DC-CIK细胞联合常规化疗治疗晚期非小细胞肺癌的临床有效性与安全性分析
2016-10-13李威威张海萍吴敏王林
李威威 张海萍 吴敏 王林
·论著·
DC-CIK细胞联合常规化疗治疗晚期非小细胞肺癌的临床有效性与安全性分析
李威威张海萍吴敏王林

非小细胞肺肿瘤;化疗;DC-CIK细胞;有效性;安全性
非小细胞肺癌(non-small cell lung cancer,NSCLC)是中老年人群呼吸系统较为常见的恶性肿瘤,晚期(临床分期[1]Ⅲ~Ⅳ期)患者手术治疗的效果并不理想[2],因此,寻找安全有效的内科疗法是肿瘤界众多医学同仁研究的热点。我院采用DC-CIK细胞联合常规化疗使晚期NSCLC患者获益明显,报告如下。
1 资料与方法
1.1一般资料选取2010年1月至2013年10月我院肿瘤科收治的晚期NSCLC患者81例,其中男58例,女33例;年龄41~73岁,平均年龄(52±14)岁。依据治疗方式不同,将行NP化疗联合DC-CIK细胞治疗者设为观察组(n=40),行NP化疗者设为对照组(n=41)。2组患者性别比、年龄、体力状态(KPS评分[3])、体重指数、病理类型、临床分期、病程、基础病、家族遗传史、既往治疗史等基线资料比较差异均无统计学意义(P>0.05),具有可比性。本研究经医院伦理委员会批准,患者及家属同意并签署知情同意书。见表1。
1.2选择标准
1.2.1纳入标准:①所有患者入院时满足《中国原发性肺癌诊疗规范·2015年版》[4],且经病理进一步确诊为NSCLC;②临床分期参照国际肺癌研究协会(IASLC)第7版《肺癌TNM分期》[1]确定为Ⅲ~Ⅳ期;③KPS评分不少于60分;④病例资料完善。
1.2.2排除标准:①诊断、病理类型或临床分期不明确者;②未完成4个周期NP方案化疗;③合并有心、肝、脑、肾等严重基础病;④合并其他NSCLC以外的其他肿瘤;⑤合并有感染性疾病、内分泌系统或免疫系统异常者;⑥哺乳及妊娠期女性;⑦近6个月免疫抑制剂或激素类药物持续服用者。

