房室交界区不应期内房性早搏刺激在预激综合征消融术中的应用
2016-10-25许环亲吴飞玉郭照军陈武刘先霞何建桂
许环亲 吴飞玉 郭照军 陈武 刘先霞 何建桂
·临床研究论著·
房室交界区不应期内房性早搏刺激在预激综合征消融术中的应用
许环亲吴飞玉郭照军陈武刘先霞何建桂
目的探讨房室交界区不应期内的房性早搏(房早)刺激在指导预激综合征靶点定位及消融的临床应用价值。方法50例预激综合征患者按是否使用房早刺激方法指导消融前传旁路,分为对照组和房早干预组。对照组20例(A型预激12例,B型预激8例),使用非房早刺激的常规术式消融前传旁路。房早干预组30例(A型预激16例,B型预激14例),使用房早刺激指导消融前传旁路,首先在窦性心律下,通过测量其RR间期后,在此基础上减去30 ms后作为房早的初始起搏间期,以5 ms逐步递减,观察体表QRS的预激成分,当达到预激最明显时,取此时的联律间期作为固定刺激频率,指导房早干预组前传旁路消融。比较2组一次性消融成功率、累计消融时间及累计射线量。结果房早干预组一次性消融成功率达80%,高于对照组的55%,2组比较差异有统计学意义(P=0.03)。房早干预组累计消融时间为(301.3±61.1)s,低于对照组[(358.5±115.5)s,P=0.03]。房早干预组累计射线量为(49.3±31.8)mGray,低于对照组[(101.2±78.5)mGray,P<0.01]。结论房室交界区不应期内房早刺激指导预激综合征导管消融具有一定临床价值,能有效缩短手术时间、降低射线暴露率及提高手术的成功率。
房室交界区不应期内的房性早搏;预激综合征;导管消融
Wolff-Parkinson-White syndrome; Catheter ablation
射频消融旁道是根治预激综合征并发严重心律失常的主要手段,影响消融成功率最重要因素是导管操作和旁道靶点图指标,尤其是右心室旁道消融成功率较低,因其窦律下AV融合性较差,靶点图特异性偏低,常常导致过多消融及长时间消融,甚至当V1导联预激不充分,临床诊断A、B型预激综合征亦经常混淆,但目前旁道术前诊断和定位仍较多依赖于体表心电图及术中导管操作比对,对预激充分性较差的旁道敏感性不高[1-2]。早搏刺激常用于心室起搏鉴别隐匿性房室旁路是否存在,但在房室交界区不应期内房早刺激较少用于预激不充分的房室旁路的临床治疗[3]。本研究旨在初步探讨在房室交界区不应期内房早刺激能否提高预激综合征靶点定位的准确性,并提高一次消融的成功率,减少消融所带来误损伤[4]。
对象与方法
一、 研究对象
连续入选2011年6月至2015年9月入住海南省农垦总医院心血管内科确诊为预激综合征且有射频消融手术意向的患者50例,进行前瞻性对照研究。按是否使用房早刺激方法指导消融预激综合征前传旁路,分为对照组和房早干预组。对照组使用非房早刺激的常规术式消融预激综合征前传旁路;房早干预组使用房室交界区不应期内房早刺激指导消融预激综合征前传旁路。首先根据体表心电图初步筛选出A型预激综合征和B型预激综合征患者,然后根据就诊顺序按(对照组∶房早干预组1∶1.5比例)进行分配。对照组20例,男女各10 例 ,年龄(32.5±8.3)岁;其中A型预激综合征男8例,女4例;B型预激综合征男4例,女4例。房早干预组30例,男16例,女14例, 年龄(39.1±10.9)岁;其中A型预激综合征男11例,女5例;B型预激综合征男5例,女9例。
每例患者均须签署知情同意书,行体表12导联同步心电图及超声心动图检查,排除器质性心脏病及室内传导阻滞,B型显性预激综合征患者体表心电图V1导联上均可见负向典型&波,A型显性预激综合征患者体表心电图V1导联上均可见正向典型&波。
二、 设备和方法
