescompeting in an Ironman triathlon acted as subjects and all the subjects were surveyed for their training history,personal best performances,and cramping history prior to the race.Results of this study showed that those who developed EAMC(n=44)exercised at a higher intensity during the race and had faster overall race time despite similarpreparation and performance histories as compared to those who did not develop EAMC[17].These findings indicate that the faster racing time(or increased exercise intensity)inthe cramp group was an independent risk factor for thedevelopment of EAMC in these triathletes.In a study using an exercise protocol specifically designed to cause fatigue of thecalf muscles,a high incidence of muscle cramping during exercise was documented[55].This study also reveal that supplementingcarbohydrate and electrolytes orally,compared with no fluid administration,resulted in a delay inthe onset of EAMC following a calf fatiguing protocol.It appears that providing athletes with more carbohydrate can alleviate EAMC.
The use of electromyography (EMG)has allowed researchers to be more convincing of the argument that EAMC is mediated by an altered neuromuscular control.In the stud ies discussed earlier[51,52],EMG was used to objectively trace the discharge of alpha motor neurons in fatigued muscles as EAMC developed.For example,a modest increasein EMG was noticed as muscle twitches prior to EAMC.However,as fatiguing exercise continues,there was a much greater change in EMG that coincided witha full-blown muscle cramp.By using EMG to compare ironman triathletes with and without EAMC,Sulzer et al.found that baseline EMG activity in triathletes who suffered from EAMC was significantly higher in a cramping thana non-cramping muscle[44].Interestingly,in these subjects,EAMC was not associated with electrolyte depletion or dehydration.
Passive stretching is the mostcommon and effective therapy to relieve acute muscle cramping[53,56-58].It is also regarded as effective treatment by thosewho support the electrolyte depletion and dehydrationtheory[43,59].Passive stretchingincreas es the tension in a muscle,thereby increasing the Golgi tendon organ’s inhibitory input to the alpha motor neuron[52,53]. This mechanismoffers further support for the hypothesis that abnormalneuromuscular control mediates EAMC.
3.3 Other etiological factors in EAMC
Other factorshave been speculated to alterneuromuscular control at the spinal cord level,thereby contributing to the development of EAMC.The first of theseis the possibility that muscle injury or damage,resultingfrom fatiguing exercise, could cause a reflex"spasm",andthus lead to a sustained involuntary contraction.Thesecond possibility is that changing signals fromother peripheral receptors,such as chemically sensitive intramuscularafferents,pressure receptors,or pain receptors,couldelicit a response from the central nervous system, which mayalterneuromuscular control of the muscles[53].In a prospective cohort study involving triathletes,one independent risk factorassociated with EAMC was a previous history