脓毒症患者血清降钙素原的表达及其对预后的影响研究
2017-02-20谭德敏谭孟源蒙振发王御林
谭德敏,谭孟源,陈 军,蒙振发,王御林
·论著·
·专题研究·
脓毒症患者血清降钙素原的表达及其对预后的影响研究
谭德敏*,谭孟源,陈 军,蒙振发,王御林
目的 探讨脓毒症患者血清降钙素原(PCT)水平的变化及其对预后的影响。方法 选取2012年3月—2016年3月在儋州市人民医院重症监护室住院并明确诊断为脓毒症的患者216例,随访28 d,根据预后分为存活组(134例)和死亡组(82例)。另选取同期本院住院非脓毒症患者188例。记录所有患者急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分、序贯器官衰竭评估(SOFA)评分、血清PCT、C反应蛋白(CRP)和脑钠肽(BNP)水平。采用多因素Logistic回归分析影响脓毒症患者预后的因素;分析各影响因素预测脓毒症预后的价值。结果 脓毒症患者APACHEⅡ评分、SOFA评分、血清PCT、CRP、BNP水平均高于非脓毒症患者(P<0.01)。死亡组住院第1、3、5天血清PCT水平以及住院第3、5天血清CRP和BNP水平均高于存活组(P<0.05)。死亡组年龄、APACHEⅡ评分、SOFA评分、天冬氨酸氨基转移酶水平均高于存活组(P<0.05)。多因素Logistic回归分析结果显示,年龄〔OR=7.284,95%CI(3.605,14.727)〕、APACHEⅡ评分〔OR=3.162,95%CI(1.528,10.629)〕、SOFA评分〔OR=3.015,95%CI(1.054,9.582)〕、PCT〔OR=1.046,95%CI(1.002,1.516)〕、CRP〔OR=0.863,95%CI(0.715,0.985)〕及BNP〔OR=0.795,95%CI(0.653,0.952)〕是影响脓毒症患者预后的因素(P<0.05)。年龄、APACHEⅡ评分、SOFA评分、PCT、CRP及BNP预测脓毒症预后的受试者工作特征(ROC)曲线下面积(AUC)及最佳阈值分别为:0.803(63.0岁)、0.826(22.3分)、0.765(7.1分)、0.849(6.9 μg/L)、0.684(49 mg/L)、0.626(825 ng/L)。Pearson相关分析结果显示,脓毒症死亡患者血清PCT水平与年龄、APACHEⅡ评分、SOFA评分、CRP及BNP水平均呈正相关(P<0.05)。结论 脓毒症患者血清PCT水平明显升高,年龄、APACHEⅡ评分、SOFA评分、PCT、CRP及BNP水平升高是影响脓毒症患者预后的独立危险因素。
脓毒症;降钙素原;重症监护病房;危险因素
脓毒症病情凶险,是危重患者常见的死亡原因之一,尽管对脓毒症的发病机制认知及诊断水平不断提高,其病死率仍居高不下,目前已成为重症监护室面临的一大难题[1-2]。近年来,用于评估脓毒症病情及判断预后的特异性指标是危重医学领域的研究热点[3-4]。降钙素原(procalcitonin,PCT)是降钙素的前体物质,一般机体受到细菌感染时,血清PCT水平显著升高,是反映感染程度的重要生物学指标,在脓毒症的早期诊断及预后评估中具有重要价值[5-6]。本研究通过检测216例ICU脓毒症患者血清PCT水平的变化,并分析脓毒症患者死亡的危险因素,以期为早期认识、诊断和治疗严重脓毒症提供依据。
