膀胱癌全腹膜外回肠膀胱术术式改良探讨
2016-10-22汪小军赵星星王佳琦李海霞
汪小军,李 鑫,李 瑾,崔 鹏,赵星星,胡 琦,王佳琦,李海霞
膀胱癌全腹膜外回肠膀胱术术式改良探讨
汪小军1,李鑫1,李瑾2,崔鹏1,赵星星1,胡琦1,王佳琦3,李海霞1
目的探讨侧腹膜小切口回肠拖出法在全腹膜外回肠膀胱术中的应用。方法选择2011-01至2014-12我科室膀胱癌患者57例。入选标准为病理确诊尿路上皮癌,临床分期为T2b~T4a,预期寿命>1年患者。其中常规手术组27例,侧腹膜切口采用传统大切口手术方法;改良手术组30例,侧腹膜切口采用侧腹膜小切口回肠拖出法。对比两组关闭侧腹膜针数、术中耗时、术中出血量、游离腹膜面积、侧腹膜切口长度、术后患者排气时间、术后出现内疝及早期肠梗阻原因,术后回肠膀胱血运及坏死情况。结果两组术后排气时间分别(72±6)、(72±10)h,两组间比较差异无统计学意义。改良组与常规组术中侧腹膜分别缝针(5±2)针、(12±2)针,耗时分别为(15±5)min、(25±5)min,出血量分别为(10±5)ml、(30±8)ml,腹膜游离面积分别为(20±5)cm2、(45±5)cm2,侧腹膜切口长度分别为(3±1)cm、(12±2)cm,组间比较差异均有统计学意义(P<0.05)。结论通过改良可明显缩短手术时间,减少手术造成腹膜损失,减少出血量,明显降低手术难度,且不增加手术并发症。
侧腹膜小切口回肠拖出法;全腹膜外回肠膀胱术;膀胱癌
膀胱肿瘤是泌尿系统常见的肿瘤, 发达国家或地区发病率较高,在国内发病率呈上升趋势。随着疾病发展,最终多会选择行全膀胱切除及尿流改道[1]。回肠膀胱术(Bricker膀胱)自1950年Bricker报道以来,至今仍为成人永久性尿流改道的常用术式之一[2]。自2011年以来,我们以上述改良方法完成全膀胱切除+回肠膀胱术30余例,术后恢复良好。
1 对象与方法
1.1对象选择2013-01至2014-12我科膀胱癌患者30例,作为改良手术组,男19例,女11例,年龄31~67岁,中位年龄53.0岁。选择2011-01至2012-12我科膀胱癌患者27例,作为常规手术组,男17例,女10例,年龄30~69岁,中位年龄53.5岁。入选标准为病理确诊尿路上皮癌,临床分期为T2b~T4a,预期寿命>1年患者。
1.2手术方法两组手术均由同一手术组完成。改良手术组:回盲部内下方侧腹膜做2~3 cm小切口,将回肠膀胱及其系膜拉出到右侧侧腹膜外;将侧腹膜小切口边缘与系膜根部间断缝合关闭此切口;在腹膜外将双侧输尿管与回肠膀胱做吻合(图1)。常规手术组:左侧腹膜横行切开至回盲部下方,将回肠膀胱拉出后,再将腹膜缝合;以1-0丝线间断缝合关闭侧腹膜,同时还需缝合关闭腹膜与回肠膀胱系膜裂孔[3]。
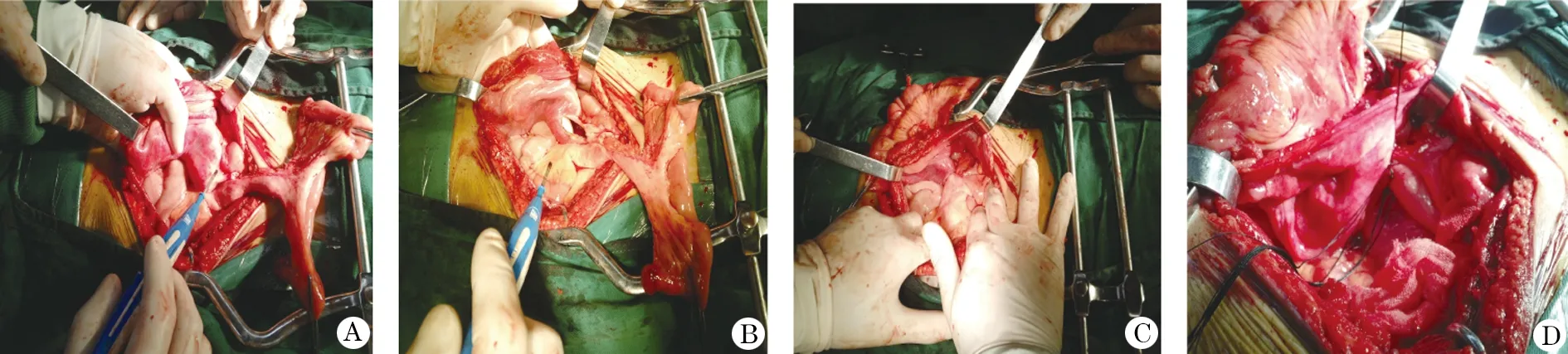
图1 全腹膜外回肠膀胱术中侧腹膜小切口回肠拖出法
1.3观察指标术中观察并记录缝制关闭侧腹膜针数、术中耗时、术中出血量、游离腹膜面积、侧腹膜切口长度、术后患者排气时间、术后出现内疝及早期肠梗阻原因,术后回肠膀胱血运及坏死与否。

