多系统萎缩P型与帕金森病患者临床特征及认知功能的比较研究
2016-10-09李哲贤宋伟强刘袁颖武德梅邢建华
李哲贤,宋伟强,刘袁颖,武德梅,邢建华
多系统萎缩P型与帕金森病患者临床特征及认知功能的比较研究
李哲贤,宋伟强,刘袁颖,武德梅,邢建华
目的比较多系统萎缩P型(MSA-P型)与帕金森病患者的临床特征及认知功能。方法选取2012年7月—2014年8月中国石油天然气总公司中心医院收治的MSA-P型患者31例作为A组,帕金森病患者53例作为B组。比较两组患者临床特征、运动功能、日常行为能力、认知功能、智力及记忆力。结果两组患者智能障碍发生率比较,差异无统计学意义(P>0.05);A组患者首发震颤发生率、锥体外系症状发生率低于B组,行走困难发生率、语言障碍发生率、小脑症状发生率、美多巴治疗无效率、锥体束症状发生率、性功能异常发生率、排尿异常发生率、直立性低血压发生率高于B组(P<0.05)。A组患者帕金森综合评分量表Ⅲ(UPDRS-Ⅲ)评分、日常生活活动能力量表(ADL)评分高于B组(P<0.05)。A组简易智能精神状态检查量表(MMSE)评分低于B组(P<0.05)。两组患者命名评分、注意力评分、语言评分、抽象能力评分、记忆评分、定向力评分及蒙特利尔认知评估量表(MoCA)总评分比较,差异无统计学意义(P>0.05);A组患者视空间/执行功能评分低于B组(P<0.05)。A组患者操作量表评分低于B 组(P<0.05);两组患者中国修订韦氏成人智力量表(WAIS-RC)总评分、言语量表评分比较,差异无统计学意义(P>0.05)。两组患者视觉再认评分、相似性评分、数字广度评分比较,差异无统计学意义(P>0.05);A组患者视觉再生评分、理解记忆评分、图形排列评分、积木测试评分、韦氏成人记忆量表总评分低于B组(P<0.05)。结论MSA-P型与帕金森病患者临床特征及认知功能存在差异,与帕金森病患者比较,MSA-P型患者认知功能、智力及记忆力较差。
多系统萎缩;帕金森病;认知障碍
李哲贤,宋伟强,刘袁颖,等.多系统萎缩P型与帕金森病患者临床特征及认知功能的比较研究[J].实用心脑肺血管病杂志,2016,24(8):24-28.[www.syxnf.net]
LI Z X,SONG W Q,LIU Y Y,et al.Comparative study for clinical features and cognitive function between patients with P-type multiple system atrophy and patients with parkinson′s disease[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2016,24(8):24-28.
多系统萎缩(MSA)是一种复杂的神经系统变性疾病,其发病机制尚不明确,病变范围可累及锥体外系、锥体系、小脑和自主神经等。MSA后期临床表现为帕金森综合征、共济失调、自主神经功能减退等[1]。近年来,医学界对MSA的研究不断深入,但由于MSA的临床症状与帕金森症相似,因此需对MSA与帕金森病进行鉴别诊断,待明确诊断后才能进行有效的治疗。目前根据国际通用的MSA诊断标准(2008年,第2版)可将MSA分为2种临床亚型,即多系统萎缩P型(MSA-P型)和多系统萎缩C型(MSA-C型)。MSA-P型主要以帕金森样症状为主,对左旋多巴反应不理想;MSA-C型以小脑性共济失调症状为主[2]。MSA-P型常需要与帕金森病进行鉴别,以明确诊断。目前有关MSA-P型与帕金森病的快速鉴别诊断技术已成为临床研究热点之一。有研究表明,MSA患者认知功能损伤较重[3-4]。为更准确、有效地鉴别MSA-P型与帕金森病,本研究比较了MSA-P型与帕金森病患者的临床特征及认知功能,旨在为MSA-P型与帕金森病的鉴别诊断和治疗提供参考,现报道如下。
1 资料与方法