1 对象与方法
1.1 研究对象 选取2012年3月—2016年3月在儋州市人民医院重症监护室住院并明确诊断为脓毒症的患者216例,其中男120例,女96例;年龄18~87岁,平均年龄(62.8±10.9)岁。脓毒症的诊断参照《2012国际严重脓毒症及脓毒性休克诊疗指南》[7]中的诊断标准。排除标准:血液系统疾病或接受抗凝治疗者,有肝肾衰竭、肺部疾病、癌症晚期及家属放弃治疗者。另选取同期本院住院非脓毒症患者188例,其中男107例,女81例;年龄22~85岁,平均年龄(62.7±11.2)岁。本研究符合医学伦理学标准,经本院伦理委员会批准,并获得患者或家属知情同意。
1.2 分组方法 采用巢式病例对照研究方法,根据216例脓毒症患者随访28 d的生存情况,按照转出ICU或出院时病情转归情况分为存活组和死亡组。其中存活组134例,男76例、女58例,年龄18~84岁,平均年龄(60.3±11.4)岁;死亡组82例,其中男44例、女38例,年龄35~87岁,平均年龄(68.6±13.6)岁。记录患者入院当天的体质指数(BMI)、基础疾病(糖尿病、冠心病、高血压等)、急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分、序贯器官衰竭评估(SOFA)评分、感染部位等基本资料。
1.3 检测指标 分别检测患者住院第1、3、5天时血清PCT、C反应蛋白(CRP)及脑钠肽(BNP)水平。使用全自动多功能酶标仪(美国Thermo公司)酶联免疫吸附法检测PCT,试剂盒为美国Rapidbio公司产品;PCT最小检测浓度为0.05 μg/L。使用Triage型诊断仪和呼吸困难测试板(美国Biosite公司)双抗夹心免疫荧光法检测BNP,BNP的分析范围为5~5 000 ng/L。罗氏全自动生化分析仪及配套试剂盒检测血清CRP、血糖(GLU)、丙氨酸氨基转移酶(ALT)、天冬氨酸氨基转移酶(AST)和总胆红素(Tbil),CRP的参考范围为0~8 mg/L。以上操作均严格按照试剂盒说明书进行。
2 结果
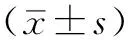
2.1 非脓毒症患者和脓毒症患者临床指标比较 脓毒症患者和非脓毒症患者性别、年龄、BMI、糖尿病、冠心病及高血压患病率比较,差异均无统计学意义(P>0.05)。脓毒症患者APACHEⅡ评分、SOFA评分、血清PCT、CRP、BNP水平均高于非脓毒症患者,差异有统计学意义(P<0.01,见表1)。
2.2 存活组和死亡组住院第1、3、5天血清PCT、CRP及BNP水平比较 PCT、CRP、BNP水平预后与时间存在交互作用(P<0.05);预后主效应显著(P<0.05);时间主效应显著(P<0.001)。其中存活组和死亡组住院第1天血清CRP、BNP比较,差异均无统计学意义(P>0.05);死亡组住院第1、3、5天血清PCT水平以及住院第3、5天血清CRP和BNP水平均高于存活组,差异有统计学意义(P<0.05,见表2)。
2.3 脓毒症患者死亡危险因素的单因素分析 存活组和死亡组性别、BMI、糖尿病、冠心病、高血压患病率、感染部位、GLU、ALT、Tbil水平比较,差异均无统计学意义(P>0.05)。死亡组年龄、APACHEⅡ评分、SOFA评分、AST水平均高于存活组,差异有统计学意义(P<0.05,见表3)。
