腹腔镜与开腹胆总管取石一期缝合的临床比较
2017-01-04潘成文吴育连
潘成文 吴育连
(浙江大学医学院附属第二医院外二科,杭州 310003)
·临床研究·
腹腔镜与开腹胆总管取石一期缝合的临床比较
潘成文 吴育连*
(浙江大学医学院附属第二医院外二科,杭州 310003)
目的 探讨胆总管结石腹腔镜胆总管取石(laparoscopic common bile duct exploration,LCBDE)一期缝合的临床疗效。 方法 回顾性分析2010年1月~2014年12月322例胆总管取石一期缝合的临床资料,LCBDE组133例,开腹组189例,比较2组手术时间、术中出血量、术后6 h疼痛视觉模拟评分(visual analogue scale,VAS)、术后首次下床活动时间、住院时间、住院费用、术后并发症。 结果 2组手术均获成功,无术中并发症发生,LCBDE组无中转开腹。与开腹组相比,LCBDE组术中出血少[(33.9±18.3) ml vs. (72.6±38.5) ml,t=-10.755,P=0.000],术后疼痛轻[(3.8±1.6)分vs.(5.3±1.2)分,t=-9.610,P=0.000],术后首次下床活动早[(9.2±2.1)h vs.(14.3±2.7)h,t=-18.242,P=0.000],住院费用少[(3.03±0.50)万元vs.(3.50±0.68)万元,t=-6.864,P=0.000],住院时间短[(12.0±2.1) d vs.(15.0±4.4)d,t=-7.596,P=0.000],2组手术时间、并发症差异无显著性(P>0.05)。 结论 腹腔镜与开腹胆总管取石术后一期缝合治疗胆总管结石均安全、有效,LCBDE具有术后疼痛轻、住院时间短、住院费用低、恢复快等优点,值得临床推广应用。
胆总管结石; 腹腔镜; 一期缝合
胆总管结石易并发急性化脓性胆管炎、急性胰腺炎,对于十二指肠镜不能处理的胆总管结石,外科胆总管切开取石术是最常用的治疗方法。胆总管切开胆道探查取石T管引流是传统经典术式,包括开腹和腹腔镜胆总管切开取石(laparoscopic common bile duct exploration,LCBDE)。对术中证实胆管结石已经取净的患者,胆总管切开取石术后胆总管一期缝合的报道越来越多。2010年1月~2014年12月,我院行322例胆总管切开取石一期缝合,其中LCBDE 133例,开腹手术189例,术后均恢复良好,未出现严重并发症,现报道如下。
1 临床资料与方法
1.1 一般资料
病例选择标准:术前经外科与十二指肠镜内镜医生讨论,不适合或无法行ERCP十二指肠镜下一期取净结石或ERCP失败,行外科手术治疗;术前常规B超、CT或MRCP检查提示胆总管直径>8 mm,无肝内胆管结石,胆总管下端无狭窄,排除胆道恶性肿瘤、肝硬化,无严重合并症,符合胆管一期缝合标准。
共322例胆总管切开取石一期缝合,主诉腹痛168例,发热106例,黄疸160例,无症状113例。按不同术者的习惯,行腹腔镜手术133例(LCBDE组),开腹手术189例(开腹组)。术前常规B超、CT或MRCP检查,明确为肝外胆管结石,244例合并胆囊结石。LCBDE组平均年龄比开腹组小3岁(P=0.035),无临床意义,其余一般资料2组差异无统计学意义(P>0.05),见表1。
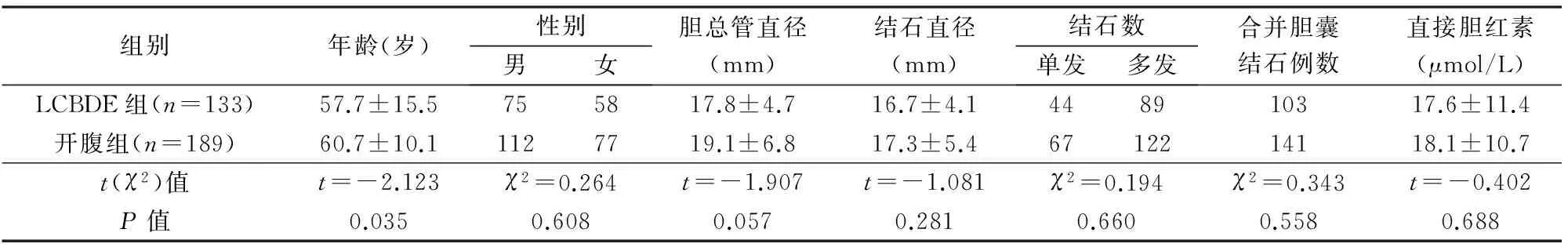
表1 2组一般资料比较
1.2 方法
1.2.1 LCBDE组 全身麻醉,平卧位,头高足低左倾30°,按四孔法胆囊切除的方式置放trocar。建立气腹,探查腹腔,如未发现其他病变,解剖胆囊三角,分离胆囊动脉用Hem-o-lok夹闭、离断,分离出胆囊管用Hem-o-lok夹闭,暂不离断。根据胆囊局部情况采用顺行或逆行分离胆囊,胆囊床彻底止血,牵拉胆囊底部使胆总管充分暴露,穿刺针穿刺明确胆总管,剪刀在胆总管前壁纵行切开1~1.5 cm,先常规吸引器头端连接一段长约8 cm的普通输液皮管,将吸引器头端皮管自剑突下主操作孔置入胆总管内,50 ml注射器装满生理盐水自吸引器端进行冲洗,充分冲洗后胆道镜取石篮取出胆总管结石,再次胆道镜检查肝内外胆管均通畅,胆道镜见到十二指肠乳头开闭,胆道无残石及狭窄后,用4-0或者5-0可吸收缝线间断缝合胆总管切口,针距2~3 mm,边距1 mm。术中均未行胆道造影。切除胆囊,将胆囊放入标本袋自脐上切口取出。常规Winslow孔处放置腹腔引流管1根,自右下操作孔引出。