2 结 果
两组手术均能顺利完成,术后恢复良好,未出现回肠膀胱血运不良及坏死发生,未发生内疝及早期肠梗阻。两组术后排气时间比较,差异无统计学意义;但改良手术组与常规手术组术中侧腹膜缝针数、耗时、出血量、腹膜游离面积、侧腹膜切口长度等指标比较差异均有统计学意义(P<0.01,表1)。

表1 全腹膜外回肠膀胱术术式改良组与常规组的比较 ±s)
3 讨 论
目前,肌层浸润性膀胱癌的标准治疗为根治性膀胱切除术,可以有效提高患者生存率,降低局部复发及远处转移率[4,5]。膀胱全切改变了原有的排尿线路,尿流改道手术随之而出。随着腔镜技术的不断发展与成熟,腹腔镜手术与机器人辅助的腹腔镜手术也已应用于多种尿流改道术[6],临床多采用腹腔镜下全膀胱切除术后腹腔外完成尿流改道[7]。近年来,出现了原位新膀胱术,同样存在诸如吻合口狭窄、尿道残端肿瘤复发后再次手术治疗困难、术后尿潴留、尿失禁、肾积水等并发症。同时,受肿瘤生长部位影响,也不是所有患者适宜原位新膀胱术。因此,尿流改道术宜根据患者及疾病具体情况而采取合适的方案,如出现肿瘤远处转移、频发血尿、肿瘤侵犯输尿管导致肾积水、肾功能不全时,就可能仅行输尿管皮肤造口,甚至连膀胱都可以无需切除。
回肠膀胱术(Bricker膀胱)自1950年Bricker报道以来,因其技术容易被掌握,且并发症发生率低,至今仍为成人永久性尿流改道的常用术式之一[2]。但因该方法将回肠膀胱末端及输尿管吻合口留置于腹腔内,所以,如果出现吻合口漏尿,尿液将直接排入腹腔肠管间,严重干扰肠道功能,引发腹腔感染、肠粘连、肠梗阻等[8]。随着技术的日臻完善,将回肠膀胱末端及输尿管吻合口位置改为置于腹膜外,即部分腹膜外回肠膀胱术,则显著降低了因术后漏尿、感染等对腹腔肠道的影响。具体方法是,切开右侧腹膜,将回肠膀胱近端及输尿管固定于腹膜外,然后缝合关闭侧腹膜切口[9]。目前,回肠膀胱术大多采用此做法。
1984年,我院李树森主任又将其改良为全腹膜外回肠膀胱术,整个回肠膀胱和输尿管吻合口均置
于腹膜外[10]。近年临床研究表明,侧腹膜大切口腹膜外回肠膀胱虽然可以减少对肠道功能的影响,但需要将右侧腹膜大面积游离切开,腹膜损失较多,易出血,耗时长,操作复杂。对此,我们对该手术方法进一步改良,选择回盲部内下方侧腹膜做2~3 cm小切口,将回肠膀胱及其系膜拉出到右侧侧腹膜外。将侧腹膜小切口边缘与系膜根部间断缝合关闭此切口。在腹膜外将双侧输尿管与回肠膀胱做吻合。本研究发现,不论是术中侧腹膜缝针数、耗时、出血量、腹膜游离面积,还是侧腹膜切口长度,改良手术组都明显优于常规手术组。改良手术组保留了侧腹膜的完整性,而且牵出回肠膀胱后同样不会出现回肠膀胱缺血坏死,同样达到全腹膜外回肠膀胱的要求。
综上所述,全腹膜外回肠膀胱术采用腹膜小切口回肠拖出法更安全实用。通过改良后可明显缩短手术时间,减少手术造成腹膜损失,减少出血量,降低手术难度,且不增加手术并发症。
[1]许存孝,赵升田. 临床泌尿外科学[M]. 济南:山东科学技术出版社,2007:158-162.