2.4 多因素Logistic回归分析 以预后为因变量(赋值:生存=0,死亡=1),以年龄(赋值:<60岁=0,≥60岁=1)、APACHEⅡ评分(赋值:<20分=0,≥20分=1)、SOFA评分(赋值:<7分=0,≥7分=1)、PCT(赋值:<6.5 μg/L=0,≥6.5 μg/L=1)、CRP(赋值:<45 mg/L=0,≥45 mg/L=1)、BNP(赋值:<1 200 ng/L=0,≥1 200 ng/L=1)为自变量进行多因素Logistic回归分析,结果显示,年龄、APACHEⅡ评分、SOFA评分、PCT、CRP及BNP是影响脓毒症患者预后的因素(P<0.05,见表4)。
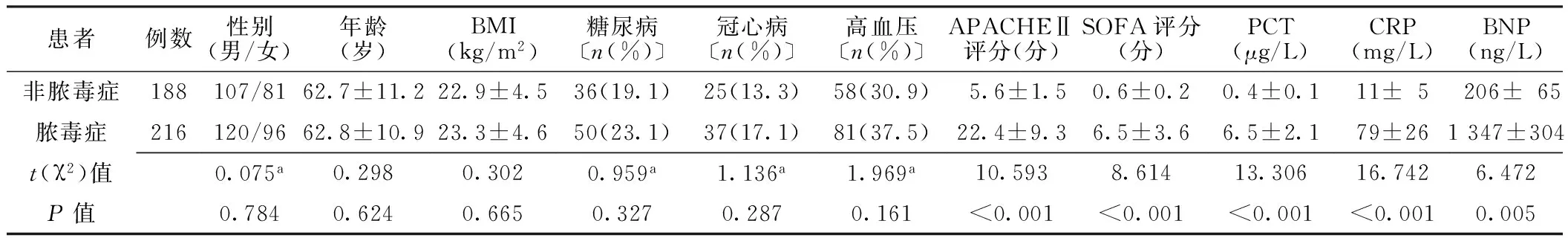
表1 非脓毒症患者和脓毒症患者临床指标比较
注:BMI=体质指数,APACHEⅡ=急性生理学与慢性健康状况评分系统Ⅱ,SOFA=序贯器官衰竭评估,PCT=降钙素原,CRP=C反应蛋白,BNP=脑钠肽;a为χ2值
表2 存活组和死亡组住院第1、3、5天血清PCT、CRP及BNP水平比较
注:与存活组比较,aP<0.05
表3 存活组和死亡组一般资料比较
注:a为t值;GLU=血糖,ALT=丙氨酸氨基转移酶,AST=天冬氨酸氨基转移酶,Tbil=总胆红素
表4 脓毒症患者预后影响因素的多因素Logistic回归分析
Table 4 Multivariate Logistic regression analysis on the influencing factors for prognosis in sepsis patients
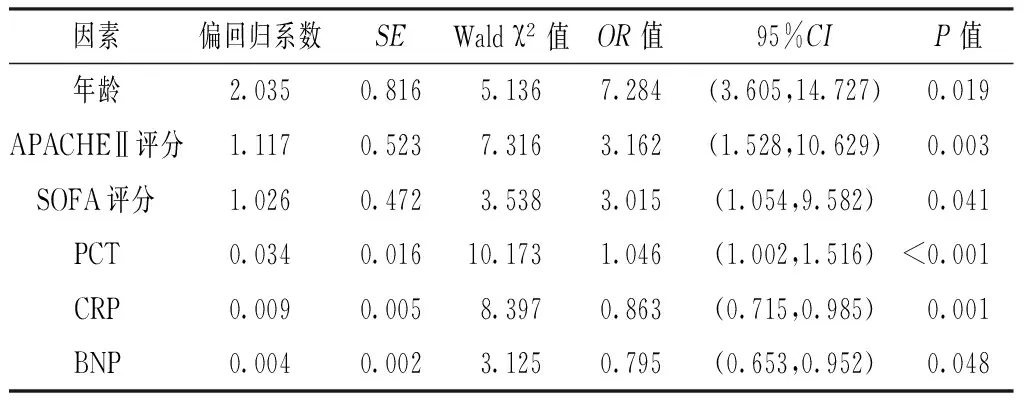
因素偏回归系数SEWaldχ2值OR值95%CIP值年龄2.0350.8165.1367.284(3.605,14.727)0.019APACHEⅡ评分1.1170.5237.3163.162(1.528,10.629)0.003SOFA评分1.0260.4723.5383.015(1.054,9.582)0.041PCT0.0340.01610.1731.046(1.002,1.516)<0.001CRP0.0090.0058.3970.863(0.715,0.985)0.001BNP0.0040.0023.1250.795(0.653,0.952)0.048
2.5 各危险因素预测脓毒症预后效能分析 年龄、APACHEⅡ评分、SOFA评分、PCT、CRP及BNP预测脓毒症预后的AUC分别为:0.803、0.826、0.765、0.849、0.684、0.626。年龄、APACHEⅡ评分、PCT的AUC均>0.800(见表5)。年龄取最佳阈值63.0岁时,灵敏度和特异度分别为84.2%和73.6%;APACHEⅡ评分取最佳阈值22.3分时,灵敏度和特异度分别为76.5%和80.4%;PCT取最佳阈值6.9 μg/L时,灵敏度和特异度分别为86.3%和76.5%(见表6)。
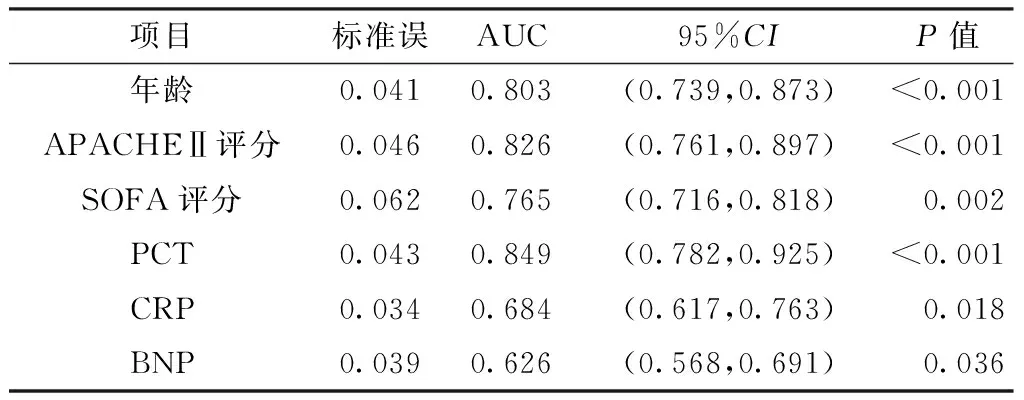
表5 各危险因素预测脓毒症预后的AUC
注:AUC=受试者工作特征曲线下面积
表6 各危险因素预测脓毒症预后的效能
Table 6 Efficacy of risk factors for predicting the prognosis of sepsis patients