采用圣犹达多导电生理刺激仪EP-Maker。检查方法:受检者取仰卧位,平静呼吸,连接心电图,常规消毒铺巾后,分别经颈静脉放置CS电极及经股静脉放置高右房电极。记录刺激前V1导联QRS间期、&波成分,CS电极的AV间期及RR间期后。使用高右房电极进行房早电刺激,在初始RR间期基础上减去30 ms后作为程序刺激的初始起搏间期,以5 ms逐步递减,观察体表V1导联的QRS的预激成分,当达到预激最明显时的上阈时,取此时的联律间期作为固定起搏频率设定,此后每隔3次心跳,心房以此频率给予早搏刺激,再用消融电极标测预激成分充分前后靶位点的AV融合情况,同时与对照组对比其一次消融成功率、累计消融时间(至消融成功所用的时间)及累计射线的使用量(至消融成功所用的射线量)。如旁路不应期较交界区不应期短,则以旁路前传中断前一跳所给的房性早搏作为刺激条件。一次消融成功是指第一次标到靶位点,并尝试放电消融10 s后,验证旁路阻断。
三、 统计学处理
结 果
一、 房早干预组与对照组一次消融成功率比较
房早干预组一次性消融成功率高于对照组(P=0.03);对B型预激指导消融方面,房早干预组一次性消融成功率高于对照组(P=0.03),见表1。
二、 房早干预组与对照组累计消融时间比较
房早干预组累计消融时间短于对照组, 2组比较差异有统计学意义(P=0.03)。对于B型预激综合征患者,房早干预组累计消融时间短于对照组,差异有统计学意义(P=0.01)。见表2。
三、 房早干预组与对照组累计射线量比较
房早干预组累计射线量为低于对照组,2组比较差异亦有统计学意义(P<0.01)。对于B型预激综合征患者,房早干预组累计射线量使用低于对照组,差异有统计学意义(P=0.01)。见表3。
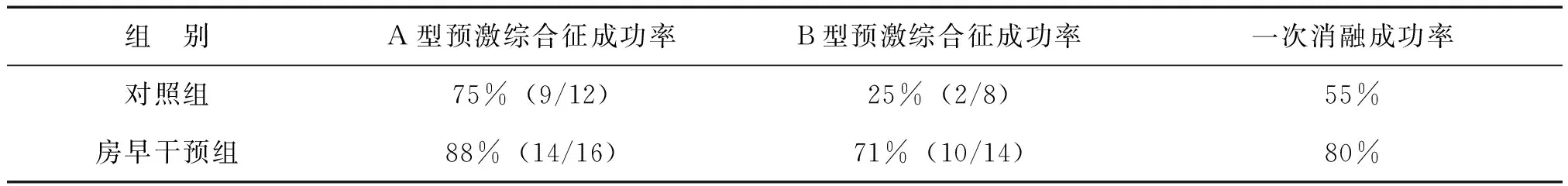
表1 房早干预组与对照组一次消融成功率比较

表2 房早干预组与对照组累计消融时间±s) s

表3 房早干预组与对照组累计射线量比较±s) mGray
讨 论
Spotnitz等[5]报道腺苷诱导消融术后休眠房室旁路传导的机制和临床意义及Caetano等[6]的报道心房起搏可诱发潜在的预激综合征等,提示适当阻断房室传导或在房室传导不应期内起搏,能充分引导旁路前传,导致预激更充分,为本文提供了理论支持。
本文采用在房室交界区不应期内给予房早起搏指导预激综合征消融,结果显示,此方法对临床消融成功率偏低的B型预激综合征具有一定指导意义,能有效缩短手术时间、降低射线暴露及提高手术成功率,且能明显降低术中对导管连续性标测的干扰。
本方法简单易行,与Delelis等[7]报道的通过术前二维B超速度向量成像对预激综合征旁道定位及Nishida等[8]报道的经非接触三维标测系统指导消融B 型预激综合征具有异曲同工之处,但本法准确性高、无额外增加手术费用,且可在术中指导精细定位,避免了术中尝试性盲目消融导致的瓣膜损伤[9]。
本研究提示,心房起搏位点如离旁路越近,此法成功率越高,但对旁路不应期明显较交界区不应期长患者的消融指导意义,此法具有一定局限性。且本研究因目前入组的病例数较少,暂不能区分对不同部位的旁路其指导意义的区别,有待进一步的跟踪研究探讨。
[1]王业松,孙爱娇.心脏导管射频消融术. 新医学,2009,40(1):50-52.
[2]Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, Estes NA 3rd, Field ME, Goldberger ZD, Hammill SC, Indik JH, Lindsay BD, Olshansky B, Russo AM, Shen WK, Tracy CM, Al-Khatib SM. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol,2016,67(13):e27-e115.