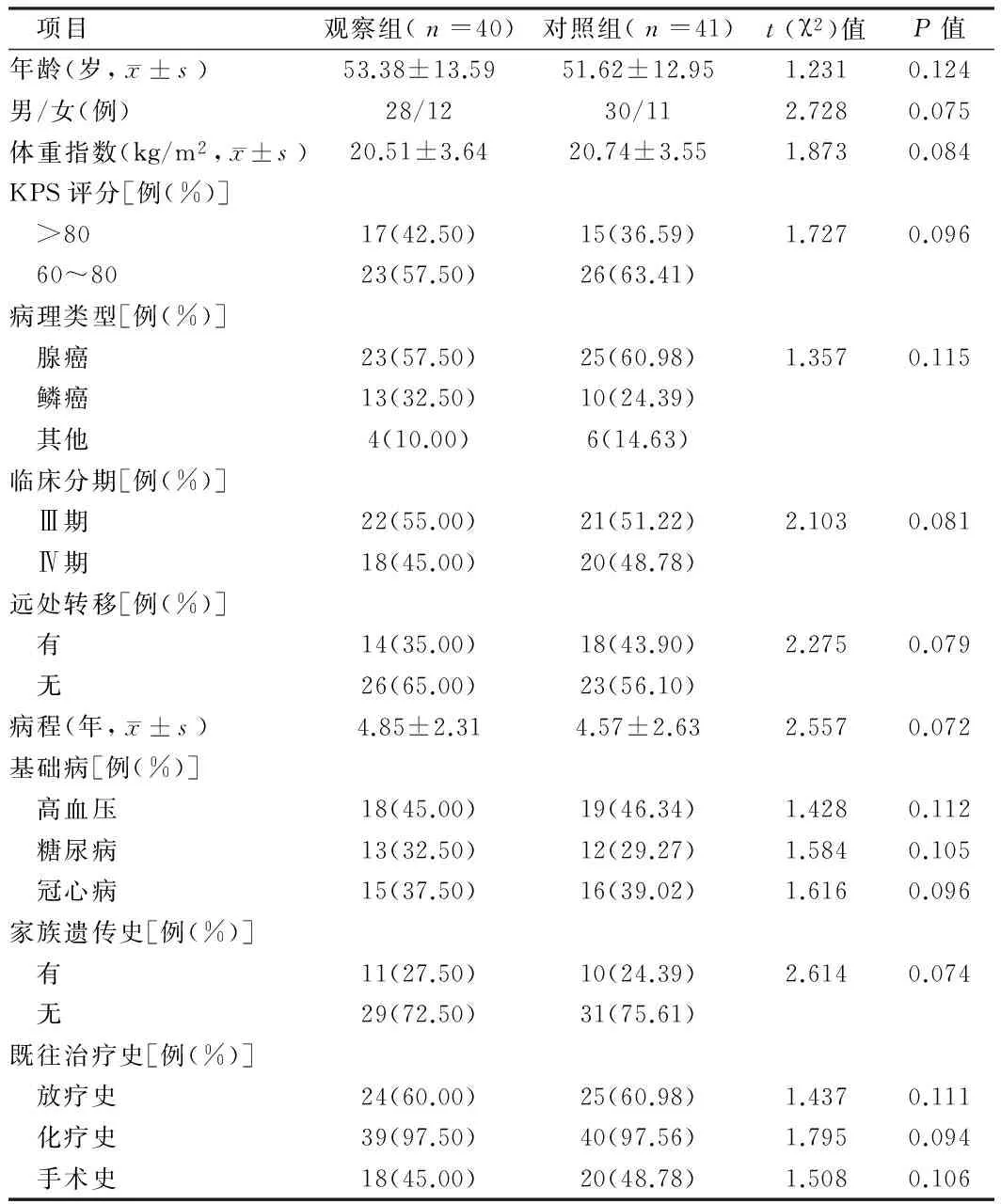
表1 2组患者基线资料情况

1.5疗效标准(1)临床疗效:结合患者治疗前后的影像学检查结果,依据实体瘤的疗效评价标准[6]对所有患者进行依次评定,其中,癌灶完全消除持续30 d者为完全缓解;最长径癌灶之和减少≥30%持续30 d者为部分缓解;最长径癌灶之和增加≥20%持续30 d者为进展;介于进展与部分缓解之间者为稳定;总有效率=完全缓解率+部分缓解率,疾病控制率=有效率+稳定率。(2)体力状态:参照Karnofsky评分法[3](KPS)评定并记录患者治疗前后体力状态,其中,改善:KPS总分增加>10分;恶化:KPS总分减少>10分;稳定:KPS总分增加或减少不超过10分;体力状态总提高率=改善率+稳定率。(3)不良反应评价:血细胞变化、胃肠道反应等不良反应的评定主要参考《WHO抗肿瘤药毒性急性与亚急性毒副反应分度标准》[7]。