of EAMC[17].In addition,in a cross-sectional study that surveyed 1383 marathon runners as mentioned earlier[16],a positive family history of cramping has also been reported as a risk factor for EAMC.In this context,a genetic predisposition to EAMC cannot be ruled out.Among other theories that have been proposed for the etiology of EAMC arean inadequate intake of carbohydrate,glycogen depletion,poor biomechanics or running gait,hilly terrain,and lack of adequate massage be-fore and during a game[4].
4 治疗和预防
4.1 治疗
既然关于EAMC病因存在多种解说,所以很难为治疗或预防策略提供唯一答案。因此,有许多干预措施可用于治疗肌肉痉挛。这些治疗包括拉伸痉挛肌肉,降低运动强度,按摩,温热疗法,冷冻疗法,补充运动饮料、盐和电解质、pickle juice(腌黄瓜汁)运动饮料,静脉输注和经皮神经电刺激。这些治疗选择方案很多是观察记录,或缺乏实验研究支持。EAMC可以被视为多种病理过程的结局,并且可能不同的运动员导致相似 EAMC表现的机制不同。因此,对一名运动员有效的治疗,不一定对其他运动员也有效。下面对一些常用的治疗方法进行讨论。
电解质紊乱和脱水学说表明,摄取含有电解质的液体有助于使组织间隙或细胞外容量正常化, 从而减轻EAMC。然而,由于许多运动饮料中的电解质较少,即使运动员正常出汗和丢失汗钠含量,也可能难以充分替代运动期间损失的电解质含量。请注意,液体和电解质在喝下后不能立即被吸收,也就是说,即使低渗液体,也需要至少13 min被吸收到循环系统中[60]。基于脱水—电解质紊乱和EAMC之间存在关系这一假设,美国国家体育医务管理员协会建议,在有倾向发生肌肉痉挛的运动员的饮料中添加0.3~0.7 g/L的盐,以避免肌肉痉挛[61]。其他运动员建议根据EAMC[49]的发生频率,在运动饮料中添加更多的钠(约3~6 g/L)。一旦发现有肌肉抽搐或轻度痉挛的迹象,立即口服高盐溶液(例如,一次口服或在5~10 min内分次服用添加3 g盐的0.5 L碳水化合物—电解质饮料),被证明能够有效缓解痉挛或防止肌肉震颤发展成为完全的EAMC[15]。服用高盐溶液后,通常运动员可立即恢复训练或比赛,并且在一个小时或更长时间内不再发生肌肉痉挛或抽搐症状[15],尽管仍然需要每隔一定时间服用额外的低钠液体。
其它经常选择用于缓解EAMC的物质包括pickle juice(腌黄瓜汁)运动饮料、奎宁和电解质,例如镁、钾和钙。 一项病例报告显示,使用 pickle juice(腌黄瓜汁)运动饮料来治疗EAMC,当摄入少量高浓度酸性盐水后(30~60 mL),可以在 35 s内缓解痉挛[48]。 然而, 这种效果被认为是由于pickle juice(腌黄瓜汁)运动饮料含有乙酸,可以在口咽部引发神经反射,从而在痉挛的肌肉中增加抑制性神经递质的活性[62]。奎宁是一种用于治疗由蚊子叮咬引起的疟疾的药物,但也常用于治疗各种原因引起的痉挛。一项对23项临床试验进行的Cochrane综述发现,与安慰剂相比,奎宁可以降低痉挛的频率、强度和天数,但不能降低持续时长,不过与安慰剂相比,使用奎宁导致血小板减少症的风险显著增加[63]。虽然据报道镁补充是用于预防复发性痉挛的最有效疗法[64],但大多数使用者报告这种方法作用很小或者没有帮助。此外,富钾补充剂或食物以及其他矿物质补充剂,如钙补剂,尚未被证明能有效缓解热痉挛的症状[15,32]。
如果运动员没有潜在疾病,那么EAMC最常见的治疗是拉伸[41]。事实上,适当的拉伸已被证明对所有类型的肌肉痉挛都有效, 包括那些与热相关的肌肉痉挛[5,7,10,65]。因此,推荐使用适当拉伸以缓解痉挛。被动拉伸增加了肌肉的张力,从而增加高尔基腱器官对α运动神经元的抑制性神经传入[52,53],这将减少 α运动神经元的活动,减少EAMC发生的可能性。其他减少运动神经元活动从而减轻EAMC的相关方法包括按摩、拮抗肌群的主动收缩和局部冰敷。当然,降低整体运动强度和改变受累肌肉的负荷也是有效的[38]。
最近,已致力于评价使用诸如辣椒、姜、芥菜和肉桂等食物的提取物来解决EAMC的方法。此类食物提取物可以激活瞬时感受器电位通道(TRP通道),此通道能够中断过度兴奋的运动神经元活动[66]。TRP通道是位于口、食道和胃中的一组离子通道,可调节离子(即带电粒子如钠离子和钾离子)穿过细胞膜的流动。最近有证据表明,口服TRP通道激动剂,如肉桂、胡椒或芥末,可以通过抑制 α运动神经元的兴奋性,减弱肌肉痉挛的强度和 /或持续时间[67,68]。 在这些研究中肌肉痉挛是通过电刺激产生的,因此这种预防方法尚未在更自然的运动性肌痉挛的临床试验中得到验证。
4.2 预防
EAMC的病理生理学机制极有可能是多因素和复杂的,因此预防 EAMC也需要多种方法。热环境发生的EAMC似乎能够通过保持水电解质平衡得到预防。监测运动员的体重是一种确保充分补充液体的简单方法。美国国家体育医务管理员协会和美国运动医学院都建议,在训练或竞赛中体液丢失不能超过体重的 2%[43,61]。运动员在比赛前至少1 h,摄取1 L水或低渗运动饮料,可以确保大部分液体、电解质和营养物质得到吸收,并且在竞赛开始时能够为身体所用。此外,在运动和竞赛期间,应提供运动员容易获得并易于吸收的饮料。出汗和钠丢失多的运动员,或者有EAMC既往史的运动员,在持续时间较长的运动中,需要额外补充钠以保持盐平衡[7],在出汗量较大时,可能需要将每日膳食盐量增加至 5~10 g/d[43],这在训练中的热适应阶段特别重要。在一项案例报告中,Bergeron证明,通过计算汗液钠丢失量并在运动期间和之后进行补充,两名先前有EAMC病史的网球运动员,能够在热环境下圆满完成比赛[15]。
如上所述,EAMC的主要病因是肌肉疲劳。因此,预防策略也应该关注运动员的适当恢复调节。要真正模拟竞赛或比赛状况,高强度的耐力训练是必需的。随着耐力的增加,肌肉在既定水平的强度下不容易发生痉挛。耐力训练可扩大血容量和细胞外液体积并延迟神经肌肉疲劳[69,70],也可以作为预防EAMC的一种有效手段。运动员受伤后恢复比赛时特别容易发生EAMC,因为他们很可能提前发生肌肉疲劳,排汗量减少,对高温环境的适应能力下降[71]。适当的康复进程能够预防运动员过度应激,同时确保在重返竞赛前充分恢复专项体能。
还应实施针对肌梭和高尔基肌腱器官的预防训练,以延迟神经肌肉疲劳的发生,并因此减少EAMC的发作。增强式训练是值得考虑的一种练习方法。这种爆发力练习可以训练运动单位,以便随着运动强度的增加而更有效地工作。据报道,增强式训练可以借助肌梭和高尔基腱器官的训练提高神经肌肉控制的效率,从而使肌肉更耐疲劳[72,73]。