1.1一般资料选取2012年7月—2014年8月中国石油天然气总公司中心医院收治的MSA-P型患者31例作为A组,帕金森病患者53例作为B组。A组中男14例,女17例;平均年龄(61.2±11.6)岁。B组中男25例,女28例;平均年龄(62.3±12.3)岁。两组患者性别、年龄、发病年龄、受教育时间、病程比较,差异无统计学意义(P>0.05,见表1),具有可比性。纳入标准:(1)符合MSA-P的诊断标准和英国帕金森病协会脑库的诊断标准[3-4];(2)经本院医学伦理学委员会审核批准;(3)自愿参与本研究,并签署知情同意书。排除标准:(1)存在帕金森叠加综合征(如路易体痴呆、进行性核上性麻痹、皮质基底核变性等)患者;(2)继发性帕金森综合征患者;(3)存在心、肺、肝、脾、肾等重要脏器功能不全患者。
1.2一般资料收集方法采用本研究项目组自制的调查问卷收集患者一般资料,包括性别、年龄、发病时间、受教育时间、病程等。

表1 两组患者一般资料比较
注:a为χ2值
1.3观察指标比较两组患者临床特征、运动功能和日常行为能力、认知功能、智力及记忆力。(1)运动功能和日常行为能力:采用帕金森综合评分量表Ⅲ(UPDRS-Ⅲ)评定患者的运动功能,分数越低表示运动功能越好;采用日常生活活动能力量表(ADL)评定患者的日常行为能力,满分100分,<20分为极严重的功能缺陷,生活完全依赖他人; 20~40分为生活需要很大帮助;41~60分为生活需要帮助; >60分为生活基本自理。(2)认知功能:采用蒙特利尔认知评估量表(MoCA)、简易智能精神状态检查量表(MMSE)评定患者认知功能[5-7],MoCA包括视空间/执行功能、命名、注意力、语言、抽象能力、记忆、定向力,总分30分,分数越高表示认知功能越好;MMSE评分越高表示认知功能越好。(3)智力:采用中国修订韦氏成人智力量表(WAIS-RC)评估患者的智力,包括11个分测验,分为言语量表和操作量表,其中言语量表包括知识、领悟、算术、相似性、数字广度、词汇共6个分测验,操作量表包括数字符号、图画填充、木块图、图片排列、图形拼凑共5个分测验,得分越高表示智力水平越好。(4)记忆力:采用韦氏成人记忆量表评估患者的记忆力,包括视觉再认、视觉再生、理解记忆、相似性、图形排列、积木测试、数字广度等维度,得分越高表示记忆力越好。

2 结果
2.1临床特征两组患者智能障碍发生率比较,差异无统计学意义(P>0.05);A组患者首发震颤发生率、锥体外系症状发生率低于B组,行走困难发生率、语言障碍发生率、小脑症状发生率、美多巴治疗无效率、锥体束症状发生率、性功能异常发生率、排尿异常发生率、直立性低血压发生率高于B组,差异有统计学意义(P<0.05,见表2)。
2.2运动功能和日常行为能力A组患者UPDRS-Ⅲ评分、ADL评分高于B组,差异有统计学意义(P<0.05,见表3)。

Table3ComparisonofUPDRS-ⅢscoreandADLscorebetweenthetwogroups

组别例数UPDRS-Ⅲ评分ADL评分A组3143.89±18.2032.49±11.32B组5328.56±15.2917.45±4.72t值4.1307.048P值P<0.05P<0.05
注:UPDRS-Ⅲ=帕金森综合评分量表Ⅲ,ADL=日常生活活动能力量表
2.3认知功能A组患者MMSE评分为(26.4±3.2)分,B组患者MMSE评分(28.4±2.5)分。A组MMSE评分低于B组,差异有统计学意义(t=3.247,P=0.002)。两组患者命名评分、注意力评分、语言评分、抽象能力评分、记忆评分、定向力评分及MoCA总评分比较,差异无统计学意义(P>0.05);A组患者视空间/执行功能评分低于B组,差异有统计学意义(P<0.05,见表4)。
2.4智力A组患者操作量表评分低于对照组,差异有统计学意义(P<0.05);两组患者WAIS-RC总评分、言语量表评分比较,差异无统计学意义(P>0.05,见图1)。
2.5记忆力两组患者视觉再认评分、相似性评分、数字广度评分比较,差异无统计学意义(P>0.05);A组患者视觉再生评分、理解记忆评分、图形排列评分、积木测试评分、韦氏成人记忆量表总评分低于B组,差异有统计学意义(P<0.05,见表5)。
3 讨论
MSA的临床症状包括帕金森综合征、自主神经系统功能紊乱和进行性小脑性共济失调等。20世纪末提出了关于MSA的诊断标准及排除标准,根据临床表现可诊断为拟诊MSA、疑似MSA和确诊MSA 3层,具有一定的临床参考价值[8-9]。GILMAN等对MSA的诊断标准进一步完善后,建议将MSA分为MSA-P型和MSA-C型,MSA-P型以帕金森症为主,MSA-C型以小脑症状为主。MSA和帕金森病均为复杂性神经系统疾病,MSA-P型与帕金森病发病前期的临床症状非常相似,故临床诊断难度较大,不利于临床治疗[10-13]。据统计,临床约1/5的MSA-P型患者于发病早期被误诊为帕金森病[12]。由于MSA-P型与帕金森病患者治疗方法及预后差别较大,故临床需进行鉴别诊断,以便采取正确的方法治疗。

