人附睾分泌蛋白4在各分期慢性肾脏疾病患者血清中变化及临床价值
2017-01-06王晓亮赵英水
王晓亮,赵英水
(1.榆林市第一医院检验科,陕西 榆林 719000;2.西北大学,陕西 西安 710000)
人附睾分泌蛋白4在各分期慢性肾脏疾病患者血清中变化及临床价值
王晓亮1,赵英水2
(1.榆林市第一医院检验科,陕西 榆林 719000;2.西北大学,陕西 西安 710000)
目的 探讨人附睾分泌蛋白4(HE4)在各分期慢性肾脏疾病患者血清中变化及临床价值。方法 选取慢性肾脏疾病(CKD)患者136例,根据肾小球滤过率(eGRF)值将患者分为CKD1期(n=41)、CKD2期(n=33)、CKD3期(n=17)、CKD4期(n=21)和CKD5期(n=24),将eGRF<60 mL·min-1作为肾功能不全的诊断标准,同期,选取健康者40例作为对照组,检测血尿素氮(BUN)、肌酐(Scr)、尿酸(UA)和胱蛋白酶抑制剂C(CysC)水平,利用酶联免疫吸附试验(ELISA法)对血清中HE4水平进行检测,利用受试者工作特征曲线(ROC曲线)对血清中不同指标在预测肾功能不全中的价值进行分析。结果 与对照组相比,CKD患者血清HE4、BUN、Scr、UA和CysC水平均升高,CKD患者中,CKD3期、CKD4期和CKD5期患者血清HE4、BUN、Scr、UA和CysC水平均高于CKD1期和CKD2期患者,且CKD2期患者血清HE4高于CKD1期,差异均有统计学意义(P<0.05);Pearson相关分析显示,CKD患者血清中HE4水平与BUN、Scr和CysC均呈正相关(r=0.295、0.342和0.416,P<0.05),Spearman相关分析显示,CKD患者血清中HE4水平与CKD分期呈正相关(rs=0.497,P<0.05);ROC曲线分析显示,CKD患者血清中HE4、BUN、Scr、UA和CysC均对肾功能不全具有预测价值,且HE4在预测肾功能不全时,曲线下面积、灵敏度和特异度均优于BUN、Scr、UA和CysC。结论 HE4在CKD患者血清中出现升高,且随患者分期而逐渐增加,可作为早期发现肾功能不全的辅助诊断指标。
慢性肾脏疾病;人附睾分泌蛋白4;分期;肾功能不全
慢性肾脏疾病(chronic kidney disease,CKD)作为肾内科常见病,具有发病率高、伴发心血管病率高、病死率高等特点,近年来,随着人们生活方式及饮食结构的改变,CKD发病率呈上升趋势,严重威胁人类健康[1]。CKD病程进展是个缓慢的过程,终末期会导致尿毒症而威胁患者生命,因此,早期发现并进行有效的控制干预,有助于阻止病程进展,改善患者预后[2]。人附睾分泌蛋白4(human epididymis protein 4,HE4)作为新近发现的肿瘤标志物,广泛表达于生殖系统、乳腺上皮、上呼吸道、肾远曲小管等组织中,具有免疫调节和抑制细胞增殖的功能[3],与卵巢癌、子宫内膜癌、泌尿系统移行细胞癌、肺癌等多种恶性肿瘤发生有关,其诊断灵敏度和特异度均优于糖类抗原125(CA125)[4]。也有研究指出[5],血清HE可反映男性肾损伤肾小球滤过功能。本研究拟对各分期慢性肾脏疾病患者血清中HE变化进行分析,探讨其对严重肾功能衰竭和尿毒症的诊断价值,以期为临床实践提供基础资料。
1 资料与方法