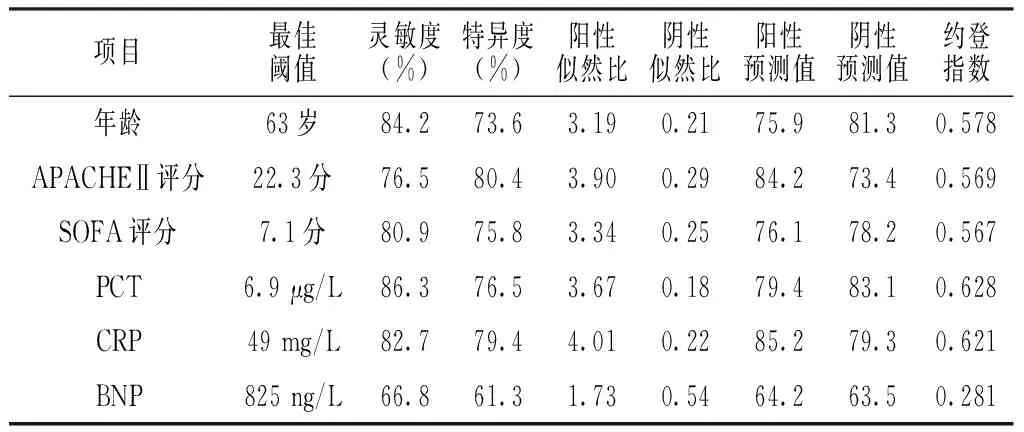
项目最佳阈值灵敏度(%)特异度(%)阳性似然比阴性似然比阳性预测值阴性预测值约登指数年龄63岁84.273.63.190.2175.981.30.578APACHEⅡ评分22.3分76.580.43.900.2984.273.40.569SOFA评分7.1分80.975.83.340.2576.178.20.567PCT6.9μg/L86.376.53.670.1879.483.10.628CRP49mg/L82.779.44.010.2285.279.30.621BNP825ng/L66.861.31.730.5464.263.50.281
2.6 血清PCT水平与各危险因素的相关性分析 Pearson相关分析结果显示,脓毒症死亡患者血清PCT水平与年龄、APACHEⅡ评分、SOFA评分、CRP及BNP水平均呈正相关(r=0.571,P<0.001;r=0.815,P<0.001;r=0.527,P=0.023;r=0.562,P<0.001;r=0.635,P<0.001)。
3 讨论
脓毒症是微生物入侵机体感染后引起机体产生大量的炎性递质而发生的急危重症,其主要特征为在严重感染反应的基础上出现急性循环衰竭,可导致重要脏器代谢障碍,从而发生多器官功能障碍综合征,对患者的生命造成极大威胁。因此,寻找一种脓毒症患者早期诊断指标及病情评估的有效方法,是降低患者病死率的关键。
PCT是降钙素的前肽蛋白,在严重感染、全身炎性反应、脓毒症或多器官功能障碍时PCT水平显著升高,是鉴别细菌感染和病毒感染的良好指标[9]。CRP是一种机体急性期反应蛋白,常用来反映感染的严重程度,已经成为临床上应用广泛的炎性指标[10]。BNP主要应用于心力衰竭、心肌梗死等心血管疾病的预后及危险度的分级,但近来研究发现其可作为评估脓毒症预后的指标[11]。APACHEⅡ评分广泛应用于ICU患者病情评估,对脓毒症和危重症患者有较好的临床评估效果[12]。SOFA评分是一个动态描述脓毒症相关脏器功能障碍的量化评分指标,能较好地评估危重病患者的预后[13]。本研究结果显示,脓毒症患者APACHEⅡ评分、SOFA评分、血清PCT、CRP和BNP水平均明显高于非脓毒症患者。死亡组住院第1、3、5天血清PCT水平均明显高于存活组,住院第3、5天血清CRP及BNP水平均高于存活组。死亡组APACHEⅡ评分、SOFA评分均明显高于存活组。上述结果说明,APACHEⅡ评分、SOFA评分、血清PCT、CRP和BNP水平在脓毒症的诊断及预后评估中具有一定的价值。越来越多的研究表明,APACHEⅡ评分和SOFA评分的变化可更好地评估脓毒症患者的预后,能客观、连续地描述轻度至重度器官衰竭的过程[14-15]。HEGAZY等[16]研究表明,血清PCT和CRP水平的检测不仅可反映脓毒症患者的病情严重程度,也可作为预测脓毒症患者预后的独立危险因素。
