Magnitude and determinants of retinal degeneration in children with myopia of Western India
2016-09-02KhandekarRajivKulkarniSuchetaSavePrajactaDoleKuldeepDeshpandeMadanTarasSudhir
Khandekar Rajiv, Kulkarni Sucheta, Save Prajacta, Dole Kuldeep, Deshpande Madan, Taras Sudhir
·Original article·
Magnitude and determinants of retinal degeneration in children with myopia of Western India
Khandekar Rajiv1, Kulkarni Sucheta2, Save Prajacta2, Dole Kuldeep2, Deshpande Madan2, Taras Sudhir2
1Aruba Road Research Department, King Khaled Eye Specialist Hospital, Al Aruba Road, Riyadh 11462, Saudi Arabia
2Department of Ophthalmology, HV Desai Eye Hospital, S.No.93/2 mohammadwadi Hadapsar, Pune, Maharashtra 411060, India
Correspondence to:Khandekar Rajiv. Aruba Road Research Department, King Khaled Eye Specialist Hospital, Al Aruba Road, Riyadh 11462, Saudi Arabia. rajiv.khandekar@gmail.com
目的:研究≥3.00D近视儿童视网膜变性的的发病率,类型和决定因素。
方法:选取研究对象为2010/2011年期间在印度马哈拉施特拉邦一所眼科医院就诊的患者。询问并记录高度近视儿童家属成员的近视史,并统计人口信息。由验光师评估每位患者的视力和屈光状态。由眼科医生对患儿进行眼科检查,评估中央和周边视网膜变化。计算出中央及周边视网膜变性的百分比。评估视网膜改变与家族近视史性别、年龄、宗教以及近视程度的相关性。应用单因素和多因素分析。
结果:共纳入≥3.00D近视儿童499位(847眼)。检查发现150眼(17.7%,95%可信区间15.4~20.4)玻璃体视网膜退化性改变。黄斑变性、后巩膜葡萄肿及格子样变性比例分别为2.0%、4.6%和18%。眼轴大于24 mm是大于5.00D近视发生玻璃体视网膜退化性改变的显著危险因素(OR=3.88)。视觉辅助的依从性为58.4%。499位患儿中8.8%视力低于6/60,他们可借助于低视力保健。
结论:近1/5近视患者存在玻璃体视网膜变性。高度近视玻璃体视网膜变性较少有严重后果。建议应定期对近视眼进行详细的视网膜检查。
引用:Khandekar R, Kulkarni S, Save P, Dole K, Deshpande M, Taras S. 印度西部近视儿童视网膜变性的病变程度及其决定性因素.国际眼科杂志2016;16(9):1609-1614
Abstract
•AIM:To present incidence, types and determinants of retinal degeneration among children with myopia of ≥3 diopter (D).
•METHODS: This case series type of study was conducted during 2010-2011 at an eye hospital in Western Maharashtra, India. Children with high myopia were interviewed to record history of myopia in family members and to collect demographic information. Optometrist evaluated visual and refractive status of each eye. Ophthalmologist examined eyes of children to assess central and peripheral retinal changes. We calculated percentage proportion of eyes with central and peripheral retinal degeneration. We also reviewed the association of family history of myopia, sex, age, religion and grade of myopia with retinal changes. We performed univariate & multivariate analysis.
•RESULTS: Eight hundred and forty-seven eyes of 499 children were examined with myopia of ≥ 3 D. In 150 eyes [17.7% (95% confidence interval 15.4-20.4)], we found vitreo-retinal degenerative changes. The rate of macular degeneration, posterior scleral staphyloma, lattice degeneration was 2.0%, 4.6% and 18% respectively. Axial length of more than 24 mm was significant risk factor (Adjusted Odd’s Ratio=3.88) of vitreo retinal degeneration in eyes with myopia of more than 5 D. The compliance of visual aid was 58.4%. There were 8.8% of the 499 children’s vision was less than 6/60 and they could benefit from low vision care.
•CONCLUSION: Nearly one fifth of eyes with myopia had vitreo retinal degeneration. High myopia had less vitreo retinal degeneration of serious consequences. Detailed retinal examination of eyes with myopia should be carried out periodically.