2 结果
2.12组患者疗效比较总有效率观察组高于对照组,但差异无统计学意义(χ2=1.468,P=0.079);疾病控制率高于对照组(χ2=5.374,P=0.041)。见表2。
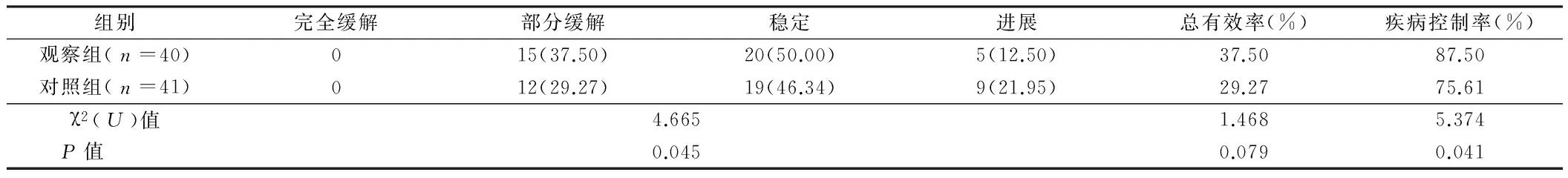
表2 2组患者疗效比较 例(%)
2.22组患者体力状态比较观察组患者体力状态总提高率高于对照组(χ2=10.957,P=0.016)。见表3。
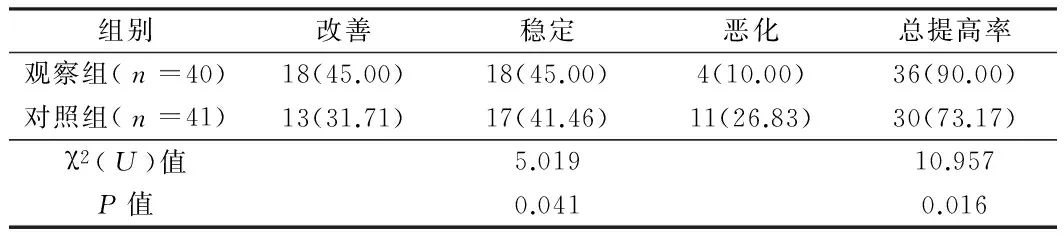
表3 2组患者体力状态比较 例(%)
2.3生存情况比较截止到随访日期,观察组40例患者,死亡30例,存活10例,其中位无瘤生存期7.5个月(95%CI:5.16~8.95),中位生存期14.5个月(95%CI:10.05~17.95);对照组41例患者,死亡35例,6例存活,其中位无瘤生存期4.5个月(95%CI:3.17~6.92),中位生存期11.5个月(95%CI:9.11~14.87);log-rank检验显示,观察组患者中位无瘤生存期长于对照组(χ2=6.557,P=0.038),中位生存期长于对照组,但差异无统计学意义(χ2=1.384,P=0.082)。2组患者生存曲线及无进展生存曲线见图1、2。


图1 2组患者生存曲线

图2 2组患者的生存曲线
2.52组患者不良反应比较观察组患者发热率高于对照组(χ2=6.549,P=0.032);2组患者白细胞降低、血小板降低、脱发、消化道反应、肝功能损害、肾功能损害等不良反应发生率比较,差异均无统计学意义(χ2=2.014,P=0.076;χ2=1.247,P=0.098;χ2=1.954,P=0.081;χ2=1.358,P=0.095;χ2=1.657,P=0.088;χ2=1.028,P=0.104)。2组患者不良反应轻微,给予对症处理后均得到控制。见表5。

表4 2组患者外周血T淋巴细胞阳性百分比比较 ±s

表5 2组患者不良反应发生情况比较 例
3 讨论
NSCLC起病隐匿,加之我国较低的医疗知识普及程度和健康宣教力度,不少患者确诊时已处于晚期,显著降低了手术治疗的意义。目前,运用较多的以规范化疗为中心的内科疗法虽能通过杀伤一定比例的肿瘤细胞来降低肿瘤负荷、缓解临床症状,但难以彻底清除微小病灶,且多数化疗对患者的免疫系统、血液系统等有着较多不利的影响[8]。因此,探求科学可靠的内科疗法有重要临床意义。