[3]张鹏,吴冬燕,李琼,卢凤民,许静. 希氏束不应期内心室早搏刺激鉴别隐匿性间隔房室旁道与慢-快型房室结折返性心动过速. 中国实用内科杂志,2014,34(S1):75-77.
[4]张澍.心血管疾病介入诊疗技术培训教材(心律失常分册). 2版.卫生部办公厅,2011: 73-74.
[5]Spotnitz MD, Markowitz SM,Liu CF, Thomas G, Ip JE, Liez J, Lerman BB, Cheung JW. Mechanisms and clinical significance of adenosine-induced dormant accessory pathway conduction after catheter ablation.Circ Arrhythm Electrophysiol,2014,7(6):1136-1143.
[6]Caetano F, Barra S, Cavaco D. Wolff-Parkinson-White syndrome unmasked by atrial pacing in a patient with cardiac sarcoidosis. Europace, 2014,16(12):1713.
[7]Delelis F, Lacroix D, Richardson M, Klug D, Kouakam C, Brigadeau F, Guyomar Y, Graux P, Kacet S, Gautier C, Ennezat PV, Marechaux S.Two-dimensional speckle-tracking echocardiography for atrioventricular accessory pathways persistent ventricular pre-excitation despite successful radiofrequency ablation. Eur He-art J Cardiovasc Imaging, 2012, 13(10):840-848.
[8]Nishida T, Nakajima T, Kaitani K, Takitsume A, Soeda T, Okayama S, Somekawa S, Takeda Y, Ishigami K, Kawata H, Kawakami R, Horii M, Uemura S, Saito Y.Non-contact mapping system accurately localizes right-sided accessory pathways in type B Wolff-Parkinson-White syndrome.Europace,2012,14(5):752-760.
[9]Penaranda Canal JG, Enriquez-Sarano M, Asirvatham SJ, Munger TM, Friedman PA, Suri RM. Mitral valve injury after radiofrequency ablation for Wolff-Parkinson-White syndrome. Circulation,2013,127(25):2551-2552.
(本文编辑:杨江瑜)
Application of atrial premature of atrioventricular junction within refractory period in ablation for patients with Wolff-Parkinson-White syndrome
XuHuanqin,WuFeiyu,GuoZhaojun,ChenWu,LiuXianxia,HeJiangui.
DepartmentofCardiology,HainanProvincialNongkenGeneralHospital,Haikou570311,China
Correspondingauthor,HeJiangui,E-mail:hejiangui@163.com
ObjectiveTo assess the clinical efficacy of atrial premature stimulation of atrioventricular junction within refractory period on the target locating and ablation in patients with Wolff-Parkinson-White syndrome (W-P-W). MethodsFifty patients with overt pre-excitation syndrome were divided into the control (n=20) and the atrial premature groups (n=30) according to whether atrial premature stimulation was delivered to guide the ablation. In the control group, 20 patients (12 cases of type A, 8 cases of type B) underwent conventional ablation via anterior accessory pathway. In the atrial premature group, 30 patients (16 cases of type A, 14 cases of type B) received atrial premature stimulation-guided ablation via anterior accessory pathway. Under the condition of sinus rhythm, R-R interval minus 30 ms was regarded as the initial pacing interval of atrial premature stimulation. As initial pacing interval was reduced by 5 ms, the pre-excitation component of the surface QRS was observed. The interval with most significant overt pre-excitation component was considered as the fixed stimulus frequency to guide the ablation via anterior accessory pathway in W-P-W patients. The success rate of the first ablation, the accumulative ablation time and the accumulative radiation dose were statistically compared between two groups. ResultsThe success rate of the first ablation in the atrial premature group was 80%, significantly higher compared with 50% in the control group (P=0.03). The accumulative ablation time in the atrial premature group was (301.3±61.1)s, considerably shorter than (358.5±115.5) s in the control group (P=0.03). The cumulative radiation dose in the atrial premature group was (49.3±31.8) mGray, significantly lower compared with (101.2±78.5) mGray in the control group (P<0.01). ConclusionsCatheter ablation guided by atrial premature stimulation of atrioventricular junction within refractory period is of certain clinical significance, which shortens operation time, reduces radiation exposure rate and improves surgical success rate.
Atrial premature of atrioventricular junction within refractory period;
10.3969/j.issn.0253-9802.2016.09.013
570311 海口,海南省农垦总医院心血管内科(许环亲,吴飞玉,郭照军,陈武,刘先霞);510080 广州,中山大学附属第一医院心血管内科(何建桂)
,何建桂,E-mail:hejiangui@163.com
2016-04-06)