表2 两组患者临床特征比较〔n(%)〕
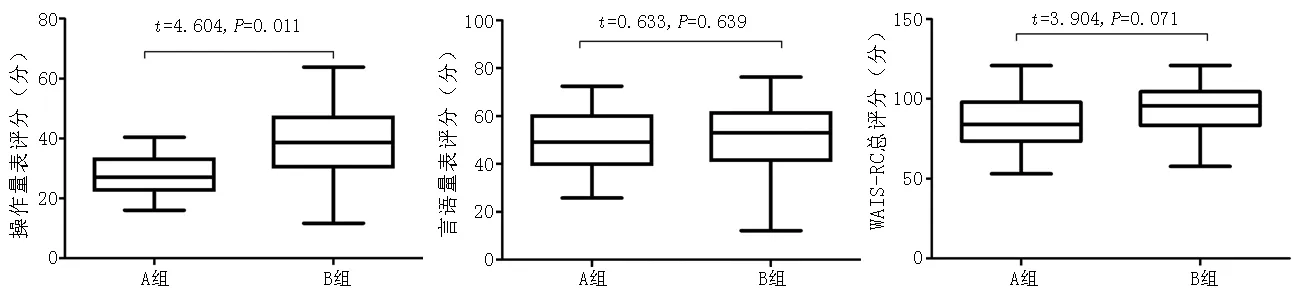
注:WAIS-RC=中国修订韦氏成人智力量表

图1 两组患者WAIS-RC评分比较

表5 两组患者韦氏成人记忆量表评分比较±s,分)
传统观点认为,MSA与帕金森病好发于中年人群。本研究结果显示,MSA-P型与帕金森病患者的发病年龄间无差异;两组患者智能障碍发生率间无差异,A组患者首发震颤发生率、锥体外系症状发生率低于B组,行走困难发生率、语言障碍发生率、小脑症状发生率、美多巴治疗无效率、锥体束症状发生率、性功能异常发生率、排尿异常发生率、直立性低血压发生率高于B组,与相关研究结果相似[9,14-15]。提示MSA-P型与帕金森病患者会发生不同程度的自主神经系统功能障碍,MSA-P型患者自主神经系统、锥体系统损伤程度较帕金森病患者更重。目前通用的MSA诊断标准中将有无自主神经功能障碍作为MSA拟诊的首要条件[1,9,14-15]。
有研究表明,MSA患者痴呆发生率低于帕金森病患者,MSA-P型和MSA-C型患者痴呆发生率约为31%[10,16-17],故不能仅依据有无痴呆症状鉴别MSA-P型和帕金森病。本研究结果显示,A组患者UPDRS-Ⅲ评分、ADL评分高于B组;A组MMSE评分低于B组;两组患者命名评分、注意力评分、语言评分、抽象能力评分、记忆评分、定向力评分及MoCA总评分间无差异,A组患者视空间/执行功能评分低于B组;两组患者操作量表评分间有差异,两组患者WAIS-RC总评分、言语量表评分间无差异;两组患者视觉再认评分、相似性评分、数字广度评分间无差异,A组患者视觉再生评分、理解记忆评分、图形排列评分、积木测试评分、韦氏成人记忆量表总评分低于B组。提示MSA-P型与帕金森病患者的认知功能均存在一定损伤,但MSA-P型患者的认知功能损伤更明显。目前,有关MSA-P型患者出现认知障碍的病理机制尚未统一;但借助影像学技术进行神经病理学研究发现,MSA-P型患者存在前额叶、额叶、颞叶和顶叶的皮质萎缩,同时上述区域的脑代谢功能降低,这可能是导致其出现认知功能障碍的病理机制之一[8-9,18]。根据大量临床研究推测,由于MSA-P型患者额叶、颞叶、顶叶的皮质萎缩,可能会引起神经元丢失,从而引发认知功能障碍[4,7,10,19],但上述推测仍有待进一步研究证实。
综上所述,MSA-P型与帕金森病患者临床特征及认知功能存在差异,与帕金森病患者比较,MSA-P型患者认知功能、智力及记忆力较差,故临床可根据患者临床特征、认知功能等进行综合评估,对MSA-P型与帕金森病进行鉴别诊断。
作者贡献:李哲贤进行实验设计与实施、资料收集整理、撰写论文、成文并对文章负责;宋伟强、刘袁颖、武德梅进行实验实施、评估、资料收集;邢建华进行质量控制及审校。
本文无利益冲突。
[1]STAMELOU M,PILATUS U,REUSS A,et al.Brain energy metabolism in early MSA-P:A phosphorus and proton magnetic resonance spectroscopy study[J].Parkinsonism Relat Disord,2015,21(5):533-535.
[2]BASCHIERI F,CALANDRA-BUONAURA G,DORIA A,et al.Cardiovascular autonomic testing performed with a new integrated instrumental approach is useful in differentiating MSA-P from PD at an early stage[J].Parkinsonism Relat Disord,2015,21(5):477-482.
[3]FOKI T,STEININGER S,KASPRIAN G,et al.An exceptional case of MSA-P[J].J Neurol,2013,260(4):1171-1173.