本研究在参阅国内外相关指南、文献[17-18]及结合专家意见的基础上对变量进行赋值,应用单因素及多因素Logistic回归分析影响脓毒症患者预后的相关因素,发现年龄、APACHEⅡ评分、SOFA评分、PCT、CRP及BNP水平升高是预测脓毒症预后的独立危险因素。老年患者机体抵抗能力下降,器官功能随着年龄的增长而发生生理性衰退,且常合并多种慢性疾病,一旦发生脓毒症可引起患者器官衰竭,甚至造成死亡。QIAO等[19]研究发现APACHEⅡ评分能较好地评价脓毒症患者的预后,是危重症患者预后的独立危险因素。SOFA评分是反映脓毒症患者病情及预后不良的可靠指标,其分值越高反映脓毒症患者病情越严重[20]。ENGUIX-ARMADA等[21]研究表明,血清PCT和CRP水平变化可有效预测细菌脓毒症患者死亡情况。既往研究表明,BNP水平可能是脓毒症风险分层和预后的一个潜在生物学指标[22]。王胜云等[23]研究显示,PCT水平与APACHEⅡ评分、SOFA评分均有相关性,病情越轻(APACHEⅡ和SOFA评分越低)其水平越低,随着病情加重(APACHEⅡ和SOFA评分升高)其水平显著升高。本研究结果显示血清PCT水平与年龄、APACHEⅡ评分、SOFA评分、CRP及BNP水平均有良好相关性。脓毒症预后危险因素的ROC曲线显示年龄、APACHEⅡ评分及血清PCT的灵敏度和特异度相对较好,AUC均>0.800。PCT的最佳阈值为6.9 μg/L,高于PODDAR等[24]研究结果,这可能与脓毒症的入选标准、研究方法、对病情的判断存在偏差有关。最近一项纳入3 244例患者,包含1 863例脓毒症患者和1 381例非脓毒症者的荟萃分析显示,PCT的灵敏度为0.77〔95%CI(0.72,0.81)〕,特异度为0.79〔95%CI(0.74,0.84)〕,AUC为0.85〔95%CI(0.81,0.88)〕[25]。
综上所述,血清PCT较CRP和BNP能更好地反映脓毒症患者的病情严重程度以及预后评估,结合APACHEⅡ评分、SOFA评分使用,更有助于脓毒症的诊断、预后判断和治疗监测。分析脓毒症的发生及预后危险因素,加强对高危患者的防治,有利于降低脓毒症的病死率。
专家点评:
降钙素原(PCT)是目前脓毒症诊断、评估疗效和预后最为有效的工具之一。目前,学术界已达成共识的是PCT水平的高低和脓毒症的严重程度呈高度正相关,其水平降低可视为感染得到控制和治疗取得效果。已有学者通过连续的PCT水平监测,成功预测了危重症患者90 d的病死率。然而单独使用PCT评估脓毒症患者预后不可避免地会发生失真,当前主流的学术观点更为推荐使用PCT联合其他指标〔如C反应蛋白(CRP)、急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分和序贯器官衰竭评估(SOFA)评分等〕以提高脓毒症预后的预测效能。本研究得到年龄、APACHEⅡ评分、SOFA评分、PCT、CRP及脑钠肽(BNP)水平对脓毒症预后的预测价值,但若能进一步联合评估脓毒症预后或可为临床带来更新的启示。
作者贡献:谭德敏进行文章的构思与设计、结果的分析与解释、撰写论文;陈军进行研究的实施与可行性分析;蒙振发进行数据收集和整理;王御林进行统计学处理;谭孟源进行论文的修订、负责文章的质量控制及审校;谭孟源、陈军对文章整体负责,监督管理。
本文无利益冲突。
[1]REITH S,ORTLEPP J R.State of the art-intensive care therapy of septic patients[J].Dtsch Med Wochenschr,2016,141(15):1082-1090.DOI:10.1055/s-0042-110669.