[2]吴阶平. 吴阶平泌尿外科学[M]. 济南: 山东科学技术出版社, 2001:94.
[3]徐国华,李振华,张青. 泌尿外科手术要点图解[M].北京:中国医药科技出版社,2013: 183-186.
[4]Stein J P, Quek M L, Skinner D G. Lymphadenectomy for invasive bladder cancer: I. historical perspective and contemporary rationale [J]. BJU Int, 2006,97(2):227-231.
[5]World Health Organization(WHO) Consensus Conference in Bladder Cancer, Hautmann R E, Abol-Enein H,etal. Urinary diversion[J]. Urology, 2007,69(1 Suppl):17-49.
[6]Huang J, Lin T, Liu H,etal. Laparoscopic radical cystectomy with orthotopic ileal neobladder for bladder cancer: oncologic results of 171 cases with a medina 3-year follow-up[J]. Eur Urol, 2008,54(1):442-449.
[7]陈光富,张旭,史立新,等. 机器人腹腔镜下根治术膀胱切除加尿流改道术的临床分析[J]. 中华泌尿外科杂志,2012,33(10):744-748.
[8]Pycha A, Comploj E, Martini T,etal. Comparison of complications in three incontinent urinary diversions [J]. Eur Urol, 2008,53(4):834-844.
[9]梅骅,陈凌武. 泌尿外科手术学[M].3版. 北京: 人民卫生出版社,2008: 358-360.
[10]李鑫,李树森, 李占文. 腹膜外回肠膀胱术[J]. 内蒙古医学杂志,2001, 33(6):521-522.
(2015-06-20收稿2015-12-20修回)
(责任编辑武建虎)
Modification of procedure of total extraperitoneal ileal conduit
WANG Xiaojun1, LI Xin1, LI Jin2,CUI Peng1, ZHAO Xingxing1, HU Qi1, WANG Jiaqi3, and LI Haixia1.
1.Department of Urology, Tumor Hospital of BaoTou city, Baotou 014030,China,2. Department of Breast Surgery, Tumor Hospital of BaoTou city, Baotou 014030,China,3.Department of Radiology, Tumor Hospital of BaoTou city, Baotou 014030,China
ObjectiveTo study the application of pulling out ileum from small lateral peritoneum incision in total extraperitoneal ileal conduit.Methods57 bladder cancer patients admitted from January 2011 to December 2014 in this department were recruited. The inclusion criteria included pathologically confirmed urothelial carcinoma, clinical stage T2b-T4a, and expected survival >1 year. 27 patients received conventional procedure, with traditional large incision applied during lateral peritoneum incision; 30 patients received modified procedure, with ileum dragging out through small lateral peritoneum incision. The differences between the two groups regarding numbers of stitches during lateral peritoneum incision suture, time consumed for the surgery, intraoperative blood loss, area of peritoneum isolated, lateral peritoneum incision length, the time to first post-operative anal exhaust, the reasons for post-operative internal hernia and early intestinal obstruction, as well as post-operative blood supply for ileal conduit and whether necrosis showed up.ResultsThe time to first post-operative anal exhaustion for the two group were (72±6) h and (72±10) h, respectively, and the difference was not statistically significant. For modified group and conventional group, the numbers of stitches applied during lateral peritoneum incision suture were (5±2) and (12±2), time consumed were (15±5) min and (25±5) min, blood loss were (10±5) ml and (30±8) ml, the area of peritoneum isolated were (20±5) cm2, and (45±5) cm2, and lateral peritoneum incision length were (3±1) cm and (12±2) cm, respectively. The differences between the two groups were statistically significant (P<0.05).ConclusionsModified procedure can shorten the time consumed during procedure, reduce peritoneum loss and blood loss, as well as simplify procedure without more procedure-induced complications.
dragging out ileal by lateral extra-peritoneal incision; total extraperitoneal ileal conduit; bladder cancer
汪小军,本科学历,主治医师。
014030,包头市肿瘤医院:1.泌尿外科,2.乳腺外科,3.影像科
李鑫,E-mail:lixinbt@sina.com
R694