1.2.2 开腹组 全身麻醉,右肋缘下斜切口,行胆囊逆行或顺行切除,穿刺针穿刺明确胆总管,在胆总管前壁纵行切开1~1.5 cm,50 ml注射器装满生理盐水行胆总管内冲洗,置入胆道镜,取石篮取出胆总管结石,胆道镜探查胆道通畅,无残留结石及胆总管狭窄,用4-0或者5-0 Prolene线间断缝合或连续缝合。常规Winslow孔处放置腹腔引流管1根,自切口右侧引出。
1.3 观察指标
从病历中提取以下数据:手术时间,术中出血量,首次下床活动时间,术后疼痛评分,总住院时间,住院费用,术后并发症包括胆漏、胆道狭窄、切口感染、结石残留率及结石复发率。术后6 h护士记录患者的疼痛视觉模拟评分(visual analogue scale,VAS)(0为不痛,10为最痛)。术后切口感染的判定:术后切口局部红、肿、热、疼痛和压痛,有脓性分泌物,伴或者不伴有发热症状。胆漏的判断:术后腹腔引流,单次胆汁样液体超过100 ml,或连续3天有胆汁流出。术后定期电话及门诊随访,术后2个月常规B超检查了解有无结石残留,2个月后对于有腹痛、黄疸等症状者行CT或MRCP检查了解有无结石复发及胆管狭窄。结石残留判定:术后2个月常规复查B超发现肝外胆管结石;未来院随访患者1年内发现的结石。结石复发判定:术后2个月常规复查B超未发现结石,以后检查发现的肝外胆管结石;未来院随访患者1年以上发现的结石。
1.4 统计学处理
2 结果
2组手术均获成功,无术中并发症发生,LCBDE组无中转开腹。2组观察指标比较见表2。与开腹组相比,LCBDE组术中出血少,术后疼痛轻,术后首次下床活动早,住院费用少,住院时间短(P<0.05),2组手术时间、并发症差异无显著性(P>0.05)。LCBDE组胆漏7例,腹腔引流5~18d自愈;开腹组11例胆漏,10例经腹腔引流6~20d自愈,1例引流量较多,术后第3天行内镜下鼻胆管引流,腹腔引流管引流液逐渐减少,10天后拔除腹腔引流管,术后1个月拔除鼻胆管。切口感染2组共8例,经切口换药6~12天愈合。2组随访2~15个月,均无胆道狭窄和结石残留。6例结石复发均随访12个月以上发现,结石直径均<1cm,均ERCP后取石。
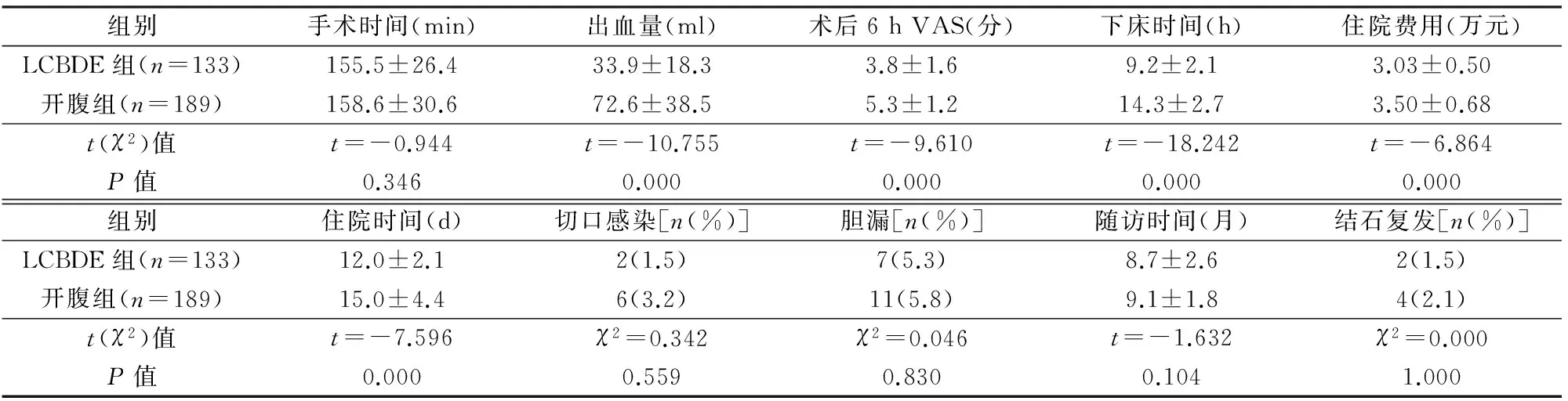
表2 2组观察指标比较
3 讨论
胆总管探查术自1890年瑞士Ludwig Courvossier首创并应用于临床[1],已经成为胆道外科常用的手术方法之一。传统的胆总管探查术常规行T管引流,影响患者生活质量[2],拔除T管后可能出现胆漏[3]等。随着肝胆外科及微创外科的发展,更多学者在胆总管取石后行胆总管一期缝合[4]。Ahmed等[5]报道,胆总管切开取石后一期缝合的胆道并发症低于T管引流组,术中需检查证实无残余结石。腹腔镜胆总管探查一期缝合术后胆漏及胆管狭窄的发生率并不高。Decker等[6]统计100例腹腔镜胆总管切开取石一期缝合,术后胆漏3例,未出现胆管狭窄。
胆总管结石取石后一期缝合的主要适应证为:①术前彩超、CT或MRCP检查未见胆管狭窄,肝内胆管无结石;②胆总管直径超过0.8 cm;③术中胆道镜探查确定胆总管和肝总管结石已取净;④胆总管下端通畅无狭窄,胆管炎症、水肿不严重;⑤无严重肝硬化等基础疾病。缝合的操作要点是:选择尽量细的无损伤线缝合,减少对胆管壁的切割。开腹手术我们常规选用4-0或5-0 Prolene线间断缝合或连续缝合,因为Prolene线对于胆管壁的切割损伤相对小,如胆总管较细,甚至可采用7-0 Prolene线缝合。因为Polene线不利于腔镜下操作,LCBDE胆总管缝合我们多采用4-0或5-0可吸收缝线(可吸收缝线腔镜下更容易操作),连续或间断缝合。针距2~3 mm为宜,边距1 mm左右,打结松紧适宜。应减少电刀的不正确使用,避免胆管壁热灼伤。缝合完毕后用纱布条轻沾以明确是否有胆汁渗出。LCBDE一期缝合对腹腔镜操作技术要求高,操作需轻柔,精准,腔镜下打结松紧适宜。Yokoyama等[7]报道腹腔镜胆总管缝合采用单向倒刺线缝合安全、有效,节省缝合时间。