•myopia; vitreo retinal degeneration; retina
INTRODUCTION
Myopia is a type of refractive error in which distant vision is blurred due to the longer axial length of the eyeball or a steep curvature along its refractive surfaces[1]. The prevalence of myopia in children is rising[2]. Fortunately, this defect can be corrected with concave spectacles, contact lenses or by performing refractive surgery[3]. High myopia is often associated with changes in the posterior segment[4]. This can cause a serious sight threatening complication called retinal detachment. As this complication usually occurs in young adults, the economic burden of retinal detachment due to myopia tends to be high. Although, prophylactic management of retinal detachment in children with high myopia could be cost effective, its clinical significance is still debatable[5]. Nevertheless, early detection of myopic degeneration is useful in identifying high risk groups and closely monitoring them. Literature has documented few studies related to this issue[6-7]. To our knowledge, such research among children of Indian subcontinent has not been undertaken. In children, myopia is usually progressive. Those exhibiting moderate myopia at younger ages are likely to have high myopia in late teenage years[8]. Peripheral retinal degeneration in the eyes of children with moderate myopia show that 10% of them could develop retinal detachment when they become 40 to 60y old[9]. Hence, such changes should be monitored regularly for timely detection.
Ours is a tertiary eye care unit with community ophthalmology subspecialty. Vision screening of school-children is periodically undertaken. The eye care-providers were concerned about rising trend of high myopia. Serious sight-threatening complications of high myopia like retinal detachment could be prevented by prophylactic treatment mainly of lattice degenerations. In order to ascertain the situation in Western Indian children, we conducted a study with the objective of determining the type and frequency of vitreo-retinal changes in children that had more than 3D myopia in at least one eye.
MATERIALS AND METHODS
The ethical and research committee of our hospital approved this study.Informed verbal consent was obtained from each participant. This study was conducted between Jan. 2010 and Jul. 2011.
This was a case series type of study. The study population comprised of children with more than 3D of myopia and had visited our institute during the study period. If a child had myopia associated with syndrome or the parents did not give consent to participate inthe study, he/she was excluded.
To calculate the sample size of our study, we used the statistical calculator, Open EPI software[10]. In a population of 100000 children with moderate and high myopia, we assumed that 50% would have degenerative changes[11]. To have a 95% confidence interval and 5% of acceptable error margin with a design effect of 2 for our study, we needed a randomly selected 768 eyes of children with moderate and high myopia. To compensate for the loss of data, we increased the sample by 10%. Thus, the final sample required for our study was at least 840 eyes. We included all the children with >3D myopia in our study. The children with syndrome and those with poor cooperation due to low intelligence quotient (IQ) (based on their family physician’s report) were excluded from the study.
The child and his/her parents were interviewed to inquire about age (range of 9mo to 16y), gender, religion, history of myopia in other family members, history of retinopathy of prematurity and its treatment, history of retinal detachment and its treatment, use of spectacles, eye symptoms and any eye surgery performed in the past. If any family member had myopia, further details were obtained about their relation to the child.
Two ophthalmologists and two optometrists were our field staff. To assess the presented and the best corrected visual acuity (BCVA) for distance, we used Snellen’s illiterate ‘E’ chart that was held at six meter distance from the child. If child could not correctly identify ‘E’ of the top line, the test was repeated at a three meter distance. A child’s vision was tested with his/her spectacles. The anterior segment of the eye was evaluated using slit lamp bio-microscope (Appasamy, India). The retina and optic nerve head were examined using +90D Volk lens and slit lamp bio-microscope. Medical retina specialist evaluated peripheral retina by using indirect binocular ophthalmoscope (Keeler, UK) and a +20D (Volk, USA) fundus lens. A slit beam was used to determine the retinal hole.
The central retinal degeneration were graded as Peripapillary atrophy (PPA), macular degeneration and posterior staphyloma and combination of all of the above. The peripheral retinal degeneration was classified as white without pressure, white with pressure, lattice degeneration, snail track and/or combination of all of the above.
The BCVA in the eye was further graded as per the WHO ICD10 code. If vision was 6/6 to 6/18, it was considered normal. For vision between 6/24 and 6/60, the eye was defined to have moderate visual impairment. If the eye showed vision less than 6/60 and ≥ 3/60, it was defined as a severe visual impairment. If vision was <3/60, the eye was considered as blind[12]. The vision in the fellow eye was better but not accounted for the present study. The children underwent cycloplegic refraction. We used 0.5% Homeatropine for this purpose. For children of less than two years, we used 1% atropine eye ointment for cycloplegia. Streak retinoscope (Heine, Germany) was used. The subjective correction was carried out after one week to determine the BCVA. Children of preverbal age, we used Lea Paddle to test visual acuity.
Moderate myopia was defined as an eye with 3D to <5D myopia. High myopia was further graded into 5D to 7D, >7D to 9D, >9D to 12D, >12D to 15D and >15D. The axial length of eye ball was measured using ultrasound sonography ‘A’ scan (Appasamy, India). The length of eye ball was graded as 16 to 20 mm (mild), 21 to 24 (moderate), 25 to 27 mm (severe), >27 to 32 mm (profound). The status of vitreous was graded as posterior vitreous detachment (PVD), liquefied vitreous, Familial Exudative Vitreoretinopathy (FEVR) and no abnormality of vitreous.