[2]KLASTRUP V,HVASS A M,MACKENHAUER J,et al.Site of infection and mortality in patients with severe sepsis or septic shock.A cohort study of patients admitted to a Danish general intensive care unit[J].Infect Dis(Lond),2016,48(10):726-731.DOI:10.3109/23744235.2016.1168938.
[3]ROWE T,ARAUJO K L,VAN NESS P H,et al.Outcomes of older adults with sepsis at admission to an intensive care unit[J].Open Forum Infect Dis,2016,3(1):ofw010.DOI:10.1093/ofid/ofw010.
[4]MIGLIETTA F,FANESCHI M L,LOBREGLIO G,et al.Procalcitonin,C-reactive protein and serum lactate dehydrogenase in the diagnosis of bacterial sepsis,SIRS and systemic candidiasis[J].Infez Med,2015,23(3):230-237.DOI:9.3105/26397291.
[5]CHOE E A,SHIN T G,JO I J,et al.The prevalence and clinical significance of low procalcitonin levels among patients with severe sepsis or septic shock in the emergency department[J].Shock,2016,46(1):37-43.DOI:10.1097/SHK.0000000000000566.
[6]JIANG L,FENG B,GAO D,et al.Plasma concentrations of copeptin,C-reactive protein and procalcitonin are positively correlated with APACHE Ⅱ scores in patients with sepsis[J].J Int Med Res,2015,43(2):188-195.DOI:10.1177/0300060514561136.
[7]高戈,冯喆,常志刚,等.2012国际严重脓毒症及脓毒性休克诊疗指南[J].中华危重病急救医学,2013,25(8):501-505.DOI:10.3760/cma.j.issn.2095-4352.2013.08.016. GAO G,FENG Z,CHANG Z G,et al.2012 international guidelines for the diagnosis and treatment of severe sepsis and septic shock[J].Chinese Critical Care Medicine,2013,25(8):501-505.DOI:10.3760/cma.j.issn.2095-4352.2013.08.016.
[8]王先运,吴多文,汲伟明,等.用ROC曲线下面积进行差异性检验的常用方法[J].中华放射学杂志,2006,40(7):763-764.DOI:10.3760/j.issn:1005-1201.2006.07.022. WANG X Y,WU D W,JI W M,et al.The common method of using the area under the ROC curve to test the difference[J].Chinese Journal of Radiology,2006,40(7):763-764.DOI:10.3760/j.issn:1005-1201.2006.07.022.
[9]LIMA L F,MASCHION J M,RODRIGUEZ N A,et al.Procalcitonin for bacterial infection management:a comprehensive understanding may clarify its due value[J].Pediatr Crit Care Med,2016,17(6):581-582.DOI:10.1097/PCC.0000000000000744.
[10]ELLIOTT T S,CASEY A L,KARPANEN T J,et al.Markers to enhance CRP for sepsis diagnosis[J].J Infect,2016,22(16):30173-30176.DOI:10.1016/j.jinf.2016.07.022.
[11]GUARICCI A I,SANTORO F,PAOLETTI PERINI A,et al.Correlations between NT-proBNP,outcome and haemodynamics in patients with septic shock[J].Acta Cardiol,2015,70(5):545-552.DOI:10.2143/AC.70.5.3110515.