已采取的其他预防措施包括:(1)纠正技术错误、肌肉不平衡和 /或姿势;(2)常规拉伸肌肉;(3)进行充分的热身;(4)在比赛之前和期间使用按摩疗法;(5)穿着弹力裤袜;(6)适应热环境;(7)使用矫形鞋袜和 /或矫形鞋垫。虽然,这些预防措施尚缺乏实验证据。
鉴于上述讨论,可以遵循以下建议,以预防EAMC的发生。
(1)参照比赛强度进行训练,或者相反,根据训练中获得的能力水平进行比赛。
(2)了解您的训练和比赛环境因素包括湿度、温度、室内与室外、海拔高度和地理环境,以及它们与通常的训练环境有何不同。
(3)如果你过去已发生过痉挛,考虑所有可能引起痉挛的因素,即强度、训练量、高度、地理环境的剧烈变化,以便相应地规划你的训练和比赛。
(4)学习识别EAMC的早期预兆,并采取相应措施。
(5)最易发生痉挛的肌肉是那些在小幅度活动范围内重复使用的肌肉,因此在训练时注重训练方式,避免急性“制动”,并尝试采用适当的髋关节和膝关节屈伸动作来增加步幅。
(6)如果你是一个“大量出汗的人”,一定要增加饮食中的盐摄入量,并摄取含有较高钠含量的液体,尤其是在较热、较潮湿的月份。
(7)盐片或盐丸是一种简单的方法,但需要在训练中学会如何使用,因为一些人可能会出现胃部不适。
(8)摄入足够的营养,特别是碳水化合物,以防止运动过程中过早的肌肉疲劳。
(9)考虑对关键肌肉群进行增强式训练。
(10)常规拉伸的同时,考虑配合动作,如主动屈曲拮抗肌并按摩痉挛或易痉挛肌肉。
4 Treatment and Prevention
4.1 Treatment
With multiple theories about the cause of EAMC,it is difficult to provide a single answer for a cure or prevention strategy.Consequently,there are many interventions available for the treatment of muscle cramps.These treatment options include stretching of the affected muscle,decreasing exercise intensity,massage,thermotherapy,cryotherapy,sports drinks, salt and electrolytes,pickle juice,intravenous infusion,and transcutaneous electric nerve stimulation.Many of these treatment options are anecdotal or not supported by experimental research.EAMC can be viewed as the endpoint of a variety of pathways and different athletes may have different mechanisms leading to very similar-appearing EAMC.Therefore,a treatment that works for one athlete may not be effective one for others.Some of the commonly used treatment options are discussed as follows.
The electrolyte disturbance-dehydration theory suggests that ingesting fluids containing electrolytes helps normalize the interstitial or extracellular volume,thereby alleviating EAMC.However,owing to a small quantity of electrolytes in many sports drinks,it may be difficult to sufficiently replace the volume of electrolytes lost during exercise even if the athlete has modest sweat losses and sweat sodium content.Note that fluids and electrolytes are not absorbed immediately after ingestion;that is,even hypotonic fluids require at least 13 minutes to be absorbed into the circulatory system[60].Based on the assumption that a relationship between dehydration-electrolyte imbalance and EAMC exists,the National Athletic Trainers’Association recommends that athletes prone to muscle cramping add 0.3 to 0.7 g/L of salt to their drinks to a vert muscle cramps[61].Others have recommended adding higher amounts of sodium (about 3 to 6 g/L)to sports drinks based on the frequency of EAMC[49].At the first sign of muscle twitches or mild cramps,a prompt oral bolus of a high-salt solution (e.g.,0.5 L of a carbohydrate-electrolyte drink with 3 g of salt added consumed all at once or over 5-10 min)has been proven effective in relieving cramping or preventing muscle fasciculationsfrom developing into a full-blown EAMC[15].After such a high-salt solution bolus,athletes can often promptly resume training or competition effectively without muscle cramping or twitching symptoms for an hour or more[15],although additional lower-sodium fluid should be consumed at regular intervals.
