血清PCT、CRP和白细胞计数对胎膜早破并发绒毛膜羊膜炎的预后评估
2017-05-03黄水萍潘志坚宁儒凤陆富华
黄水萍,潘志坚,宁儒凤,陆富华,林 源,方 琳
(广西钦州市妇幼保健院,广西 钦州,535099)
血清PCT、CRP和白细胞计数对胎膜早破并发绒毛膜羊膜炎的预后评估
黄水萍,潘志坚,宁儒凤,陆富华,林 源,方 琳
(广西钦州市妇幼保健院,广西 钦州,535099)
目的 检测胎膜早破并发绒毛膜羊膜炎孕妇降钙素原(PCT)、C-反应蛋白(CRP)和白细胞计数水平,为其早期诊断及预后评估提供科学依据。方法 选择2014年1月至2015年12月在广西钦州市妇幼保健院治疗的胎膜早破患者100例,其中并发绒毛膜羊膜炎57例,为研究组,43例无并发绒毛膜羊膜炎,为对照组。检测各组PCT、CRP和白细胞计数,评估敏感度和特异度,并进行Logistic回归分析。结果 研究组患者血清PCT、CRP和白细胞计数检测结果分别为(11.46±1.13)ng/mL、(13.61±1.08)mg/L和(11.48±1.83)×109/L,均高于对照组的(4.25±0.78)ng/mL、(6.42±0.91)mg/L和(7.65±1.40)×109/L,差异有统计学意义(t值分别为9.89、10.17、9.74,均P<0.05);患者血清PCT、CRP的敏感度和特异度分别为89.47%、88.37%和82.46%、79.09%,均高于白细胞计数的59.65%、67.44%,差异有统计学意义(χ2值分别为8.78、8.93、8.82、9.11,均P<0.05),且PCT的特异度高于CRP,差异有统计学意义(χ2=8.05,P<0.05);研究组患者治疗后血清PCT、CRP和白细胞计数检测结果分别为(6.58±1.06)ng/mL、(6.90±0.97)mg/L和(7.11±1.24)×109/L,均低于治疗前,差异有统计学意义(t值分别为9.31、9.60、9.22、均P<0.05)。结论 胎膜早破并发绒毛膜羊膜炎患者血清PCT、CRP和白细胞计数均显著升高,血清PCT、CRP敏感度和特异度均高于白细胞计数,有助于胎膜早破并发绒毛膜羊膜炎患者的早期诊断和预后评估。
胎膜早破;绒毛膜羊膜炎;降钙素原;C-反应蛋白;白细胞计数
胎膜早破(premature rupture of membrane,PROM)是指产妇临产前发生胎膜破裂,是产科常见的分娩并发症之一。绒毛膜羊膜炎是产妇围产期的一种急性炎症性反应,主要因羊水、胎膜、胎盘等受病原菌感染所导致,也是胎膜早破的重要并发症,给母婴结局带来严重的不良后果[1-2]。早期对胎膜早破并发绒毛膜羊膜炎患者进行诊断感染阳性率较低,误诊率高,因此,寻找早期宫内感染的诊断方法具有重要的临床意义。本研究检测胎膜早破并发绒毛膜羊膜炎孕妇降钙素原(procalcitonin,PCT)、C-反应蛋白(C-reactive protein,CRP)和白细胞计数水平,为其早期诊断及预后评估提供科学依据。
1资料与方法
