Diagnosis and outcomes of collateral arterial formation after irreversible early hepatic artery thrombosis in pediatric liver recipients
2017-02-10
Shanghai, China
Diagnosis and outcomes of collateral arterial formation after irreversible early hepatic artery thrombosis in pediatric liver recipients
Li-Hong Gu, Feng-Hua Li, Qiang Xia, Hua Fang, Shi-Jun Zhang and Long-Zhi Han
Shanghai, China
BACKGROUND: Early hepatic artery thrombosis (eHAT) has been recognized as an important cause of graft loss and mortality. However, the incidence, etiology and outcome are not clear, especially for children. The present study was to investigate the formation of collateral artery fow after irreversible eHAT and its impact on patient's prognosis.
METHODS: We analyzed eHAT after liver transplantation in children from October 2006 to April 2015 in our center, illustrated the formation of collateral hepatic artery fow after irreversible eHAT and explored the diagnosis, complications, treatment and prognosis. The basic and follow-up ultrasonographic images were also compared.
RESULTS: Of the 330 pediatric liver recipients, 22 (6.67%) developed eHAT within 1 month. Revascularization attempts including surgical thrombectomy, interventional radiology and conservational treatment (thrombolysis) were successful in 5 patients. Among the 17 patients who had irreversible eHAT, follow-up ultrasonography revealed that collateral artery fow was developed as early as 2 weeks after eHAT. Liver abscess and bile duct complication occurred secondary to eHAT in variable time.
CONCLUSIONS: Collateral arterial formation is a compensatory adaptation to eHAT to supply blood to liver grafts. However, the severe bile duct damage secondary to eHAT is irreversible and retransplantation is unavoidable.
(Hepatobiliary Pancreat Dis Int 2017;16:39-44)
ultrasonography;
liver transplantation;
children;
hepatic artery thrombosis;
collateral arterial formation
Introduction
There is currently no solitary defnition of early hepatic artery thrombosis (eHAT), the time is defned from 2 weeks to 3 months. However, for practical purposes, HAT within 1 month of liver transplantation (LT) is a clinically useful defnition of eHAT.[1-3]eHAT is a lethal vascular complication after LT, and is a major cause of graft loss (53.1%) and mortality (33.3%) in the early postoperative period.[4]The incidence of eHAT occurs in 8.3% of children and 2.9% of adults undergone LT.[4]Liver abscess and bile duct complications are secondary to irreversible eHAT, and have a negative effect on the outcome and survival of LT recipients.[5-7]Traditionally, retransplantation was the frst choice to treat eHAT. However, the application of this approach is restricted by the limited availability of donor organs.[8-11]Though early treatment was useful for the revascularization of HAT, some recipients developed irreversible HAT.[12,13]It is reported that collateral arterial formation is detectable in the irreversible recipients by ultrasonography.[14,15]The present study reviewed patients with eHAT and illustrated the formation of collateral artery fow after irreversible eHAT and its impact on patient's prognosis.
Methods
Patients
We retrospectively reviewed pediatric liver recipients with eHAT between October 2006 and April 2015. Patients with eHAT in the present study was defned asthose diagnosed within 1 month after LT. A total of 330 consecutive patients under eighteen years old with a full size or living donor LT (LDLT) at the department of liver surgery in our hospital were included using the previous reported surgical technique.[16,17]The study was performed according to the principles of theDeclaration of Helsinkiand was approved by the ethics committee of our hospital.
In our study, eHAT was defned as HAT occurring within 1 month after LT. HAT occurring more than 1 month after LT, is less common. Its causes are less well defned and may have a different evolution and outcome.[18]
Diagnosis of HAT was initially made by ultrasound. CT angiography served as an important supplement, and the diagnosis was confrmed by arteriography or surgery. Surgery or interventional radiology was performed immediately (within two hours) after the diagnosis of eHAT. The decision to operate or perform interventional radiology primarily depended on the surgeon's experience. Surgical revascularization was preferred over interventional radiology in cases of eHAT occurring within 1 week after LT. If the recipient had unstable vital signs, thrombolysis was chosen as a conservative treatment. We usually chose low molecular weight heparin or warfarin and prevented the side effect by keeping the INR between 1.5-2.0.