Other substances often chosen to relieve EAMC are pick le juice,quinine,and electrolytes such as magnesium,potassium,and calcium.A case report for using pickle juice to treat EAMC revealed that ingesting of a small volume of highlysalty and acidic brine(30 to 60 mL)could relieve cramp with in 35 s[48].This effect was,however,attributed to the fact that pickle juice contains acetic acid that can trigger a re flex, probably in the oropharyngeal region,that acts to increase inhibitory neurotransmitter activity in cramping muscles[62].Quinine is a medication used to treat malaria caused by mosquito bites,but also often prescribed to treat cramps of all causes. A Cochrane review of 23 clinical trials has concluded that quinine reduces cramp frequency,intensity,and days,but not duration,compared with placebo,and that there is a significantly greater risk of thrombocytopenia for quinine compared with placebo[63].Though magnesium supplementation has beenreported to be the most treatment used to prevent recurrent cramping[64],most users report this method to be of little or no help.Additionally,potassium-rich supplements or foods or other mineral supplements such as calcium have not been proven effective in relievingsymptoms associated with heat-related cramps[15,32].
If the athlete has no underlying illness,then the most common treatment for EAMC is stretching[41].In fact,moderate stretching of the affected muscle has proven to be effective for muscle cramps of all types including those that are heat related[5,7,10,65].Therefore,moderate stretching of the affected muscle to alleviate the cramp is recommended.Passive stretching increases the tension in a muscle,thereby increasing the Golgi tendon organ’s inhibitory input to the alpha motor neuron[52,53].This will then reduce the activity of alpha motor neurons,making EAMC less likely to occur.Other methods that have been implicated for reducing motor neuron activity,thereby alleviating EAMC include massage,active contraction of the antagonist muscle group,and icing of the affected muscles.Certainly,lowering overall exercise intensity and altering the load on the distressed muscles can be effective as well[38].
Recently,an effort has been devoted to evaluate a method of using food extracts like peppers,ginger,mustard, and cinnamon to resolve EAMC.Such food extracts can activate transient receptor potential channels(TRP channels)that are capable of disrupting hyperexcited motor neurons[66].TRP channels are a group of ion channels located in the mouth, esophagus and stomach that regulate the flow of ions,i.e., charged particles like sodium and potassium,across cell membranes.Recent evidence suggests that oral ingestion of TRP channel agonists like cinnamon,peppers,or mustard may attenuate the intensity and/or duration of muscle cramps,presumably by dampening alpha motor neuron excitability[67,68]. These studies produced muscle cramps by electrical stimulation.Therefore,this preventive approach has yet to be examined in clinical trials where cramps can be more naturally induced by physical exercise.
4.2 Prevention
The pathophysiology causing EAMC is most likely multifactorial and complex.As such,prevention of EAMC will need a multifactorial approach.EAMC that occur in hot conditions seemsto be prevented by maintaining fluid and salt balance.Monitoring an athlete’s body weight is an easy method of ensuring adequate fluid replacement.Both the National Athletic Trainers’Association and the American College of Sports Medicine recommend a volume of fluid that allows for less than a 2%body weight reduction from training or competition[43,61].An athlete who ingests a liter of water or hypotonic sports drink at least 1 hour before competition can be confident that the majority of the fluid,electrolytes,and nutrients would be absorbed and become available in the body when the competition begins. Additionally,fluids should be available and easily accessible throughout practices and competitions.Athletes with high sweat rates and sodium loss or who have a history of EAMC may need to consume supplemental sodium during prolonged activities to maintain salt balance[7]and may need to increase dailydietary salt to 5-10 g·day-1when sweat losses are large[43].This is especially important during the heatacclimatization phase of training.In a case report,Bergeron[15]demonstrated that by calculating sweat sodium losses and replacing them during and after activity,two athletes with previously debilitating EAMC were able tocompete successfully in hot conditions.