Table 1Profile of children with more than 3D myopia
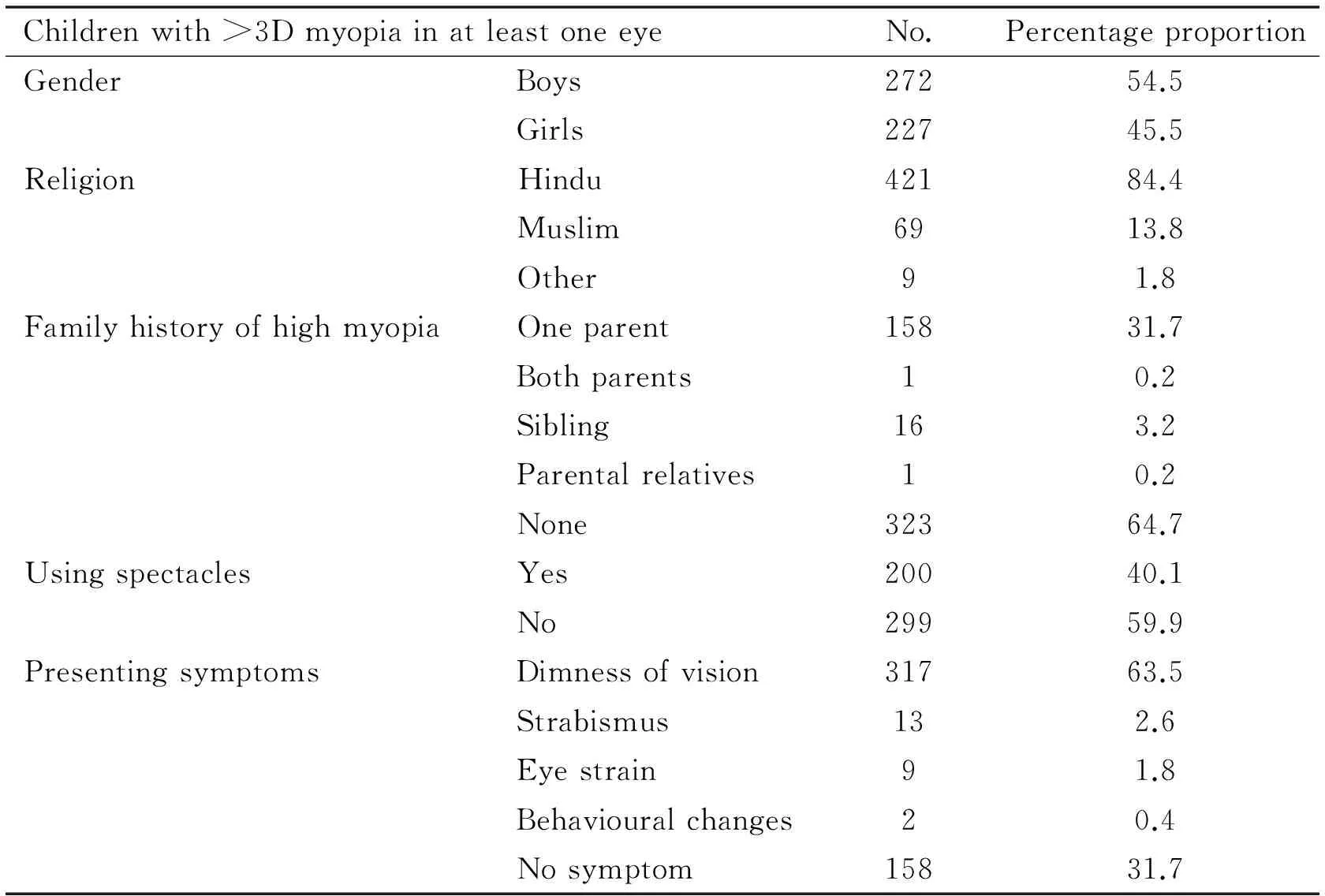
Childrenwith>3DmyopiainatleastoneeyeNo.PercentageproportionGenderBoys27254.5Girls22745.5ReligionHindu42184.4Muslim6913.8Other91.8FamilyhistoryofhighmyopiaOneparent15831.7Bothparents10.2Sibling163.2Parentalrelatives10.2None32364.7UsingspectaclesYes20040.1No29959.9PresentingsymptomsDimnessofvision31763.5Strabismus132.6Eyestrain91.8Behaviouralchanges20.4Nosymptom15831.7
The data was entered in computer using spreadsheet of Microsoft Excel®(Microsoft Inc., USA). For continuous variable like age, we ensured that its distribution was normal. We calculated the mean and standard deviation of age. For a qualitative variable, we calculated Odd’s Ratio (OR) and its 95% confidence interval (CI) with two tailed ‘P’ value. We also calculated chi-square value, degree of freedom and its 95% CI.