本研究LCBDE组手术采用4个小切口,患者术后疼痛感明显减轻,术后首次下床活动较开腹组早。住院费用腹腔镜组较开腹组少,主要与住院时间短以及腹腔镜术后使用抗生素等药物时间短等有关。LCBDE一期缝合具有创伤小、患者恢复快、疼痛感轻、住院时间短等优点,甚至适用于有腹部手术史者[8]。腹腔镜胆道缝合创伤相对小,可降低患者的免疫抑制[9]。随着微创外科的发展,LCBDE手术不但在成人方面,甚至在儿科方面也是可行的[10],也同样适合于老年人[11],对符合适应证的患者可以作为替代T管引流的术式[12]。Yi等[13]报道对于部分LCBDE一期缝合的长期疗效评估也是安全有效的。本研究术后随访2~15个月,复查B超、CT或MRCP未发现残余结石及胆管狭窄,结石复发率1.9%(6/322),长期结果尚待随访。
本研究术后并发症主要为胆漏,LCBDE组7例,考虑与早期腔镜下缝合技巧有关。Rossi等[14]报道胆道手术后胆漏发生率为0.8%~12%,胆总管直径和胆总管结石清除是胆漏的风险因素,另外,操作不熟练导致缝合时反复进针、胆管壁较薄弱、严重胆管炎症导致胆管壁容易被切割以及患者全身情况都有关系。Lee等[15]报道LCBDE采用V-loc线一期缝合,同时置入胆道支架,明显减少术后并发症。腹腔镜外科医生技术熟练,患者经过仔细选择,术后胆漏发生率相对降低[16]。为预防胆漏发生,我们认为应做到以下几点:①胆道镜取石时动作轻柔,避免胆管黏膜损伤水肿,以免术后胆道压力增高引起胆漏;②缝合技巧,开放手术缝合建议用Prolene线,腔镜下选择可吸收线,胆管壁的缝合选用较细的针线,进行黏膜对黏膜的细致缝合,缝合完毕以生理盐水冲洗无胆汁渗出,结束手术前再次冲洗确认无胆汁渗出;③胆道镜检查确保结石取净,必要时术中胆道造影或腹腔镜超声检查进一步证实;④常规术中放置腹腔引流管;⑤熟练的操作技术及选择合适的病人也非常重要。
综上所述,腹腔镜和开腹胆总管切开取石一期缝合都是治疗胆总管结石安全、有效的方法,LCBDE一期缝合具有创伤小、恢复快、治疗费用低等优点,同时要严格把握适应证,术中做到精准与熟练操作。
1 许卓明,甄作均,苏树英,等.腹腔镜胆总管切开术:T管引流还是一期缝合.中国内镜杂志,2007,13(4):401-404.
2 Zhang WJ,Xu GF,Wu GZ,et al.Laparoscopic exploration of common bile duct with primary closure versus T-tube drainage:a randomized clinical trial.J Surg Res,2009,157(1):e1-5.
3 Haq A,Morris J,Goddard C,et al.Delayed cholangitis resulting from a retained T-tube fragment encased within a stone:a rare complication.Surg Endosc,2002,16(4):714.
4 Khaled YS,Malde DJ,de Souza C,et al.Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis.Surg Endosc,2013,27(11):4164-4170.
5 Ahmed I,Pradhan C,Beckingham IJ,et al.Is a T-tube necessary after common bile duct exploration?World J Surg,2008,32(7):1485-1488.
6 Decker G,Borie F,Millat B,et al.One hundred laparoscopic choledochotomies with primary closure of the common bile duct.Surg Endosc,2003,17(1):12-18.