1.1一般资料
选择2014年1月至2015年12月在广西钦州市妇幼保健院治疗的胎膜早破患者100例,年龄20~39岁,平均年龄(27.59±4.36)岁,平均孕周(34.85±2.36)周。分娩后取2cm×2cm胎盘及一小段脐带进行病理学诊断证实。其中并发绒毛膜羊膜炎患者57例,为研究组,平均年龄(27.51±4.42)岁,平均孕周(34.80±2.31)周。其余43例无并发绒毛膜羊膜炎,为对照组,平均年龄(27.60±4.28)岁,平均孕周(34.92±2.43)周。两组患者年龄、孕周比较,差异均无统计学意义(P>0.05)。排除病例:妊娠期糖尿病、子痫、全身感染患者。
1.2方法和指标
两组孕妇均于发生胎膜早破时(28~37周)入院后4h内采集患者外周静脉血5mL,采用化学发光免疫夹心法定量测定血清中的PCT,应用免疫比浊法定量测定患儿血清CRP水平,并进行白细胞计数,均严格按照试剂盒上的操作方法进行检测。以PCT≥0.5ng/mL为检测结果阳性,CRP≥10mg/L为阳性,白细胞计数≥10×109/L为阳性,评估其敏感度和特异度。特异度=真阴性人数/(真阴性人数+假阳性人数)×100%。
胎膜早破的治疗:胎膜早破发生后,患者卧床休息,保持外阴清洁,积极采取措施防治并发症。早产胎膜早破或足月胎膜早破超过12h者,应给予抗生素以预防感染。胎膜早破发生在28~35孕周,延长孕龄、促进肺成熟,一旦胎肺成熟,应尽早终止妊娠。胎膜早破发生在孕36周以后,应尽快终止妊娠,破膜后12~24h仍不临产者应予以引产。
研究组患者经治疗分娩一天后采集患者外周静脉血5mL,进行检测,以评估患者预后状况。
1.3统计学方法

2结果
2.1两组患者血清PCT、CRP和白细胞计数检测结果比较
研究组患者血清PCT、CRP和白细胞计数检测结果均高于对照组,差异有统计学意义(t值分别为9.89、10.17、9.74,均P<0.05),见表1。

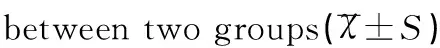
分组例数(n)PCT(ng/mL)CRP(mg/L)白细胞计数(×109/L)对照组434.25±0.786.42±0.917.65±1.40研究组5711.46±1.1313.61±1.0811.48±1.83t9.8910.179.74P0.0190.0130.021
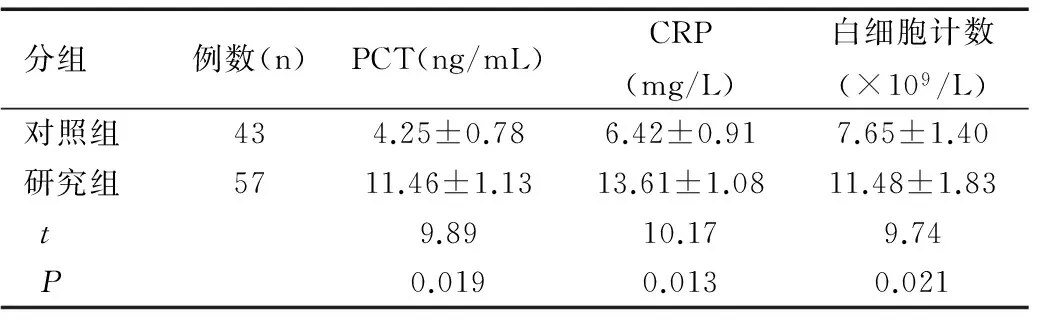
2.2血清PCT、CRP和白细胞计数敏感度及特异度比较
患者血清PCT、CRP的敏感度和特异度分别为89.47%、88.37%和82.46%、79.09%,均高于白细胞计数的59.65%、67.44%,差异有统计学意义(χ2值分别为8.78、8.93、8.82、9.11,均P<0.05),且PCT的特异度高于CRP,差异有统计学意义(χ2=8.05,P<0.05),见表2。
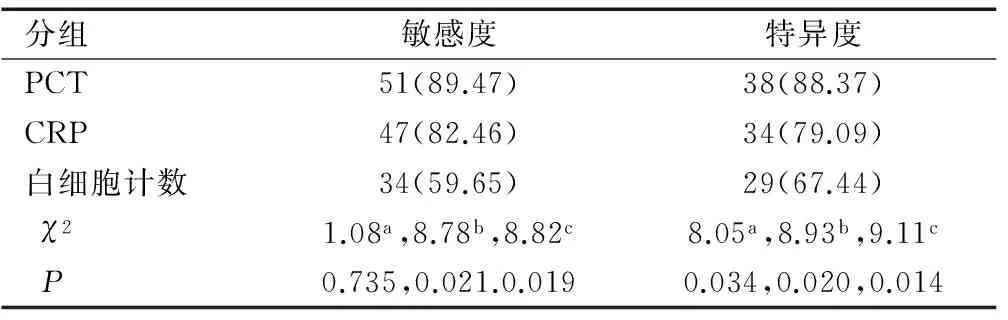