[12]CHHANGANI N P,AMANDEEP M,CHOUDHARY S,et al.Role of acute physiology and chronic health evaluation Ⅱ scoring system in determining the severity and prognosis of critically ill patients in pediatric intensive care unit[J].Indian J Crit Care Med,2015,19(8):462-465.DOI:10.4103/0972-5229.162463.
[13]NAIR R,BHANDARY N M,D′SOUZA A D.Initial sequential organ failure assessment score versus simplified acute physiology score to analyze multiple organ dysfunction in infectious diseases in intensive care unit[J].Indian J Crit Care Med,2016,20(4):210-215.DOI:10.4103/0972-5229.180041.
[14]KARTAL E D,KARKAC E,GULBAS Z,et al.Several cytokines and protein C levels with the APACHE Ⅱ scoring system for evaluation of patients with sepsis[J].Balkan Med J,2012,29(2):174-178.DOI:10.5152/balkanmedj.2011.016.
[15]杨旭,刘志.联合应用早期体温峰值及48h-ΔSOFA评分对急诊脓毒症患者预后评估的临床价值[J].中华急诊医学杂志,2016,25(1):68-72.DOI:1006-1302.2016.07.015. YANG X,LIU Z.The clinical value of combining early peak temperature with 48h-Δsequential organ failure assessment score in predicting prognosis for patients with sepsis in emergency department[J].Chinese Journal of Emergency Medicine,2016,25(1):68-72.DOI:1006-1302.2016.07.015.
[16]HEGAZY M A,OMAR A S,SAMIR N,et al.Amalgamation of procalcitonin,C-reactive protein,and sequential organ failure scoring system in predicting sepsis survival[J].Anesth Essays Res,2014,8(3):296-301.DOI:10.4103/0259-1162.143115.
[17]范泉,张泓.脓毒症患者预后危险因素的Logistic回归分析[J].安徽医科大学学报,2014,49(10):1479-1481.DOI:1028-1315.2014.03.012. FAN Q,ZHANG H.Logistic regression analysis of the prognostic factors of patients with sepsis[J].Acta Universitatis Medicinalis Anhui,2014,49(10):1479-1481.DOI:1028-1315.2014.03.012.
[18]YANG Y,XIE J,GUO F,et al.Combination of C-reactive protein,procalcitonin and sepsis-related organ failure score for the diagnosis of sepsis in critical patients[J].Ann Intensive Care,2016,6(1):51.DOI:10.1186/s13613-016-0153-5.
[19]QIAO Q,LU G,LI M,et al.Prediction of outcome in critically ill elderly patients using APACHE Ⅱ and SOFA scores[J].J Int Med Res,2012,40(3):1114-1121.DOI:10.1125/li3615-012-0128-3.
[20]MACDONALD S P,ARENDTS G,FATOVICH D M,et al.Comparison of PIRO,SOFA,and MEDS scores for predicting mortality in emergency department patients with severe sepsis and septic shock[J].Acad Emerg Med,2014,21(11):1257-1263.DOI:10.1111/acem.12515.
[21]ENGUIX-ARMADA A,ESCOBAR-CONESA R,GARCA-DE LA TORRE A,et al.Usefulness of several biomarkers in the management of septic patients:C-reactive protein,procalcitonin,presepsin and mid-regional pro-adrenomedullin[J].Clin Chem Lab Med,2016,54(1):163-168.DOI:10.1515/cclm-2015-0243.
[22]WU J R,CHEN I C,DAI Z K,et al.Early elevated B-type natriuretic peptide levels are associated with cardiac dysfunction and poor clinical outcome in pediatric septic patients[J].Acta Cardiol Sin,2015,31(6):485-493.DOI:10.1512/acem.27122912.
[23]王胜云,陈德昌.降钙素原和C-反应蛋白与脓毒症患者病情严重程度评分的相关性研究及其对预后的评估价值[J].中华危重病急救医学,2015,27(2):97-101.DOI:10.3760/cma.j.issn.2095-4352.2015.02.004. WANG S Y,CHEN D C.The correlation between procalcitonin,C-reactive protein and severity scores in patients with sepsis and their value in assessment of prognosis[J].Chinese Critical Care Medicine,2015,27(2):97-101.DOI:10.3760/cma.j.issn.2095-4352.2015.02.004.
[24]PODDAR B,GURJAR M,SINGH S,et al.Procalcitonin kinetics as a prognostic marker in severe sepsis/septic shock[J].Indian J Crit Care Med,2015,19(3):140-146.DOI:10.4103/0972-5229.152755.