As mentioned earlier,an important etiology for EAMC is muscle fatigue.As such,prevention strategy should also focus on proper conditioning of an athlete.To truly simulate race or game conditions,intense endurance training is necessary.As endurance capacity increases,muscle would be less prone to cramp at a given level of intensity.Endurance training may also serve as an effective means of preventing EAMC by expanding plasma volume and the extracellular flu id compartment and delaying neuromuscular fatigue[69,70]. Athletes who are returning to competition after injury are particularly susceptible to EAMC as they are likely to experience early muscle fatigue,to be less acclimatized to a hot environment,and to have diminished sweating capacity[71].Proper progression during rehabilitation will prevent overstressing the athlete while ensuring adequate sport specific conditioning before the return to competition.
Prevention exercises that target muscle spindle and Golgi tendon organs should also be implemented to delay the onset of neuromuscular fatigue and,hence,EAMC.Plyometrics may be such exercise to be considered.The explosive nature of this exercise can train neuromuscular units to operate more effectively with increasing levels of intensity.It has been reported that plyometric training can improve the efficiency ofneuromuscular control by muscle spindles and Golgi tendon organs,thereby making them more resistant to fatigue[72,73].
Other preventive measures that have been taken include 1)correctingtechnique errors,muscle imbalance,and/or posture,2)stretching muscle regularly,3)having adequate warm up,4)applying massage therapy before and during competition,5)wearingcompression garments,5)becoming heat acclimatized,and 6)optimizing footwear and/or orthotics.These preventive measures,however,are not evidence-based.
Considering the above discussion,here are some recommendations that can be followed to prevent the occurrence of EAMC:
*Train at race-intensity or,conversely,race according to the level of ability that was attained in training.
*Know your training and competition conditions andfactor in humidity,temperature,indoor versus outdoor,altitude and terrain,and how they might be different than your usual training conditions.
*If you've cramped in the past,think about all factors that could have played a role,i.e.,drastic change in intensity, volume,altitude,terrain,so you can plan your training and competition accordingly.
*Learn to recognize early warning signs of EAMC and respond accordingly.
*Muscles most affected by cramping are those repetitively used and confined to a small arc of motion,so focus on form in training to avoid heavy"braking"and try to stretch out the stride with adequate hip and knee flexion and extension.
*If you’re a“salty sweater,”be sure to increase salt intake in your diet and take in fluids higher in sodium content, especially in the hotter,more humid months.
*Salt tabs or pills are an easy method,but practice using them in training as they can cause upset stomach in some individuals.
*Have adequate nutritional intake,particularly carbohydrates,to prevent premature muscle fatigue during exercise.
*Consider plyometric training of key muscle groups.
*Along with regular stretching,consider corollary activities like flexing opposing muscles and massaging cramped or cramp-prone muscles.
5 总结
尽管EAMC具有高发病率,但是关于其原因、治疗和预防的实验数据很少。EAMC长期以来的解释是依靠电解质紊乱和脱水学说。然而,其支持性证据主要来自观察记录和病例报告。此外,该学说没有阐明合理的病理生理机制,并且据报道,EAMC可以在没有电解质耗竭或脱水的情况下发生。最新的证据表明,EAMC可能由于肌肉疲劳使神经肌肉控制改变而产生。支持这种“异常神经肌肉控制学说”的证据源于实验室研究,这些研究使用了肌电图来监测对肌肉疲劳和痉挛进行应答的脊髓反射活动。虽然有待于进一步证实,但肌肉疲劳和神经肌肉控制的改变似乎对关于这一复杂病症的原因、治疗和预防中未知问题提供更加合理的解释。EAMC的治疗和预防存在许多策略,但其中大多数是观察记录或不受实验研究支持。未来需要能够提供高水平证据的研究来证实EAMC的病因学、治疗方案和预防策略。
5 Overall Summary
Despite the high prevalence of EAMC,few experimental data exist on their cause,treatment,and prevention.EAMC has long been explained by the electrolyte imbalance and dehydration theory.However,its supporting evidence comes mainly from anecdotal observations and casereports.In addition,the theory does not offer plausible pathophysiological mechanisms and it has been reported that EAMC can occur without electrolyte depletion or dehydration.More recent evidence suggests that EAMC may be mediated by muscle fatigue that altered neuromuscular control.The evidence thatsupport this “altered neuromuscular control”theory stems from the laboratory-based experiments that used EMG to monitor spinal reflex activities in response to muscle fatigue and cramping.Although a definitive proof is still needed, muscle fatigue and altered neuromuscular control seem more plausible in explaining many of the unanswered questions with regard to cause,treatment and prevention of this complex condition.There are numerous strategies existed for the treatment and prevention of EAMC.However,most of them are anecdotal and unsupported by experimental research.Research that provide high levels of evidence is needed to substantiate the etiology,treatment options,and prevention strategies of EAMC.
[1]Kantarowski P.G.,Hiller W.D.,Garrett W.E.Cramping studies in 2600 endurance athletes[J].Med.Sci.Sports Exerc.,1990, 22(2):s104.