2.3并发绒毛膜羊膜炎患者治疗前后血清PCT、CRP和白细胞计数检测结果比较
研究组患者治疗后血清PCT、CRP和白细胞计数检测结果均低于治疗前,差异有统计学意义(t值分别为9.31、9.60、9.22,均P<0.05),见表3。
表2 血清PCT、CRP和白细胞计数敏感度和特异度结果比较[n(%)]
Table 2 Comparison of sensitivity and specificity of serum PCT, CRP and WBC[n(%)]
注:a为PCT与CRP比较,b为PCT与白细胞计数比较,c为CRP与白细胞计数比较。


分组例数(n)PCT(ng/mL)CRP(mg/L)白细胞计数(×109/L)治疗前5711.46±1.1313.61±1.0811.48±1.83治疗后576.58±1.066.90±0.977.11±1.24t9.319.609.22P0.0220.0140.026
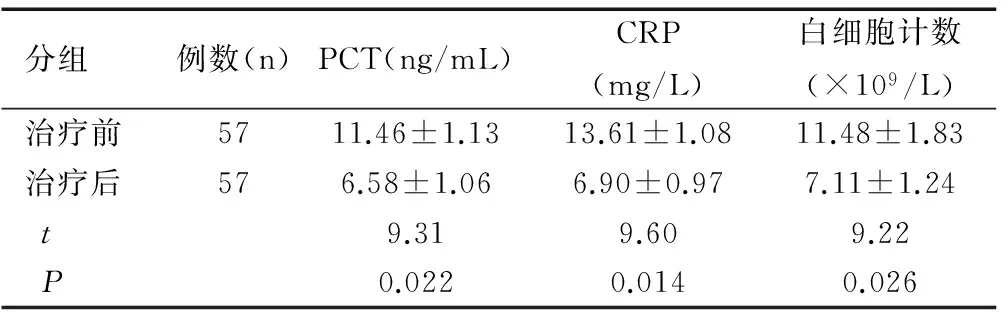
2.4两组患者血清PCT、CRP和白细胞计数与并发绒毛膜羊膜炎的Logistic分析
多因素Logistic回归分析中,将血清PCT、CRP和白细胞计数作为自变量,并分别赋值,并发绒毛膜羊膜炎为因变量,进行Logistic分析,结果显示,并发绒毛膜羊膜炎与血清PCT、CRP和白细胞计数均相关,差异均具有统计学意义(均P<0.05),见表4。
表4 两组患者血清PCT、CRP和白细胞计数与并发绒毛膜羊膜炎的Logistic分析
Table 4 Logistic analysis of serum PCT, CRP and WBC in two groups with concurrent chorioamnionitis

3讨论
3.1胎膜早破并发绒毛膜羊膜炎对母婴危害
胎膜早破是产科常见的分娩并发症,胎膜破裂后,羊膜腔与外界相通,病原菌可直接经阴道、宫颈口上行进入羊膜腔,使绒毛膜羊膜炎发生的几率增加。胎膜早破并发绒毛膜羊膜炎早期,大多数孕妇无临床症状,出现临床症状时,可给孕产妇和新生儿造成严重并发症,严重威胁母婴安全。早期进行诊断,及时发现胎膜早破并发绒毛膜羊膜炎进行治疗,减少新生儿的宫内感染率,改善母婴预后[3]。
3.2血清PCT、CRP在胎膜早破并发绒毛膜羊膜炎中的意义
本次研究结果显示,研究组患者血清PCT、CRP和白细胞计数检测结果均高于对照组,差异有统计学意义(P<0.05),PCT、CRP和白细胞计数能够鉴别感染性与非感染性疾病,对胎膜早破并发绒毛膜羊膜炎患者进行诊断。CRP是一种由肝脏产生的急性时相反应蛋白,正常情况下CRP 在血液中的含量非常少,机体受到感染或组织损伤能释放入血,在血清中迅速升高[4-5]。PCT属于无激素活性的降钙素前肽物质,生理情况下极少量的PCT由甲状腺 C 细胞产生,机体受到细菌等感染后,外周血的单核细胞、巨噬细胞等大量释放PCT,同时各种炎性因子也刺激肝脏合成、分泌大量PCT释放入血。