Doppler ultrasound
Ultrasound was performed using a Philips Envisor scanner (Philips Medical Systems, Andover, MA, USA) with a convex probe of 3.5 MHz in the imaging and Doppler mode. Prior to May 2009, Doppler ultrasound was performed during the frst three days after LT, and then performed when there were clinical manifestations or laboratory abnormalities. After May 2009, patients were enrolled in a follow-up protocol, which included routine daily ultrasound in the frst postoperative week and then once a week during the frst month. Extra ultrasound examination would be performed if it was needed in response to clinical or laboratory abnormalities. All studies were performed by experienced radiologists (9 year 1200 cases experience in liver transplantation radiology), and any patient with absent arterial fow on ultrasound was rescanned by another radiologist (11 year 1500 cases experience in liver transplantation radiology). Before May 2009, among 22 pediatric liver recipients, 1 had eHAT; after May 2009, 21 out of 308 pediatric liver recipients suffered eHAT.
Following treatment of HAT, ultrasound examination was performed immediately and daily in the frst three days to confrm the patency of hepatic artery (HA) and the velocity of blood fow. Extra ultrasound examination was performed when necessary. Routine ultrasound was performed every three months after discharge. Extra ultrasound examination was performed whenever necessary. The HA was imaged at the porta hepatis, just anterior to the portal vein (PV), and then within the liver following the course of the right or left PV. Measurements included peak systolic and end diastolic velocities and the resistance index [RI=(peak systolic velocity - end diastolic velocity)/peak systolic velocity]. In the irreversible HAT cases, the collateral artery blood fow was detected around the PV by ultrasonography and confrmed by digital subtraction angiography or CT angiography. The liver parenchyma, bile ducts were also evaluated by ultrasound.
Recorded data included the time between transplantation and the development of eHAT, treatment (surgical thrombectomy and re-anastomosis, interventional radiology, thrombolysis, or retransplantation), the successful rate of revascularization, the time of collateral artery fow formation in the irreversible cases, the RI and peak systolic velocity of the collateral artery fow, and the occurrence of complications (abscess or biliary) secondary to eHAT detected by follow-up ultrasound.
Statistical analysis
Statistical analyses were performed using SPSS, version 20 for Windows (SPSS, Chicago, IL, USA), and aPvalue less than 0.05 was considered statistically signifcant. The demographic characteristics of the patients are summarized with frequency counts, means, and standard deviations. Differences in gender, age, body weight, type of graft and underlying diseases between the eHAT and non-eHAT groups were evaluated using the test and independentttest.
Results
Twenty-two (6.67%) of 330 pediatric liver recipients developed eHAT. The average age and weight in the eHAT group and non-eHAT group were 15.80±18.56 vs 24.89± 35.18 months and 10.07±6.88 vs 11.76±9.60 kg, respectively. The incidence of eHAT was 25.58% (11/43) in full size LT and 3.83% (11/287) in LDLT. The underlying diseases included biliary atresia (n=286), other cholestasis disease (n=14), metabolic liver disease (n=14), cirrhosis (n=5), and others (n=11). Biliary atresia accounted for more than 85% of cases (Table 1).
All cases of eHAT were detected by ultrasound and confrmed by surgery or hepatic angiography. Seventeen (77.27%) of the 22 LT recipients developed eHAT within the frst postoperative week. The other fve occurred day 9, 10, 10, 10 and 26. Surgical thrombectomy was performed in11 recipients, interventional radiology in 6, thrombectomy combined with interventional radiology in 1, conservation treatment in 4. Revascularization was successful in fve patients, but failed in 17 (Fig. 1). One of the patients who had initially successful revascularization by interventional radiology had a reoccurrence of eHAT two days later.
In the fve patients who had successfully revascularized, the average RI was 0.66±0.08 (range 0.54-0.78) and the average peak systolic velocity was 58.94±21.53 cm/s (range 37.8-95.7) after treatment of eHAT. Liver abscess developed in one recipient 6 days after the occurrence of eHAT, and dilatation of bile duct developed in three recipients in 48 days, 53 days and 9 months after eHAT, respectively. Biliary surgery was performed in one case for severe bile duct dilatation and biliary sludge formation. This patient fnally received retransplantation in 1 year after the frst transplantation. One recipient died forsevere abdominal infection 3 weeks after eHAT. Two recipients were alive with bile duct complication and 1 was alive without complication.