[2]Schwellnus M.P.,Drew N.,Collins M.Muscle cramping in athletes-risk factors,clinical assessment and management[J].Clin. Sports Med.,2008(1):183-194.
[3]Parisi L.,Pierelli F.,Amabile G.,et al.Muscular cramps:proposals for a new classification[J].Acta.Neurol Scand.2003, 107:176-186.
[4]Schwellnus M.P.,Derman E.W.,Noakes T.D.Aetiology of skeletal muscle“cramps”during exercise:a novel hypothesis[J]. Sports Sci.,1997,15:277-285.
[5]Maquirriain J.,Merello M.The athlete with muscular cramps: clinical approach[J].Am.Acad.Orthop.Surg.,2007,15:425-431.
[6]Miller T.,Layzer R.B.Muscle cramps[J].Muscle Nerve,2005, 32:431-442.
[7]Bergeron M.Exertional heat cramps.In:Exertional heat illnesses[J].Human Kinstics,2003:91-102.
[8]Ladell W.S.S.Heat cramps[J].Lancet,1949,2:836-839.
[9]Dickhuth H.,Rocker K.,Niess A.,et al.Exercise induced,persistent and generalized muscle cramps[J].Sports Med.Phys.Fitness,2002,42:92-94.
[10]Schwellnus M.Cause of exercise associated muscle cramps(eamc) -altered neuromuscular control,dehydration or electrolyte depletion[J].Br.J.Sports Med.,2009,43:401-408.
[11]Brubaker D.,Whitesel J.,Barth B.Quinine sulfate:a treatment for recurrent muscle spasms[J].Athl.Train(Greenville,NC), 1985,20:121-123.
[12]Moss K.Some effects of high air temperatures and muscular exertion upon colliers[J].Proc.R.Soc.Lond.Biol.Sci,1923, 95:181-200.
[13]Maughan R.J.Exercise induced muscle cramp:a prospective biochemical study in marathon runners[J].Sports Sci.,1986,4: 31-34.
[14]Schwellnus M.,Nicol J.,Laubscher R.,et al.Serum electrolyte concentrations and hydration status are not associated with exercise associated muscle cramping(EAMC)in distance runners [J].Br.J.Sports Med.,2004,38:488-492.
[15]Bergeron M.F.Heat cramps during tennis:a case report[J].Int. J.Sport Nutr.,1996,6:62-68.
[16]Manjra S.I.,Schwellnus M.P.,Noakes T.D.Risk factors for exercise associated muscle cramping(EAMC)in marathon runners[J].Med.Sci.Sports Exerc.,1996,28(5):S167.
[17]Drew N.Exercise-associated muscle cramping(EAMC)in Ironman triathletes[D].Cape Town:University of Cape Town,2006. [18]Schwellnus M.P.Muscle cramping in the marathon:etiology and risk factors[J].Sports Med.,2007,37:364-367.
[19]Edsall D.L.New disorder from heat:A disorder due to exposure to intense heat[J].Journal of the American Medical Association,1908,11:1969-1971.
[20]Swanik C.,Lephart S.,Stone D.,et al.The effects of shoulder plyometric training on proprioception and muscle performance characteristics[J].Shoulder Elbow Surg.,2002,11:579-586.
[21]Cooper E.,Ferrara M.,Broglio S.Exertional heat illness and environmental conditions during a single football season in the Southeast[J].Athl.Train,2006,41:332-336.
[22]Galloway S.Dehydration,rehydration,and exercise in the heat: rehydration strategies for athletic competition[J].Can.J.Appl. Physiol.,1999,24:188-200.
[23]Rehrer N.,Smets A.,Reynaert H.,et al.Effect of exercise on portal vein blood flow in man[J].Med.Sci.Sports Exerc.,2001, 31:701-715.
[24]Armstrong L.E.,Maresh C.M.The exertional heat illness:a risk of athletic participation[J].Med.Exerc.Nutr.Health,1993, 2:125-134.
[25]Bergeron M.Heat cramps:fluid and electrolyte challenges during tennis in the heat[J].Sci.Med.Sport,2003,6:19-27.
[26]Stofan J.,Zachwieja J.,Horswill C.,et al.Sweat and sodium losses in NCAA football players:a precursor to heat cramps[J]. Int.J.Sport Nutr.Exerc.Metab.,2005,15:641-652.
[27]McCance R.A.Proceedings of the Royal Society of London. Series B-Biological Sciences,Volume 119,1935-1936:Experimental sodium chloride deficiency in man[J].Nutr.Rev.,1990, 48:145-147.