胎膜破裂后,导致羊膜腔与外界相通,增加绒毛膜羊膜炎发生几率,血清PCT、CRP显著升高,和白细胞 计数相比,显示出较好的优势[6-7]。其中PCT 在4h其浓度即可增加,6~8h达到高峰,其临床半衰期为24~30h,对于细菌感染具有较高的高灵敏度和特异性。在早期更有助于对胎膜早破并发绒毛膜羊膜炎患者进行诊断和评估[8-9]。PCR在机体发生细菌感染或损伤后6~12h开始升高,24~48h逐渐达到高峰,反映机体感染状况具有较高的敏感性。但CRP易受其他部位炎症的影响,特异性有一定局限性[10-11]。白细胞计数易受到其他因素影响,敏感度和特异度均受到一定限制,在早期较难准确反映合并羊膜腔感染,难以及时预测感染的存在。本次研究结果也证实患者血清PCT、CRP的敏感度和特异度均高于白细胞计数,且PCT的特异度高于CRP,经过抗感染治疗后,随着炎症的消退,PCT、CRP和白细胞计数逐渐降低恢复,可作为并发绒毛膜羊膜炎及预后的评估指标。
综上所述,胎膜早破并发绒毛膜羊膜炎患者血清PCT、CRP和白细胞计数均显著升高,血清PCT、CRP敏感度和特异度均高于白细胞计数,有助于胎膜早破并发绒毛膜羊膜炎患者的早期诊断和预后评估。
[1]柯玮琳,赵卫华,王欣昱.足月胎膜早破与母儿感染的临床分析[J].中国妇幼健康研究,2013,24(3):351-352,374.
[2]中华医学会妇产科学分会产科学组.胎膜早破的诊断与处理指南(2015)[J].中华妇产科杂志,2015,50(1):3-8.
[3]靳钰,申彩霞,刘晓宁.IL-6、TNF-α、MMP-8与胎膜早破早产及宫内感染的关系[J].中国优生优育,2013,19(3):169-172.
[4]刘雪彩,陈月花,张桂英,等.CRP、IL-6联合检测对胎膜早破绒毛膜羊膜炎的临床价值[J].海南医学院学报,2016,22(2):163-165.
[5]Gulati S, Agrawal S, Raghunandan C,etal. Maternal serum interleukin-6 and its association with clinicopathological infectious morbidity in preterm premature rupture of membranes: a prospective cohort study[J].J Matern Fetal Neonatal Med,2012,25(8):1428-1432.
[6]Vajrychova M, Kacerovsky M, Tambor V,etal. Microbial invasion and histological chorioamnionitis upregulate neutrophil-gelatinase associated lipocalin in preterm prelabor rupture of membranes[J].J Matern Fetal Neonatal Med,2016,29(1):12-21.