If children with myopia were found to have retinal degeneration with risk of impending retinal detachment, we applied prophylactic laser to seal the degenerative area. The identity of child was delinked from other data while analysis to maintain confidentiality. The outcomes of study were presented in Maharashtra ophthalmology society meeting in 2011.
RESULTS
We examined 847 eyes of 499 children that had more than 3D of myopia. Only 200 (40.1%) children were using spectacles at the time of their hospital visit. The mean age of participants was 10.6y (Standard deviation 3.22y, lowest 9mo and highest 16y). The profile of the examined sample is given in Table 1.
The presented and best corrected visual acuity of eyes with moderate and high myopia are presented in Figure 1. Despite spectacles, 52 (6.1%) eyes had BCVA less than 3/60 while another 36 eyes (4.3%) had BCVA 6/60 to 3/60.
X axis: number of eyesThe severity of myopia was analysed (Figure 2). In 118 (13.9%) eyes, myopia was of 5 to 7 D grade. One hundred and fifty (17.1%) eyes had myopia of more than 9D.
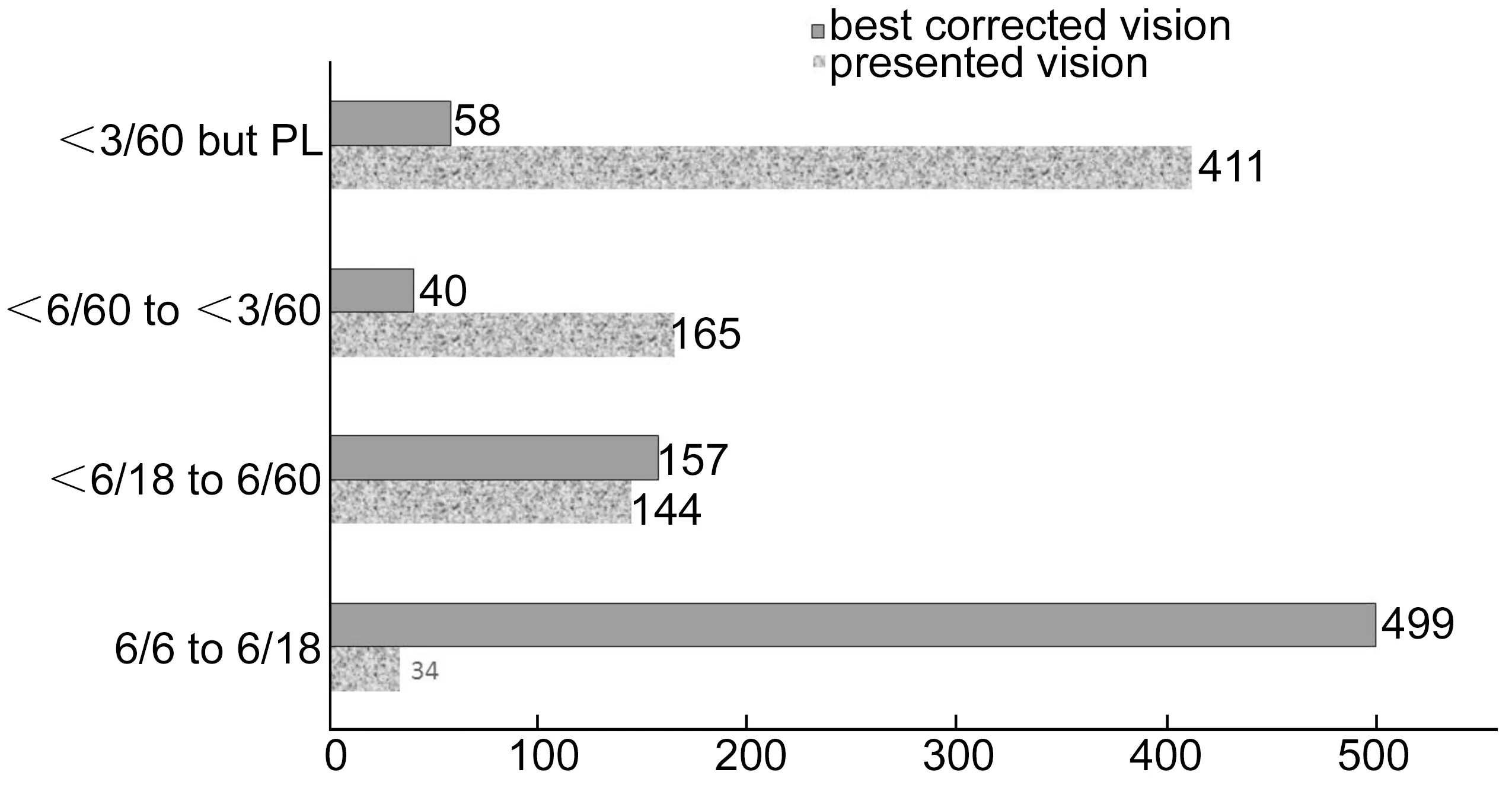
Figure 1Presented and the best corrected visual acuity in eyes of children with moderate and high myopia.