1.1 一般资料 选取2013年3月至2016年4月在榆林市第一医院肾内科住院治疗的CKD患者136例,其中,男性61例,女性75例,年龄25~79岁,平均年龄(63.8±10.5)岁,原发病类型:慢性肾小球肾炎35例,肾盂肾炎11例,糖尿病肾病17例,肾病综合征23例,狼疮性肾炎9例,紫癜性肾炎2例,IgA肾病13例,高血压肾病26例。所有患者均符合2002年K/DOQI《慢性肾脏病临床实践指南》中相关诊断标准[6]。排除肾功能急性恶化者、接受血液透析治疗者、心功能严重不全者、急慢性感染者、自身免疫系统疾病者、内分泌系统疾病者、恶性肿瘤者。根据CKD-EPI公式计算的肾小球滤过率(eGRF)值对患者进行分组[7]:CKD1期41例:eGRF≥90 mL·min-1;CKD2期33例:60 mL·min-1≤eGRF<90 mL·min-1;CKD3期17例:30 mL·min-1≤eGRF<60 mL·min-1;CKD4期21例:15 mL·min-1≤eGRF<30 mL·min-1;CKD5期24例:eGRF<15 mL·min-1;将eGRF<60 mL·min-1作为肾功能不全的诊断标准。同期,从体检中心选取健康者40例作为对照组,其中,男性18例,女性22例,平均年龄(62.9±9.8)岁,排除肾脏疾病、恶性肿瘤、急慢性感染和其他慢性病史者。本研究获榆林市第一医院伦理委员会批准,患者或近亲属对研究方案签署知情同意书。
1.2 方法 所有研究对象均抽取晨起空腹静脉血6 mL,常温下于3 500 r·min-1离心10 min,留取血清分装于两个抗凝管中,保存于-70 ℃冰箱以备检。利用日立7600全自动生化分析仪及配套试剂对尿素氮(BUN)、肌酐(SCr)、尿酸(UA)和胱蛋白酶抑制剂C(CysC)进行检测。利用酶联免疫吸附试验(ELISA法)对血清中HE4水平进行检测,试剂盒购自上海研卉生物科技有限公司,所有操作均按照试剂盒说明进行。
2 结果
2.1 CKD患者和对照组血清中HE4、BUN、Scr、UA和CysC比较 与对照组相比,CKD患者血清HE4、BUN、SCr、UA和CysC水平均升高,差异均有统计学意义(P<0.05);CKD患者中,CKD3期、CKD4期和CKD5期患者血清HE4、BUN、SCr、UA和CysC水平均高于CKD1期和CKD2期患者,且CKD2期患者血清HE4高于CKD1期,均差异有统计学意义(P<0.05),见表1。
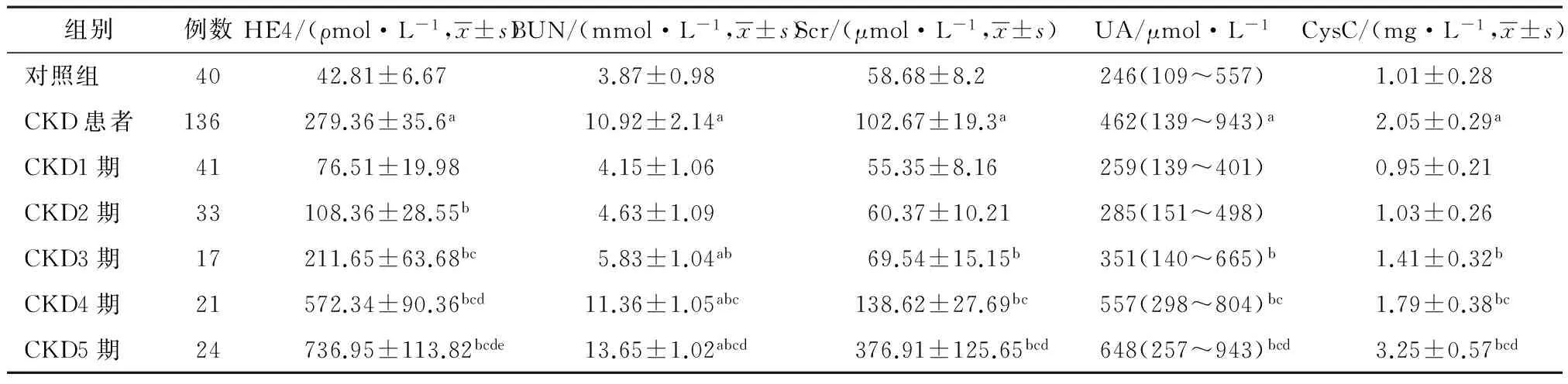
表1 CKD患者和对照组血清中HE4、BUN、Scr、UA和CysC比较
注:与对照组相比,aP<0.05;与CKD1期相比,bP<0.05;与CKD2期相比,cP<0.05;与CKD3期相比,dP<0.05;与CKD4期相比,eP<0.05。
2.2 CKD患者血清中HE4水平与其他指标相关性 Pearson相关分析显示,CKD患者血清中HE4水平与BUN、SCr和CysC均呈正相关(r=0.295、0.342和0.416,P<0.05);Spearman相关分析显示,CKD患者血清中HE4水平与CKD分期呈正相关(rs=0.497,P<0.05)。
2.3 CKD患者血清中不同指标在预测肾功能不全中的价值 ROC曲线分析显示,CKD患者血清中HE4、BUN、SCr、UA和CysC均对肾功能不全具有预测价值,且HE4在预测肾功能不全时,曲线下面积、灵敏度和特异度均优于BUN、SCr、UA和CysC,见表2。
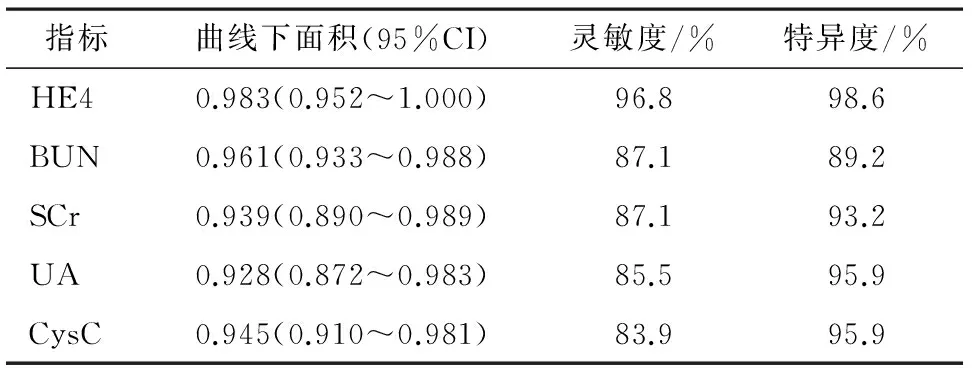
表2 CKD患者血清中不同指标在预测肾功能不全中的价值
3 讨论