[7]Canpolat F E, Yigit S, Korkmaz A,etal.Procalcitonin versus CRP as an early indicator of fetal infection in preterm premature rupture of membranes[J].Turk J Pediatr,2011,53 (2):180-186.
[8]Le Ray I, Mace G , Sediki M ,etal. Changes in maternal blood inflammatory markers as a predictor of chorioamnionitis: a prospective multicenter study[J].Am J Reprod Immunol,2015,73 (1):79-90.
[9]李冉,罗正琴.降钙素原检测在胎膜早破患者中的临床应用价值探讨[J].中国医药科学,2015,5(1):162-164,174.
[10]李娜,董智力.血清CRP对临产后剖宫产产妇早期感染的预测价值[J].中国妇幼健康研究,2015,26(6):1315-1317.
[11]Miyazaki K, Furuhashi M, Ishikawa K,etal. Long-term outcomes of antenatal corticosteroids treatment in very preterm infants after chorioamnionitis[J].Arch Gynecol Obstet,2015,292 (6):1239-1246.
[专业责任编辑: 杨文方]
Prognostic evaluation of premature rupture of membrane complicated with chorioamnionitis with serum PCT, CRP and WBC
HUANG Shui-ping, PAN Zhi-jian,NING Ru-feng, LU Fu-hua, LIN Yuan, FANG Lin
(GuangxiQinzhouMaternalandChildHealthCareHospital,GuangxiQinzhou535099,China)
Objective To detect the levels of procalcitonin (PCT) and C-reactive protein (CRP) and white blood cell count (WBC) of pregnant women with premature rupture of membranes (PROM) complicated with chorioamnionitis and provide scientific basis for early diagnosis and prognostic evaluation. Methods Totally 100 cases of PROM treated in Guangxi Qinzhou Maternal and Child Health Care Hospital were selected from January 2014 to December 2015, of which 57 cases complicated with chorioamnionitis were set in study group and 43 cases without chorioamnionitis in control group. PCT, CRP and WBC of two groups were detected, and sensitivity and specificity were assessed and Logistic regression analysis was conducted. Results The levels of serum PCT and CRP and WBC of the study group were 11.46±1.13ng/mL, 13.61±1.08mg/L and (11.48±1.83)×109/L, respectively, which were higher than those of the control group [4.25±0.78ng/mL, 6.42±0.91mg/L and (7.65±1.40)×109/L]. The differences were statistically significant (tvalue was 9.89, 10.17 and 9.74, respectively, allP<0.05). The sensitivity of serum PCT and CRP was 89.47% and 88.37%, respectively, and the specificity was 82.46% and 79.09%, respectively. They were higher than those of WBC (59.65%, 67.44%) with statistical significance (χ2value was 8.78, 8.93, 8.82 and 9.11, respectively, allP<0.05). The specificity of PCT was higher than CRP, and the difference was statistically significant (χ2=8.05,P<0.05). Serum PCT, CRP and WBC after treatment of the study group were 6.58±1.06ng/mL, 6.90±0.97mg/L and (7.11±1.24)×109/L, respectively, which were lower than those before treatment with significant differences (tvalue was 9.31, 9.60, and 9.22, respectively, allP<0.05). Conclusion Serum PCT, CRP and WBC of PROM patients complicated with chorioamnionitis are significantly elevated. The sensitivity and specificity of serum PCT and CRP are higher than those of WBC, which is helpful for early diagnosis and prognostic evaluation for the patients with PROM complicated with chorioamnionitis.
premature rupture of membrane (PROM); chorioamnionitis; procalcitonin (PCT); C-reactive protein (CRP); white blood cell count (WBC)
2016-06-13
黄水萍(1983-),女,主治医师,主要从事病理产科工作。
潘志坚,主任医师。
10.3969/j.issn.1673-5293.2017.03.030
R714
[文章编号]1673-5293(2017)03-0312-02