[25]WACKER C,PRKNO A,BRUNKHORST F M,et al.Procalcitonin as a diagnostic marker for sepsis:a systematic review and meta-analysis[J].Lancet Infect Dis,2013,13(5):426-435.DOI:10.1016/S1473-3099(12)70323-7.
(本文编辑:贾萌萌)
Expression of Serum Procalcitonin and Its Impact on Prognosis in Sepsis
TANDe-min*,TANMeng-yuan,CHENJun,MENGZhen-fa,WANGYu-lin
IntensiveCareUnit,DanzhouCityPeople′sHospital,Danzhou571799,China
Objective To investigate the expression of serum procalcitonin(PCT)level and impact on prognosis in sepsis.Methods A total of 216 patients who were hospitalized the Intensive Care Unit,Danzhou City People′s Hospital and definitely diagnosed with sepsis from March 2012 to March 2016 were enrolled in this study.And they were divided into the survival group (n=134) and death group(n=82) based on the treatment outcome showed by a 28-day follow-up.Other 188 non-sepsis patients hospitalized in the hospital during the same period were selected as the subjects,too.We recorded all the subjects′ Acute Physiology and Chronic Health Evaluation Ⅱ(APACHE Ⅱ) score,Sequential Organ Failure Assessment (SOFA) score,levels of serum PCT,C-reactive protein(CRP) and brain natriuretic peptide(BNP).The factors affecting the prognosis of sepsis were analyzed with a multivariate Logistic regression model and their roles in predicting the prognosis of sepsis were investigated.Results Compared with the non-sepsis patients,sepsis patients had higher APACHEⅡ score,SOFA score,serum PCT level,CRP level and BNP level(P<0.01).The serum PCT levels on the 1st,3rd and 5th days of admission,and both the serum CRP and BNP levels on the 3rd and 5th days of admission were higher in the death group than those in the survival group(P<0.05).Patients in the death group were older,and they had higher APACHEⅡ,SOFA scores and AST compared with those in the survival group(P<0.05).Results of multivariate Logistic regression analysis demonstrated that the factors affecting the prognosis of sepsis were age〔OR=7.284,95%CI(3.605,14.727),P<0.05〕,APACHEⅡ score〔OR=3.162,95%CI(1.528,10.629),P<0.05〕,SOFA score〔OR=3.015,95%CI(1.054,9.582),P<0.05〕,serum PCT〔OR=1.046,95%CI(1.002,1.516),P<0.05〕,CRP〔OR=0.863,95%CI(0.715,0.985),P<0.05〕 and BNP〔OR=0.795,95%CI(0.653,0.952),P<0.05〕.ROC curve analysis indicated that the area under curve (AUC) and optimal threshold of age,APACHEⅡ scoring,SOFA scoring,PCT,CRP and BNP levels for predicting death in sepsis respectively was 0.803(63.0 years),0.826(22.3 points),0.765(7.1 points),0.849(6.9 μg/L),0.684(49 mg/L),0.626(825 ng/L).Pearson correlation analysis revealed that in the death group,the level of serum PCT was positively correlated with age,APACHE Ⅱ score,SOFA score,CRP and BNP levels(P<0.05).Conclusion The level of serum PCT is significantly elevated in patients with sepsis.Older age,higher APACHE Ⅱ and SOFA scores,higher PCT,CRP and BNP levels are independent risk factors for prognosis in sepsis.
Sepsis;Procalcitonin;Intensive care unit;Risk factors
海南省医药卫生科研基金项目(15A200264)
R 631
A
10.3969/j.issn.1007-9572.2017.05.004
2016-09-10;
2016-12-27)
571799海南省儋州市人民医院重症医学科
*通信作者:谭德敏,主治医师;E-mail:xiaohuan232565650@163.com
谭德敏,谭孟源,陈军,等.脓毒症患者血清降钙素原的表达及其对预后的影响研究[J].中国全科医学,2017,20(5):520-525.[www.chinagp.net]
TAN D M,TAN M Y,CHEN J,et al.Expression of serum procalcitonin and its impact on prognosis in sepsis[J].Chinese General Practice,2017,20(5):520-525.
*Correspondingauthor:TANDe-min,Attendingphysician;E-mail:xiaohuan232565650@163.com