[4]HOZUMI I,PIAO Y S,INUZUKA T,et al.Marked asymmetry of putaminal pathology in an MSA-P patient with Pisa syndrome[J].Mov Disord,2004,19(4):470-472.
[5]OUDMAN E,POSTMA A,VAN DER STIGCHEL S,et al.The Montreal Cognitive Assessment (MoCA) is superior to the Mini Mental State Examination (MMSE) in detection of Korsakoff′s syndrome[J].Clin Neuropsychol,2014,28(7):1123-1132.
[6]DONG Y,SHARMA V K,CHAN B P,et al.The Montreal Cognitive Assessment (MoCA) is superior to the Mini-Mental State Examination (MMSE) for the detection of vascular cognitive impairment after acute stroke[J].J Neurol Sci,2010,299(1/2):15-18.
[7]HOOPS S,NAZEM S,SIDEROWF A D,et al.Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease[J].Neurology,2009,73(21):1738-1745.
[8]PAVIOUR D C,PRICE S L,JAHANSHAHI M,et al.Regional brain volumes distinguish PSP,MSA-P,and PD:MRI-based clinico-radiological correlations[J].Mov Disord,2006,21(7):989-996.
[9]RAGOTHAMAN M,SWAMINATH P V,SARANGMATH N,et al.Role of dysautonomic symptoms in distinguishing Parkinson′s disease (PD) from multiple system atrophy (MSA-P) within a year of developing motor symptoms[J].J Assoc Physicians India,2011(59):95-98.
[10]KAMITANI T,KUROIWA Y,WANG L,et al.Visual event-related potential changes in two subtypes of multiple system atrophy,MSA-C and MSA-P[J].J Neurol,2002,249(8):975-982.
[11]KASTEN M,BRUGGEMANN N,SCHMIDT A,et al.Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease[J].Neurology,2010,75(5):478-479.
[12]KAWAI Y,SUENAGA M,TAKEDA A,et al.Cognitive impairments in multiple system atrophy:MSA-C vs MSA-P[J].Neurology,2008,70(16 Pt 2):1390-1396.
[13]KÖLLENSPERGER M,SEPPI K,LIENER C,et al.Diffusion weighted imaging best discriminates PD from MSA-P:A comparison with tilt table testing and heart MIBG scintigraphy[J].Mov Disord,2007,22(12):1771-1776.