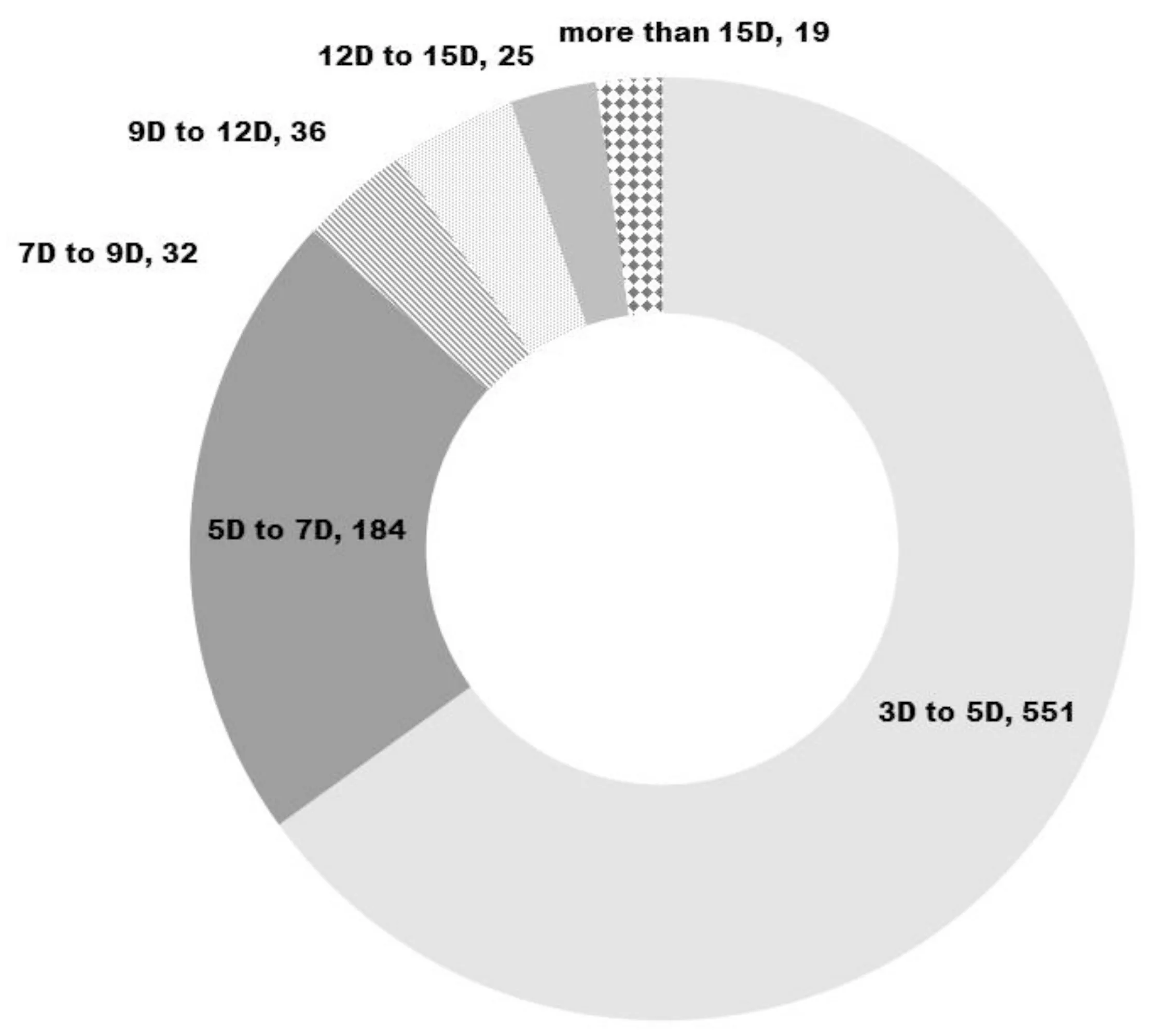
Figure 2Severity of myopia in eyes of children with moderate and high myopia.