[28]Levin S.Investigating the cause of muscle cramps[J].Phys. Sportsmed,1993,21:111-113.
[29]Liu L.,Borowski G.,Rose L.I.Hypomagnesemia in a tennis player[J].Phys.Sportsmed,1983,11:79-80.
[30]Miles M.P.,Clarkson P.M.Exercise-induced muscle pain, soreness,and cramps.[J].Sports Med.Phys.Fitness,1994,34: 203-216.
[31]StamfordB.Musclecramps:untyingtheknots[J].Phys.Sportsmed, 1993,21:115-116.
[32]Eichner E.R.The role of sodium in“heat cramping”[J].Sports Med.,2007,37:368-370.
[33]Inoue Y.,Havenith G.,Kenney W.L.,et al.Exercise-and methylcholine-induced sweating responses in older and younger men: effect of heat acclimation and aerobic fitness[J].Int.J.Biometeorol.,1999,42:210-216.
[34]Shirreffs S.M.,Maughan R.J.Volume repletion after exerciseinduced volume depletion in humans:replacement of water and sodium losses[J].Am.J.Physiol.,1998,274:F868-F875.
[35]Costill D.L.,Cote R.,Fink W.Muscle water and electrolytes following varied levels of dehydration in man[J].Appl.Physiol.,1976,40:6-11.
[36]Nose H.,Mack G.W.,Shi X.R.,et al.Shift in body fluid compartments after dehydration in humans[J].Appl.Physiol.,1988; 65:318-324.
[37]Sanders B.,Noakes T.D.,Dennis S.C.Water and electrolyte shifts with partial fluid replacement during exercise[J].Eur.J. Appl.Physiol.,1999,80:318-323.
[38]Bergeron M.Muscle cramps during exercise:is it fatigue or electrolyte deficit[J].Curr.Sports Med.Rep.,2008,7:S50-S55.
[39]Minetto M.A.,Holobar A.,Botter A.,et al.Origin and development of muscle cramps[J].Exerc.Sport Sci.Rev.,2013,41: 3-10.
[40]Layzer R.B.The origin of muscle fasciculations and cramps[J]. Muscle Nerve,1994,17:1243-1249.
[41]Ruff R.L.Effects of length changes on Na+current amplitude and excitability near and far from the end-plate[J].Muscle Nerve, 1996,19:1084-1092.
[42]Sjogaard G.,Adams R.P.,Saltin B.Water and ion shifts in skeletal muscle of humans with intense dynamic knee extension [J].Am.J.Physiol.,1985,248:R190-R196.
[43]Armstrong L.E.,Casa D.J.,Millard-Stafford M.,et al.Exertional Heat Illness during Training and Competition[J].Med. Sci.Sports Exerc.,2007,39:556-572.
[44]Stone M.,Edwards J.,Stemmans C.,et al.Certified athletic trainers’perceptions of exercise associated muscle cramps[J]. Sport Rehabil.,2003,12:333-342.
[45]Eichner E.Heat cramps:salt is simplest,most effective antidote [J].Sports Med.Dig.,1999,21:88.
[46]Eichner E.R.Treatment of suspected heat illness[J].Int.J.Sports Med.,1998,19:S150-S153.
[47]Meira F.S.,Poli de Figueiredo C.E.,Figueiredo A.E.Influence of sodium profile in preventing complications during hemodialysis[J].Hemodial Int.,2007,3:S29-S32.
[48]Jones B.H.,Rock P.B.,Smith L.S.,et al.Medical complaints after a marathon run in cool weather[J].Phys Sportsmed.,1985, 13:103-110.
[49]Bergeron M.Exertional heat cramps:recovery and return to play [J].Sport Rehabil.,2007,16:190-196.
[50]Laird R.H.Medical care at ultra-endurance triathlons[J].Med. Sci.Sports Exerc.,1989,21:S222-S225.
[51]Hutton R.S.,Nelson L.D.Stretch sensitivity of Golgi tendon organs in fatigued gastrocnemius muscle[J].Med.Sci.Sports Exerc.,1986,18:69-74.
[52]Nelson L.D.,Hutton R.S.Dynamic and static stretch response in muscle spindle receptors in fatigued muscle[J].Med.Sci. Sports Exerc.,1985,17:445-450.
[53]Khan S.,Burne J.Reflex inhibition of normal cramp following electrical stimulation of the muscle tendon[J].Neurophysiol., 2007,98:1102-1107.
[54]Bentley S.Exercise-induced muscle cramp.Proposed mechanisms and management[J].Sports Med.,1996,21:409-420.