7 Yokoyama K,Tanigawa N,Ogata A,et al.Laparoscopic technique and initial experiences of coledocholithotomy closure with knotless unidirectional barbed sutures after surgery for biliary stone disease.Surg Laparosc Endosc Percutan Tech,2015,25(4):e129-133.
8 Liang H,Zhang C,Zhang H.Study on suture of patients with history of abdominal surgery after laparoscopic choledocholithotomy.Pak J Pharm Sci,2015,28(6 Suppl):2285-2289.
9 Wang C,Wang Q,Sun D,et al.Immunogenic alteration in laparoscopic common bile duct exploration.J Surg Res,2014,187(1):302-309.
10 Lau BJ,Sydorak RM,Shaul DB.Laparoscopic techniques for safe and successful removal of common bile duct stones in pediatric patients.J Laparoendosc Adv Surg Tech A,2014,24(5):362-365.
11 Wang B,Ding YM,Nie YG,et al.The clinical evaluation of laparoscopic transcystic duct common bile duct exploration in elderly choledocholithiasis.Hepatogastroenterology,2014, 61(132):892-896.
12 Dong ZT,Wu GZ,Luo KL,et al.Primary closure after laparoscopic common bile duct exploration versus T-tube.J Surg Res,2014,189(2):249-254.
13 Yi HJ,Hong G,Min SK,et al.Long-term outcome of primary closure after laparoscopic common bile duct exploration combined with choledochoscopy.Surg Laparosc Endosc Percutan Tech,2015,25(3):250-253.
14 Rossi P,Servili S,Contine A,et al.Bile leak from the hepatic bed after laparoscopic cholecystectomy.Chir Ital,2002,54(4):507-509.
15 Lee JS,Yoon YC.Laparoscopic common bile duct exploration using V-Loc suture with insertion of endobiliary stent.Surg Endosc,2015,Aug 27. [Epub ahead of print]
16 Hua J,Lin S,Qian D,et al.Primary closure and rate of bile leak following laparoscopic common bile duct exploration via choledochotomy.Dig Surg,2015,32(1):1-8.