The grades of axial length of eyeball among study sample suggested that 254 (30%) of eyes had axial length between 24 to 27 mm and 55 (6.5%) eyes had axial length of more than 27 mm. (Figure 3).The number, percentage proportion and 95% confidence interval of different vitro retinal degeneration (including isolated vitreous and retinal degeneration) were calculated (Table 2). All types of vitreo retinal degeneration was noted in 129 [(14.3%), 95% confidence interval 11.9-16.7]. Sight threatening macular degeneration and staphyloma was noted in 77 (9.1%) of eyes while lattice degeneration a risk for retinal detachment was found in 37 (4.4%) eyes.
Table 3Risk factors of retinal degeneration in eyes with moderate and high myopia
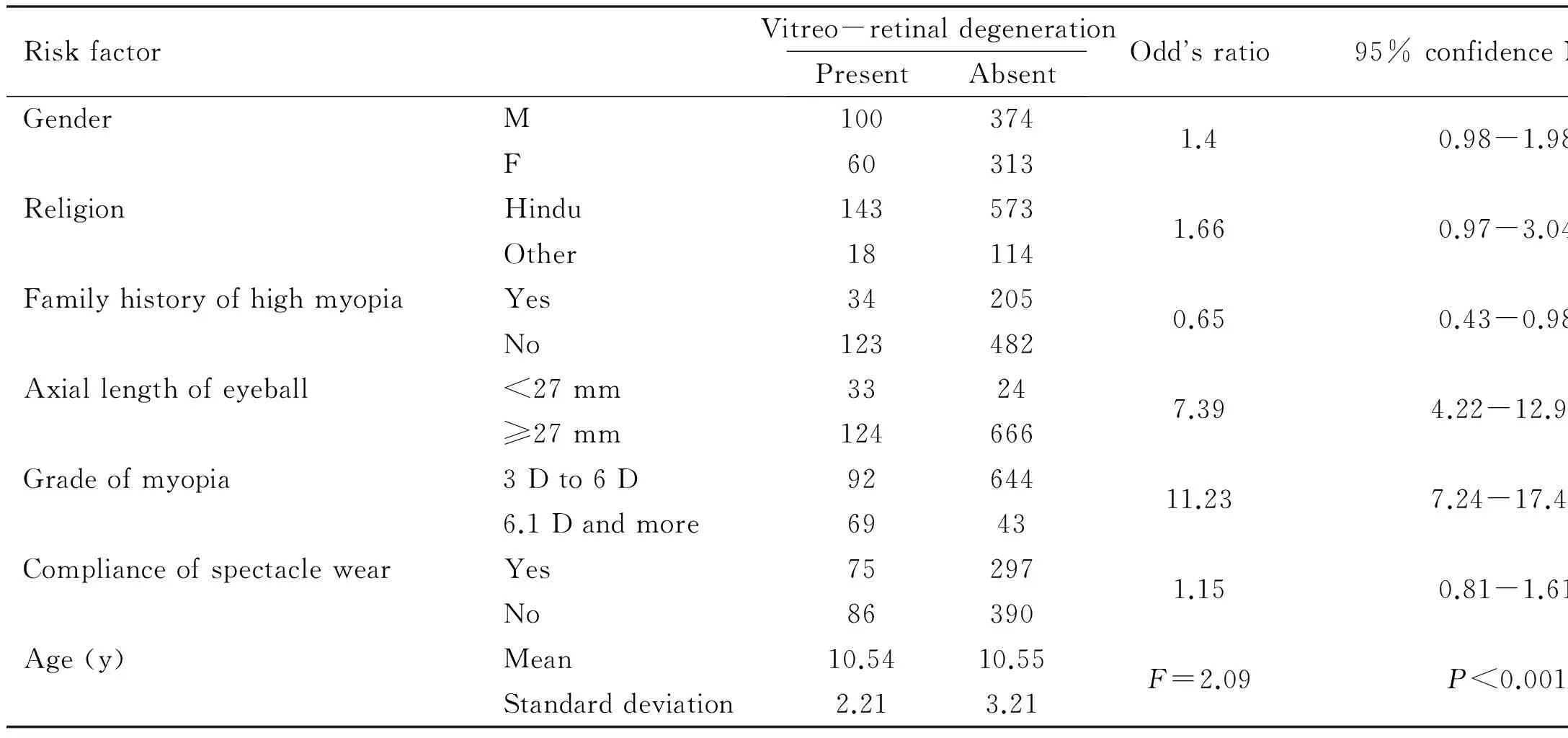
RiskfactorVitreo-retinaldegenerationPresentAbsentOddsratio95%confidenceIntervalGenderM1003741.40.98-1.98F60313ReligionHindu1435731.660.97-3.04Other18114FamilyhistoryofhighmyopiaYes342050.650.43-0.98No123482Axiallengthofeyeball<27mm33247.394.22-12.92≥27mm124666Gradeofmyopia3Dto6D9264411.237.24-17.426.1Dandmore6943ComplianceofspectaclewearYes752971.150.81-1.61No86390Age(y)Mean10.5410.55F=2.09P<0.001Standarddeviation2.213.21
Table 4Predictors of central retinal degeneration in eyes with moderate and high myopia
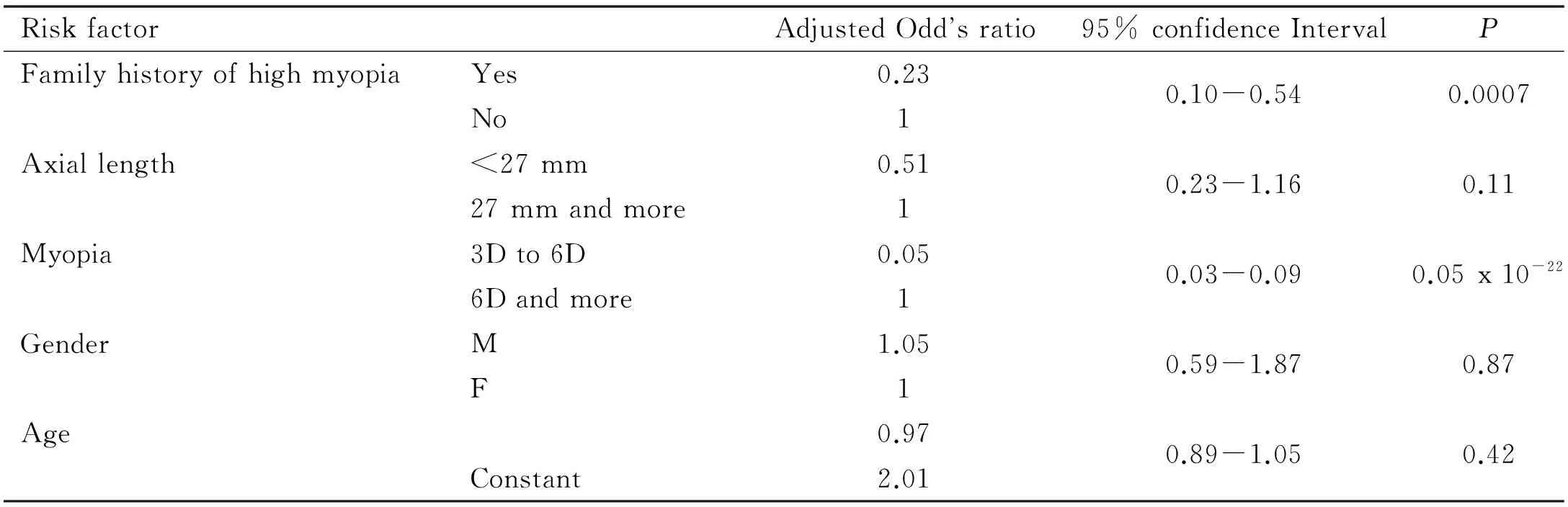