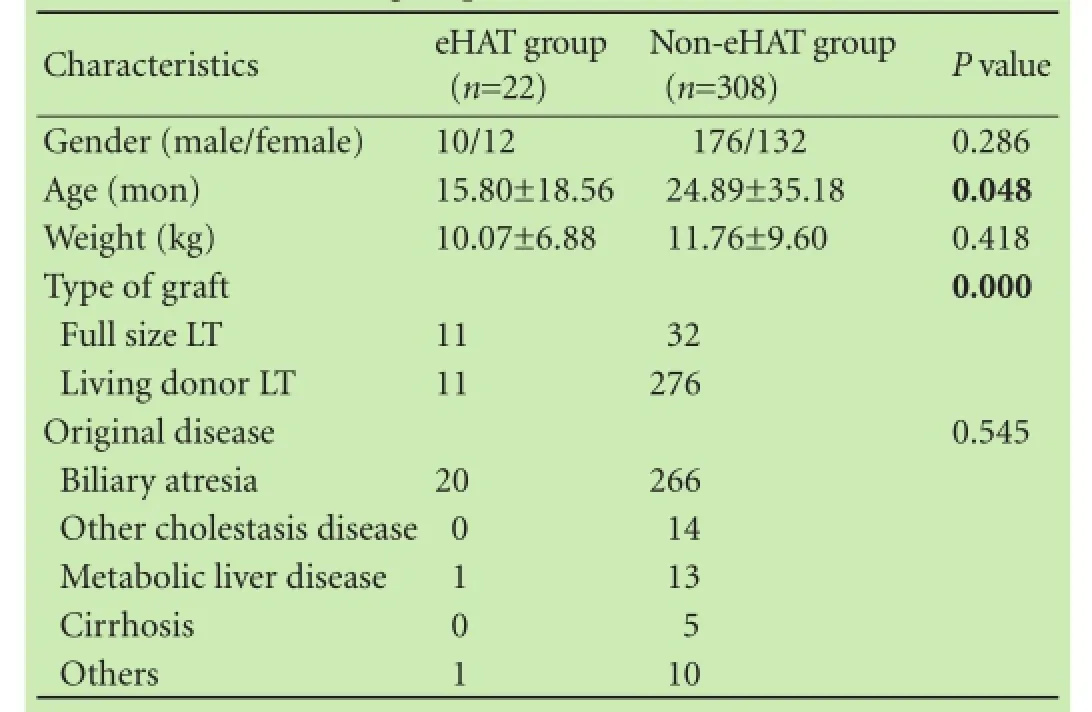
Table 1. Demographic characteristics of LT recipients in the eHAT and non-eHAT groups
In the 17 irreversible cases of eHAT, four died at postoperative day 5, 5, 7 and 10 and no collateral artery fow. In the remaining 13 cases, the mean time of the detection of collateral artery fow after eHAT was 25.00 ±6.25 days with a range from 14 to 36 days (Table 2). A low RI and low velocity artery fow next to the PV in the liver could be detected by ultrasound (Fig. 2). The average RI was 0.56±0.08 (range 0.42-0.76) and the average peak systolic velocity was 31.98±6.13 cm/s (range 22.00-48.80). The average RI levels within the frst postoperative week were 0.75±0.09 in pediatric recipients without eHAT and the average peak systolic velocity levels within the frst postoperative week were 50.49±19.89 cm/s. Liver abscess was detected in 8 cases (8/17) between 2 and 20 days after the development of eHAT and was self-limited. Biliary complications developed in seven cases (7/17) and occurred from 23 days to 90 days after eHAT.