[55]Jung A.P.,Bishop P.A.,Al-Nawwas A.,et al.Influence of Hydration and Electrolyte Supplementation on Incidence and Time to Onset of Exercise-Associated Muscle Cramps[J].Athl.Train, 2005,40:71-75.
[56]Eaton J.M.Is this really a muscle cramp[J].Postgrad Med., 1989,86:227-232.
[57]Helin P.Physiotherapy and electromyography in muscle cramp [J].Br.J.Sports Med.,1985,19:230-231.
[58]Sontag S.J.,Wanner J.N.The cause of leg cramps and knee pains:a hypothesis and effective treatment[J].Med.Hypotheses, 1988,25:35-41.
[59]Howe A.S.,Boden B.P.Heat-related illness in athletes[J].Am. J.Sports Med.,2007,35:1384-1395.
[60]Talbot H.T.Heat cramps[J].Medicine,1935,14:323-376.
[61]Binkley H.,Beckett J.,Casa D.,et al.National Athletic Trainers’Association position statement:exertional heat illnesses[J]. Athl.Train,2002,37:329-343.
[62]Vriens,Joris,Bernd N.,et al.Herbal Compounds and Toxins Modulating TRP Channels[J].Cur.Neuropharmacology,2008, 6:79-96.
[63]El-Tawil S.,Musa A.,Valli H.,et al.Quinine for muscle cramps [J].Cochrane Database Syst.Rev.,2010,8:CD005044.
[64]Blyton F.,Chuter V.,Burns J.Unknotting night-time muscle cramp:a survey of patient experience,help-seeking behaviour and perceived treatment effectiveness[J].Foot Ankle Res.,2012, 5:7.
[65]Daniel H.Simple cure for nocturnal leg cramps[J].N.Eng.J. Med.,1979,301:216.
[66]Vist G.,Maughan R.The effect of osmolality and carbohydrate content on the rate of gastric emptying of liquids in man[J].J. Physiol.,1995,486:523-531.
[67]Craighead D.H.,Shank S.W.,Alexander L.M.,et al.Orally ingested transient receptor potential(trp)channel activators attenuatetheintensity-durationofvoluntarilyinducedmusclecramps in humans[J].The FASEB Journal,2016,30:lb706.
[68]Short G.F.,Hegarty B.W.,Westphal C.H.,et al.Orally-administered TRPV1 and TRPA1 activators inhibit electrically-induced muscle cramps in normal healthy volunteers[J].Neurology 2015,84(14):S17.003.
[69]Convertino V.Blood volume:its adaptation to endurance training[J].Med.Sci.Sports Exerc.,1991,23:1338-1348.
[70]Hakkinen K.,Komi P.Fatigability in voluntary and reflex contraction after conditioning of human skeletal muscle[J].Electromyogr Clin.Neurophysiol,1985,25:319-330.
[71]Jung A.P.Exercise-associated muscle cramps and functional return to sport[J].Athl.Ther.Today,2006,11:48-50.
[72]Chimera N.,Swanik K.,Swanik C.,et al.Effects of plyometric training on muscle activation strategies and performance in female athletes[J].Athl.Train,2004,39:24-31.
[73]Sulzer N.U.,Schwellnus M.P.,Noakes T.D.Serum electrolytes in Ironman triathletes with exercise-associated muscle cramping [J].Med.Sci.Sports Exerc.,2005,37:1081-1085.
(责任编辑:何聪)
Exercise Associated Muscle Cramps-A Current Perspective
KANG Jie1,ZHANG Peng2
(1.Human Performance Laboratory,Department of Health and Exercise Science,The College of New Jersey, USA;2.Shanghai Research Institute of Sports Science,Shanghai 200030,China)
Exercise-associated muscle cramps (EAMC)are a common condition experienced by recreational and competitive athletes and often require medical attention during or immediately after sports events.Despite the high prevalence of this condition,the etiology of EAMC remains poorly understood and there is a lack of high levels of evidence to guide the management of this condition.The previous claim as to how EAMC come about is being challenged by more recent evidence suggesting a distinctive mechanism.The purpose of this article is to examine the existing scientific evidence in support of various views on the etiology of EAMC and to highlight the most current understanding of this complex condition.Various strategies adopted to treat and prevent EAMC are also discussed even though most of them remain anecdotal and have yet to be substantiated by research experimentation.
EAMC;mechanism;risk factors;treatment;prevention
G804.5
A
1006-1207(2017)01-0001-13
2017-02-11
康杰,博士,美国运动医学院院士。主要研究方向:运动人体科学。E-mail:kang@tcnj.edu。
1.美国新泽西尤英新泽西学院,健康和运动科学系;2.上海体育科学研究所,上海 200030。