1蔡文科,石云.非小细胞肺癌分期技术的应用研究及第七版肺癌分期的解析.国际肿瘤学杂志,2013,40:523-526.
2Leora H.Advances in the treatment of non-small cell lung cancer.Journal of the National Comprehensive Cancer Network Jnccn,2014,12:764-767.
3Rades D,Dziggel L,Nagy V,et al.Erratum to “A new survival score for patients with brain metastases who received whole-brain radiotherapy (WBRT) alone” Radiother Oncol 108 (2013) 123-127.Radiotherapy Oncology,2013,109:335.
4支修益,石远凯,于金明,等.中国原发性肺癌诊疗规范(2015年版).中华肿瘤杂志,2015,37:67-78.
5张俊萍,毛光华,史天良,等.DC-CIK联合化疗治疗晚期非小细胞肺癌的临床疗效.中国肿瘤生物治疗杂志,2011,18:424-429.
6Mizuki N,Stephanie C,Jackman DM,et al.RECIST 1.1 in NSCLC patients with EGFR mutations treated with EGFR tyrosine kinase inhibitors: comparison with RECIST 1.0.Ajr American Journal of Roentgenology,2013,201:W64-71.
7姜珊.GP方案不同给药时间治疗晚期非小细胞肺癌疗效与安全性的回顾性研究.南开大学,2014.
8高云霄,张洁慧,刘元坤,等.顺铂脂质体联合化疗治疗非小细胞肺癌毒副作用的Meta分析.湖南中医杂志,2013,29:129-132.
9张晶,任秀宝.肿瘤微环境中负性调节树突状细胞功能的因素及治疗策略.国际免疫学杂志,2011,34:290-293.
10黄孙卉,张崇友.DC与CIK细胞共培养在肿瘤治疗中的研究进展.实用肿瘤学杂志,2011,25:14-17.
11黄香,陈龙邦.化疗药物的免疫调节作用.医学研究生学报,2010,23:76-81.
12盛春华,鲍锋,徐爽,等.化疗联合DC-CIK细胞治疗非小细胞肺癌临床研究.实用肿瘤杂志,2011,26:503-506.
13何立香.DC-DIK联合常规化疗治疗晚期NSCLC的临床研究.中南大学,2013.
14彭大为,李建旺,元建华,等.自体DC-CIK细胞联合培美曲塞治疗老年非小细胞肺癌的疗效与安全性.中国免疫学杂志,2012,28:648-651,656.
15蔡俊霞,谭洁,王彬,等.DC-CIK治疗43例晚期非小细胞肺癌的近期疗效观察.现代肿瘤医学,2014,22:67-70.
Clinical efficiency and safety of DC-CIK cells combined with conventional chemotherapy in treatment of advanced non small cell lung cancer
LIWeiwei,ZHANGHaiping,WUMin,etal.
DepartmentofOncology,TheFirstPeople’sHospitalofTianmenCity,Hubei,Tianmen431700,China
ObjectiveTo analyze the clinical efficiency and safety of DC-CIK cells combined with conventional chemotherapy in treatment of advanced non small cell lung cancer (NSCLC).MethodsEighty-one patients with NSCLC who were admitted and treated in Department of Oncology of our hospital from January 2010 to October were enrolled in the study. According to different therapy modes,these patients were divided into observation group (n=40) and control group (n=41). The patients in observation group were treated by NP chemotherapy combined with DC-CIK cells,however,the patients in control group were treated by NP chemotherapy only. The therapeutic effects, performance status (Karnofsky score ), changes of immune function, blood routine test, liver and kidney function, adverse reactions, survival status were observed and compared between two groups.ResultsThe total effective rate in observation group and control group was 37.50% and 29.27%,respectively, there was no significant difference between two groups (χ2=1.468,P>0.05).The disease control rate and total improvement rate of physical state in observation group was 87.50%, 90.00%,respectively,which was significantly higher than that (75.61%, 73.1%, respectively) in control group (P<0.05).Until the end of follow up,among 40 patients in observation group,30 patients died and 10 patients survived in whom the median carcinoma-free survival time was 7.5 months, and the median survival time was 14.5 months, however, among 41 patients in control group,35 patients died,6 patients survived in whom the median carcinoma-free survival time was 4.5 months, the median survival time was 11.5 months. Log-rank detection showed that the median carcinoma-free survival time in observation group was significant longer than that in control group (χ2=6.557,P<0.05),moreover, the median survival time in observation group was
non small cell lung cancer; chemotherapy; DC-CIK cell; effectiveness; safety
10.3969/j.issn.1002-7386.2016.19.004
431700湖北省天门市第一人民医院肿瘤科
R 734.2
A
1002-7386(2016)19-2900-05
2016-03-17)