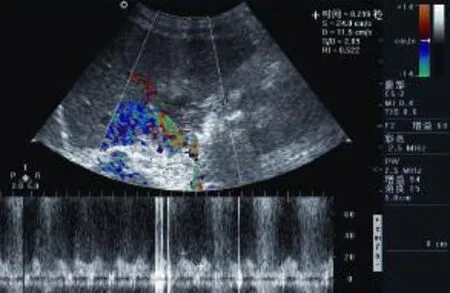
Fig. 2. Ultrasound images showing the collateral artery fow. Note that the peak systolic velocity of the artery is low measuring approximately 24 cm/s and resistance index in the hepatic artery is low measuring approximately 0.52.
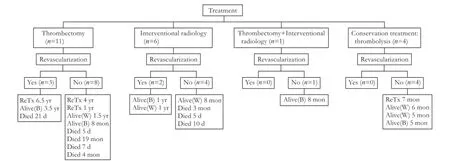
Fig. 1. Diagnosis, treatment and survival of LT recipients with eHAT. Alive(B): alive with bile duct complication; Alive(W): alive well; ReTx: retransplantation.

Table 2. Collateral artery fow after eHAT detected by ultrasonography following LT
Three of the 13 cases with collateral artery fow died in 3, 4 and 19 months after eHAT, allograft failure associated with vascular thrombosis and multiple system organ failure was the primary cause of death. Retransplantation was performed in three cases in 3, 8 and 48 months after eHAT for severe bile duct complication. The remaining seven patients survived, 4 were with no complication and 3 with bile duct complication.
Discussion
Our analysis showed that the HAT rate is signifcantly higher in full size LT compared with LDLT. The explanations might be compared with LDLT, the HA is usually longer and thinner in the deceased donor liver, resulting in a higher risk of kink or distortion; the intima injury is probably more severe in deceased donor liver due to the longer ischemia time and procurement damage, leading to higher thrombosis risk; the full sized liver had a wider end which might affect the blood supply.
Urgent retransplantation is the frst choice for the treatment of eHAT. However, the shortage of liver donor and the worse condition of the children made it diffcult to perform an emergency retransplantation.[9-11]Surgical thrombectomy, interventional radiology and conservation treatment were chosen to treat eHAT in our study. We found that majority of the patients with irreversible eHAT developed collateral artery fow and the formation time was 14-36 days. Collateral artery fow is a compensatory adaptation of eHAT to supply liver grafts blood fow. Stringer et al[8]reported the formation of collateral artery fow within 3 weeks after LT, which was well developed by 3 months. The present study found that collateral artery fow developed as early as 2 weeks after eHAT with a low RI and low peak systolic velocity. It was reported that collateral artery fow supply from the surface capsular and phrenic branches, the branches of the superior mesenteric artery or, rarely, the post-thrombot-ic recanalization of the HA.[8,19,20]We proposed that the collateral artery is from the original arteries, since the interval between the occurrence of eHAT and collateral detection is relatively short (14-36 days) and the time might not be enough to create a new artery.
Hall et al[21]illustrated that collateral artery fow might be misdiagnosis as normal HA fow by ultrasound which caused false negative cases of HAT. In this regard, routine ultrasound is necessary because it can diagnose the occurrence of HAT at the frst time and differentiate the following collateral artery fow from the normal HA. The present study found that collateral artery was tiny and the fow was slow with low resistance at the porta hepatis and within the liver following the course of the PV branch. The total blood fow was lower than that with successful revascularization fow. de Jong et al[22]described the implantable continuous Doppler monitoring device for detection of eHAT after LT. The accuracy was increased from 93% to 99%. Although ultrasound had a high sensitivity and accuracy in diagnosis of eHAT in our study, the intermittent character of ultrasound (once daily in the frst week in our center) can cause a considerable delay in the diagnosis. Continuous monitoring of arterial fow would shorten the time between the thrombotic event and the surgical intervention. This offers the best chance for an early management and prevention of a retransplantation.
Early detection and treatment of eHAT alleviate liver abscess and bile duct complications.[23,24]Some of the recipients with revascularization or collateral artery fow need retransplantation if the bile duct complication was severe. In the LT recipients, the arterial vessels supplying the biliary tract are disrupted and HA is the only supply to bile duct. The ischemic biliary tree sheds damaged biliary epithelium, the bile duct ischemia made the patient susceptible to liver abscess and bile duct complication.[11,25]Although the vascularization of HA or collateral artery fow supplies blood to the bile duct, the bile duct damage is irreversible.