CKD是发病率较高、危害较大的肾脏疾病,但该病早期诊断及人群知晓率却较低,有研究指出[8],我国成人CKD患病率高达10.8%,但知晓率不足13.0%。已成为威胁人类健康的一大“杀手”。 HE4作为一种新发现的肿瘤标志物,是早期诊断女性上皮性卵巢癌的指标[9],有研究指出[10],HE4可能通过抑制多种蛋白酶活性而参与了肾脏纤维化过程。也有研究指出[11],HE4可表达于人肾远曲小管中。本研究显示,与对照组相比,CKD患者血清HE4升高,CKD患者中,CKD3期、CKD4期和CKD5期患者血清HE4水平均高于CKD1期和CKD2期患者,且CKD2期患者血清HE4高于CKD1期,说明CKD患者血清中HE水平出现升高,且随着患者分期而逐渐增加,提示血清中HE水平可能与CKD患者病情进展有关。
BUN和SCr是反映肾功能的常用指标,在肾功能损害早期不敏感,但可在正常范围内,当肾小球率过滤降低至正常值50%以下时,浓度迅速上升[12],UA亦是反映肾脏排泄功能的指标,但易受年龄、性别、饮食等因素的影响[13],CysC作为近年来广泛用于评价肾小球滤过功能的指标,可更好的反映肾小球滤过功能[14],本研究显示,与对照组相比,CKD患者血清BUN、SCr、UA和CysC水平均升高, CKD患者中,CKD3期、CKD4期和CKD5期患者血清BUN、SCr、UA和CysC水平均高于CKD1期和CKD2期患者,说明CKD患者肾小球滤过功能受损,且四项指标均在CKD3期及以上时迅速升高,提示这些指标对早期肾功能变化不敏感。Pearson相关分析显示,CKD患者血清中HE4水平与BUN、SCr和CysC均呈正相关,Spearman相关分析显示,CKD患者血清中HE4水平与CKD分期呈正相关,进一步说明CKD患者血清中HE4水平与患者肾小球滤过功能有关,可作为评估CKD患者病情严重程度的参考指标。ROC曲线分析显示,CKD患者血清中HE4、BUN、SCr、UA和CysC均对肾功能不全具有预测价值,且HE4在预测肾功能不全时,曲线下面积、灵敏度和特异度均优于BUN、SCr、UA和CysC,说明CKD患者血清中HE4对早期发现肾功能不全具有重要辅助诊断价值。
综上所述,CKD患者血清中HE4水平出现升高,且随患者分期而逐渐增加,可作为早期发现肾功能不全的辅助诊断指标,因此,对于临床上发现患者血清HE4水平升高时,应排除CKD的可能。
[1] Clarke AL,Yates T,Smith AC,et al.Patient's perceptions of chronic kidney disease and their association with psychosocial and clinical outcomes:a narrative review[J].Clin Kidney J,2016,9(3):494-502.
[2] Larmour KE,Maxwell AP,Courtney AE.Improving early detection of chronic kidney disease[J].Practitioner,2015,259(1779):19-23,2-3.
[3] Chang X,Ye X,Dong L,et al.Human epididymis protein 4(HE4)as a serum tumor biomarker in patients with ovarian carcinoma[J].Int J Gynecol Cancer,2011,21(5):852-858.