[14]PENDLEBURY S T,MARKWICK A,DE JAGER C A,et al.Differences in cognitive profile between TIA,stroke and elderly memory research subjects:a comparison of the MMSE and MoCA[J].Cerebrovasc Dis,2012,34(1):48-54.
[15]RAZALI R,JEAN-LI L,JAFFAR A,et al.Is the Bahasa Malaysia version of the Montreal Cognitive Assessment (MoCA-BM) a better instrument than the Malay version of the Mini Mental State Examination (M-MMSE) in screening for mild cognitive impairment (MCI) in the elderly?[J].Compr Psychiatry,2014(1):S70-75.
[16]PAVIOUR D C,PRICE S L,LEES A J,et al.MRI derived brain atrophy in PSP and MSA-P.Determining sample size to detect treatment effects[J].J Neurol,2007,254(4):478-481.
[17]YAMAMOTO T,SAKAKIBARA R,UCHIYAMA T,et al.Pelvic organ dysfunction is more prevalent and severe in MSA-P compared to Parkinson′s disease[J].Neurourol Urodyn,2011,30(1):102-107.
[18]TIR M,DELMAIRE C,LE THUC V,et al.Motor-related circuit dysfunction in MSA-P:Usefulness of combined whole-brain imaging analysis[J].Mov Disord,2009,24(6):863-870.
[19]BARNAY J L,WAUQUIEZ G,BONNIN-KOANG H Y,et al.Feasibility of the cognitive assessment scale for stroke patients (CASP) vs.MMSE and MoCA in aphasic left hemispheric stroke patients[J].Ann Phys Rehabil Med,2014,57(6/7):422-435.
(本文编辑:李洁晨)
Comparative Study for Clinical Features and Cognitive Function between Patients with P-type Multiple System Atrophy and Patients with Parkinson′s Disease
LIZhe-xian,SONGWei-qiang,LIUYuan-ying,WUDe-mei,XINGJian-hua.
DepartmentofPreventiveMedicineandGeriatrics,theCentralHospitalofChinaPetroleumandNaturalGasCorporation,Langfang065000,China
ObjectiveTo compare the clinical features and cognitive function between patients with P-type multiple system atrophy and patients with Parkinson′s disease.MethodsFrom July 2012 to August 2014 in the Central Hospital of China Petroleum and Natural Gas Corporation,a total of 31 patients with P-type multiple system atrophy were selected as A group,53 patients with Parkinson′s disease were selected as B group.Clinical features,motor function,daily behavior ability,cognitive function,mentality and memory were compared between the two groups.ResultsNo statistically significant differences of incidence of mental retardation was found between the two groups(P>0.05);incidence of initial tremor and extrapyramidal symptoms of A group was statistically significantly lower than that of B group,respectively,while incidence of mobility limitation,linguistic barrier,cerebellum symptoms,pyramidal tract symptoms,sexual dysfunction,paruria and postural hypotension,and ineffective rate of madopar of A group was statistically significantly higher than that of B group(P<0.05).UPDRS-Ⅲ scores and ADL scores of A group were statically significantly higher than those of B group(P<0.05).MMSE score of A group was statistically significantly lower than that of B group(P<0.05).No statistically significant differences of naming score,attentiveness score,language score,abstract ability score,memory score,directive force score and total MoCA score was found between the two groups(P>0.05),while visual space/executive function score of A group was statistically significantly lower than that of B group(P<0.05).Operating Scale score of A group was statistically significantly lower than that of B group(P<0.05),while no statistically significant differences of total WAIS-RC score or Verbal Scale score was found between the two groups(P>0.05).No statistically significant differences of visual recognition score,similarity score or digit span score was found between the two groups(P>0.05);while visual reproduction score,comprehension memory score,graphic arrangement score,building test score and total Wechsler Adults Memory Scale score of A group were statistically significantly lower than those of B group(P<0.05).ConclusionThere are significant differences of clinical features and cognitive function between patients with P-type multiple system atrophy and patients with Parkinson′s disease,cognitive function,mentality and memory of patients with P-type multiple system atrophy are worse than those of patients with Parkinson′s disease.
Multiple system atrophy;Parkinson disease;Cognition disorders
065000河北省廊坊市,中国石油天然气总公司中心医院保健与老年医学科
R 745.7R 742.5
A
10.3969/j.issn.1008-5971.2016.08.006
2016-03-04;
2016-07-16)