Our study has several limitations. First, we couldn't confrm the long-term survival rate of all the recipients with eHAT. Second, although routine ultrasound was performed daily in the frst postoperative week, after that it was only performed when indicated by laboratory or clinical abnormalities. Five cases were diagnosed with eHAT after the frst week, there might be an interval between the onset of eHAT and diagnosis.
In conclusion, eHAT is a serious vascular complication that occurs in children after LT, with a high rate of mortality and morbidity. Patients with irreversible eHAT typically developed arterial collaterals in two weeks. However, the blood fow is far much lower than those with successful revascularization fow. Collateral artery fow is a compensatory adaptation of eHAT to supply liver grafts blood fow. However, the bile duct damage secondary to eHAT is irreversible and retransplantation could not be avoided in those cases with severe bile duct complication.
Contributors:LFH and XQ proposed the study. GLH and FH performed the research and wrote the frst draft. ZSJ and HLZ collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. LFH is the guarantor.
Funding:This study was supported by a grant from the Science and Research of Shanghai's Health Bureau (20134Y019).
Ethical approval:Informed consents were obtained from all donors. Each organ donation was approved by the Institutional Review Board, Renji Hospital, School of Medicine, Shanghai Jiaotong University and was strictly in accordance with the guidelines of the Ethics Committee of the hospital, the current regulation of the Chinese Government, and theDeclaration of Helsinki.
Competing interest:No benefts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Unal B, Gonultas F, Aydin C, Otan E, Kayaalp C, Yilmaz S. Hepatic artery thrombosis-related risk factors after living donor liver transplantation: single-center experience from Turkey. Transplant Proc 2013;45:974-977.
2 Fan J, Nishida S, Selvaggi G, Levi D, Tekin A, Weppler D, et al. Factor V Leiden mutation is a risk factor for hepatic artery thrombosis in liver transplantation. Transplant Proc 2013;45:1990-1993.
3 Oh CK, Pelletier SJ, Sawyer RG, Dacus AR, McCullough CS, Pruett TL, et al. Uni- and multi-variate analysis of risk factors for early and late hepatic artery thrombosis after liver transplantation. Transplantation 2001;71:767-672.
4 Bekker J, Ploem S, de Jong KP. Early hepatic artery thrombosis after liver transplantation: a systematic review of the incidence, outcome and risk factors. Am J Transplant 2009;9:746-757.
5 Wozney P, Zajko AB, Bron KM, Point S, Starzl TE. Vascular complications after liver transplantation: a 5-year experience. AJR Am J Roentgenol 1986;147:657-663.
6 Bucuvalas JC, Ryckman FC, Atherton H, Alonso MP, Balistreri WF, Kotagal U. Predictors of cost of liver transplantation in children: a single center study. J Pediatr 2001;139:66-74.
7 Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA. Complications and costs after high-risk surgery: where should we focus quality improvement initiatives? J Am Coll Surg 2003;196:671-678.
8 Stringer MD, Marshall MM, Muiesan P, Karani JB, Kane PA, Mieli-Vergani G, et al. Survival and outcome after hepatic artery thrombosis complicating pediatric liver transplantation. J Pediatr Surg 2001;36:888-891.
9 Nikeghbalian S, Kazemi K, Davari HR, Salahi H, Bahador A, Jalaeian H, et al. Early hepatic artery thrombosis after liver transplantation: diagnosis and treatment. Transplant Proc 2007;39:1195-1196.
10 Zhou J, Fan J, Shen YH, Wang JH, Wu ZQ, Qiu SJ, et al. Diagnosis and management for early hepatic artery thrombosis after liver transplantation. Zhonghua Yi Xue Za Zhi 2005;85:1670-1673.
11 Heaton ND. Hepatic artery thrombosis: conservative management or retransplantation? Liver Transpl 2013;19:S14-16.
12 Ackermann O, Branchereau S, Franchi-Abella S, Pariente D, Chevret L, Debray D, et al. The long-term outcome of hepatic artery thrombosis after liver transplantation in children: role of urgent revascularization. Am J Transplant 2012;12:1496-1503.