[4] 唐雨曦,罗晨辉,王瑛,等.人附睾蛋白4(HE4)在恶性肿瘤中的表达与临床进展[J].肿瘤药学,2015,5(2):87-91.
[5] 贺艳光,仇燕,刘然,等.人附睾分泌蛋白4在男性肾损伤诊断中的价值[J].中华实用诊断与治疗杂志,2016,30(1):80-82.
[6] National Kidney Foundation.K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease[J].Am J Kidney Dis,2003,42(4 Suppl 3):201-205.
[7] 王长安,刘金瑞,张靖华.基于血清胱抑素C的肾小球滤过率评估方程在评价移植肾功能中的应用[J].中华器官移植杂志,2015,36(6):339-342.
[8] Zhang L,Wang F,Wang L,et al.Prevalence of chronic kidney disease in China:a cross-sectional survey[J].Lancet,2012,379(9818):815-822.
[9] Dikmen ZG,Colak A,Dogan P,et al.Diagnostic performances of CA125,HE4,and ROMA index in ovarian cancer[J].Eur J Gynaecol Oncol,2015,36(4):457-462.
[10] Allison SJ.Fibrosis:HE4 — a biomarker and target in renal fibrosis[J].Nat Rev Nephrol,2013,9(3):124-128.
[11] Galgano MT,Hampton GM,Frierson HF Jr.Comprehensive analysis of HE4 expression in normal and malignant human tissues[J].Mod Pathol,2006,19(6):847-853.
[12] Wang YT,Fu JJ,Li XL,et al.Effects of hemodialysis and hemoperfusion on inflammatory factors and nuclear transcription factors in peripheral blood cell of multiple organ dysfunction syndrome[J].Eur Rev Med Pharmacol Sci,2016,20(4):745-750.
[13] 郭琴,罗薇,银代淑,等.体检人群尿微量白蛋白肌酐比的临床意义[J].四川大学学报(医学版),2016,47(1):122-127.
[14] Brou NA,Jacqz-Aigrain E,Zhao W.Cystatin C as a potential biomarker for dosing of renally excreted drugs[J].Br J Clin Pharmacol,2015,80(1):20-27.
Changes of serum HE3 levels in various stages of chronic kidney disease and its clinical significance
WANG Xiaoliang1,ZHAO Yingshui2
(1.DepartmentofLaboratory,FirstHospitalofYulinCity,Yulin,Shaanxi719000,China;2.NorthwestUniversity,Xi’an,Shaanxi710000,China)
Objective To investigate the changes of serum human epididymis protein 4(HE3)levels in various stages of chronic kidney disease and its clinical significance.Methods Totally136 cases of patients with chronic kidney disease(CKD)were selected.According to estimated glomerular filtration rate(eGRF),the patients were assigned stage 1 group(n=41),stage 2 group(n=33),stage 3 group(n=17),stage 4 group(n=21)and stage 5 group(n=24).The eGFR<60 mL·min-1was used as the diagnostic criteria for renal dysfunction.In the same period,40 healthy subjects were selected as control group.The blood urea nitrogen(BUN),serum creatinine(Scr),uric acid(UA)and cystatin C(CysC)were detected.The serum level of HE4 was detected by using enzyme-linked immunosorbent assay(ELISA method).The values of different indicators in predicting renal dysfunction were analyzed by using receiver operating characteristic curve(ROC curve).Results Compared with the control group,the serum levels of HE4,BUN,Scr,UA and CysC in patients with CKD were increased.Among the patients with CKD,the serum levels of HE4,BUN,Scr,UA and CysC in stage 3 group,stage 4 group and stage 5 group were higher than stage 1 group and stage 2 group,and the serum level of HE4 in stage 2 group was higher than stage 1 group.The differences were statistically significant(P<0.05).Pearson correlation analysis showed that the serum level of HE4 in patients with CKD was positively correlated with BUN,Scr and CysC(r=0.295,0.342 and 0.416,respectively;P<0.05).Spearman correlation analysis showed that the serum level of HE4 in patients with CKD was positively correlated with CKD staging(rs=0.497,P<0.05).ROC curve analysis showed that the serum levels of HE4,BUN,Scr,UA and CysC in patients with CKD all had values in predicting renal dysfunction,and as for HE4,the area under the curve,sensitivity and specificity were better than BUN,Scr,UA and CysC.Conclusions The serum level of HE4 was elevated in patients with CKD,and was gradually increased with the staging of patients,which could be used as adjuvant diagnostic marker for early detection of renal dysfunction.
Chronic kidney disease;HE4;Staging;Renal dysfunction
陕西省科学技术研究发展计划项目(2011K12-69)
10.3969/j.issn.1009-6469.2016.11.019
2016-06-20,
2016-10-09)