(修回日期:2016-04-08)
(责任编辑:王惠群)
【编者按】 胆总管结石胆总管切开取石后胆管一期缝合还是置放T管引流已有很多报告,有成功的经验,也有值得吸取的教训。关键是胆漏的发生,一旦发生往往造成严重后果,有的甚至需要多次手术。本文无论开腹组还是腹腔镜组,胆漏发生率都较高(>5%),远远超过胆道手术并发症胆漏发生率0.1%~0.5%,其原因和教训值得深究。本文18例幸好均经持续引流得到缓解,应引以为戒。胆总管一期缝合的病例选择非常重要,术中证实胆道结石完全取净非常关键,胆道镜对2级肝内胆管的观察有局限性,术中造影十分必要,可避免残留结石造成胆漏。对胆道结石残余与复发的界定目前尚无统一意见。Thompson、Saharia等提出在胆道取石2年内再出现的结石为残余结石,2年后出现的结石为复发性结石[1]。而国内黄志强[2]、石景森[3]等均以3年为界。再生的结石是手术后3年内再形成的结石。(再生结石的条件是:①前次手术后T管造影未发现结石;②再次手术与前次手术发现的结石性质、部位有所不同;③前次手术后3年内无症状)。梁力建等[4]提出术后1年以内发现结石者为残余结石,1年或1年以上者为复发结石。残余结石与结石再生(复发)是两个不同的概念,残余结石与手术有关,而结石再生(复发)与患者体质有关。本文作者以术后2个月为界缺乏文献依据。刊登此文,供同道交流。
参考文献
1 Saharia PC,Zuifema GD,Cameron JL.Primary common duct stones.Ann Surg,1977,185(5):598-604
2 黄志强,主编.当代胆道外科学.上海:上海科技文献出版社,1998.437.
3 石景森,王炳煌,主编.胆道基础与临床.北京:人民卫生出版社,2003.523.
4 梁力建,韩雨生.肝胆管残余结石的诊断方法及治疗选择.中国实用外科杂志,2000,20(9):521-523.
执行主编:傅贤波
Comparative Study Between Laparoscopic and Open Common Bile Duct Exploration with Primary Closure
PanChengwen,WuYulian.
SecondDepartmentofSurgery,SecondAffiliatedHospital,ZhejiangUniversitySchoolofMedicine,Hangzhou310003,China
WuYulian,E-mail:wuyulian@medmail.com.cn
Objective To discuss the clinical efficacy of primary suture following laparoscopic common bile duct exploration (LCBDE) for choledocholithiasis. Methods Clinical data of 322 patients with common bile duct stones undergoing primary suture from January 2010 to December 2014 were retrospectively analyzed. There were 133 patients receiving laparoscopic common bile duct exploration (LCBDE group) and 189 patients receiving open operation (open group). The operative time, blood loss, visual analogue scale (VAS) of pain 6 h after surgery, postoperative ambulation time, hospitalization time, hospitalization expenses, postoperative complication rate of the two groups were observed and compared. Results The procedure was successfully accomplished in all the patients in both groups. No complications occurred in the process of surgery. No conversion to open operation was required in the LCBDE group. The blood loss in the LCBDE group [(33.9±18.3) ml] was less than that in the open group [(72.6±38.5) ml,t=-10.755,P=0.000). The pain VAS scores were lower in the LCBDE group [(3.8±1.6) points] than in the open group [(5.3±1.2) points,t=-9.610,P=0.000]. The LCBDE group showed earlier out-of-bed activity [(9.2±2.1) hours] than the open group [(14.3±2.7) hours,t=-18.242,P=0.000]. The hospitalization expenses in the LCBDE group [(3.03±0.50)×104yuan] was lower than that in the open group [(3.50±0.68)×104yuan,t=-6.864,P=0.000]. The postoperative hospital stay in the LCBDE group [(12.0±2.1) days] was shorter than that in the open group [(15.0±4.4) days,t=-7.596,P=0.000]. There was no significant difference between the two groups in the operation time and postoperative complications rates (P>0.05). Conclusions LCBDE and the open choledocholithotomy with primary suture of the common bile duct are both effective and safe procedures for common bile duct stones. As compared with the open operation, LCBDE with primary suture has smaller incision, less pain, less hospitalization costs and quicker recovery, being more worthy of clinical application.
Choledocholithiasis; Laparoscope; Primary closure
A
1009-6604(2016)06-0518-04
10.3969/j.issn.1009-6604.2016.06.011
2016-03-07)
*通讯作者,E-mail:wuyulian@medmail.com.cn