13 Nishida S, Kato T, Levi D, Naveen M, Berney T, Vianna R, et al. Effect of protocol Doppler ultrasonography and urgent revascularization on early hepatic artery thrombosis after pediatric liver transplantation. Arch Surg 2002;137:1279-1283.
14 Fouzas I, Sklavos A, Bismpa K, Paxiadakis I, Antoniadis N, Giakoustidis D, et al. Hepatic artery thrombosis after orthotopic liver transplantation: 3 patients with collateral formation and conservative treatment. Transplant Proc 2012;44:2741-2744.
15 Han B, Liu C, Tian H, Liu Y, Yu L, Liu X, et al. Formation of collateral circulation within hepatic parenchyma after recurrent hepatic artery thrombosis and thrombolysis early after liver transplantation: case report. Transplantation 2009;87:1591-1592.
16 Zhu JJ, Xia Q, Zhang JJ, Xue F, Chen XS, Li QG, et al. Living donor liver transplantation in 43 children with biliary atresia: a single-center experience from the mainland of China. Hepatobiliary Pancreat Dis Int 2012;11:250-255.
17 Zhou J, Shen Z, He Y, Zheng S, Fan J. The current status of pediatric liver transplantation in Mainland China. Pediatr Transplant 2010;14:575-582.
18 Gu LH, Fang H, Li FH, Zhang SJ, Han LZ, Li QG. Preoperative hepatic hemodynamics in the prediction of early portal vein thrombosis after liver transplantation in pediatric patients with biliary atresia. Hepatobiliary Pancreat Dis Int 2015;14:380-385.
19 Vaidya S, Dighe M, Bhargava P, Dick AA. Chronic hepatic artery occlusion with collateral formation: imaging fndings and outcomes. Transplant Proc 2011;43:1770-1776.
20 Casadaban L, Parvinian A, Tzvetanov IG, Jeon H, Oberholzer J, Benedetti E, et al. Unconventional extrahepatic neovascularization after transplant hepatic artery thrombosis: a case report. Transplant Proc 2013;45:2841-2844.
21 Hall TR, McDiarmid SV, Grant EG, Boechat MI, Busuttil RW. False-negative duplex Doppler studies in children with hepatic artery thrombosis after liver transplantation. AJR Am J Roentgenol 1990;154:573-575.
22 de Jong KP, Bekker J, van Laarhoven S, Ploem S, van Rheenen PF, Albers MJ, et al. Implantable continuous Doppler monitoring device for detection of hepatic artery thrombosis after liver transplantation. Transplantation 2012;94:958-964.
23 García-Criado A, Gilabert R, Nicolau C, Real I, Arguis P, Bianchi L, et al. Early detection of hepatic artery thrombosis after liver transplantation by Doppler ultrasonography: prognostic implications. J Ultrasound Med 2001;20:51-58.
24 Horrow MM, Blumenthal BM, Reich DJ, Manzarbeitia C. Sonographic diagnosis and outcome of hepatic artery thrombosis after orthotopic liver transplantation in adults. AJR Am J Roentgenol 2007;189:346-351.
25 Dodd GD 3rd, Memel DS, Zajko AB, Baron RL, Santaguida LA. Hepatic artery stenosis and thrombosis in transplant recipients: Doppler diagnosis with resistive index and systolic acceleration time. Radiology 1994;192:657-661.
Received April 13, 2016
Accepted after revision November 21, 2016
Author Affliations: Department of Ultrasound (Gu LH, Li FH, Fang H and Zhang SJ) and Department of Liver Surgery (Xia Q and Han LZ), Renji Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai 200127, China
Feng-Hua Li, MD, Department of Ultrasound, Renji Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai 200127, China (Tel: +86-21-68383396; Fax: +86-21-50896639; Email: renjilfh@163.com)
© 2017, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(16)60165-0
Published online December 28, 2016.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Instructions for Authors
- The consensus on liver autotransplantation from an international panel of experts
- Associating liver partition and portal vein ligation for staged hepatectomy: the current role and development
- Right hepatectomy in living donors with previous abdominal surgery
- Cytokines are early diagnostic biomarkers of graft-versus-host disease in liver recipients
- Resection of T4 hepatocellular carcinomas with adjacent structures, is it justifed?