RiskfactorAdjustedOddsratio95%confidenceIntervalPFamilyhistoryofhighmyopiaYes0.230.10-0.540.0007No1Axiallength<27mm0.510.23-1.160.1127mmandmore1Myopia3Dto6D0.050.03-0.090.05x10-226Dandmore1GenderM1.050.59-1.870.87F1Age0.970.89-1.050.42Constant2.01
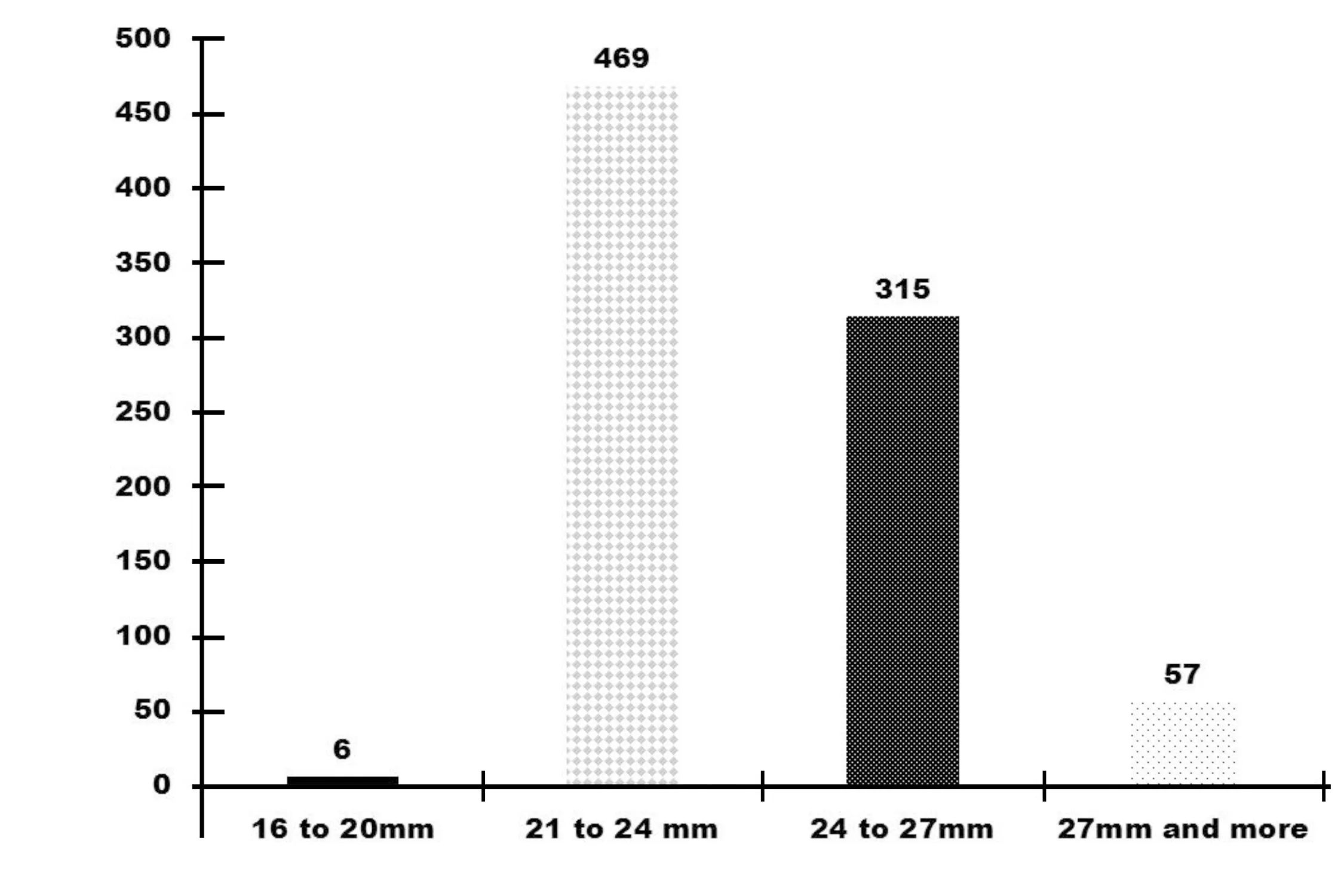
Figure 3Axial length of eyeball of children with moderate and high myopia.
We associated presence of vitreo retinal degeneration to risk factors like, family history of high myopia, severe grade of myopia, high axial length of globe, gender, age and compliance of spectacle wear(Table 3).
Of 104 eyes with lattice degeneration, 23 had family history of high myopia. Among 743 eyes without lattice degeneration, 216 had family history of high myopia. Lattice degeneration was negatively associated to the family history of moderate and high myopia. [OR=0.69 (95%CI0.31-1.5)].
We conducted binominal regression analysis to identify the predictors of central retinal degeneration in eyes with moderate and high myopia. More than 6 D myopia and absence of family history of high myopia were independently associated to central retinal degeneration (Table 4).
DISCUSSION
In this study, vitreo retinal (VR) degeneration was found in 14.3% of children with ≥3D myopia. Axial length, myopia of >6D were significant predictors of vitreo retinal degeneration. High rate of non-compliance of visual aid (60%) among children with myopia is a matter of concern. Children with low vision disability need further assessment to provide low vision rehabilitation.
The rate of VR degeneration in our study was less than that reported by Il’nitskiǐetal[11]. Differences in age group and study population in our and the study in Russia could explain this variation in rates of VR degeneration. Lattice type of peripheral retinal degeneration was noted in 4.4% of eyes with myopia. Bansaletal[7]had reported as high as 33% of eyes with lattice among <10y old children with myopia of ≥ 6 D myopia. Gozumetal[13]had observed that lattice degeneration was frequent in the eyes of people of all ages and with high myopia. But they postulated that the rate of lattice degeneration increases with the age and the axial length. Since our series had only children of less than 16y of age and we excluded cases with syndromes, the rate of lattice degeneration could be low. Rate of posterior staphyloma and posterior vitreous detachment in our series was 4.6% and 2.6% respectively. This was lower than reported in a study in Turkey[13]. The progressive nature of increases in the axial length and younger age group could be the reason for these differences.
We did not find significant association of VR degeneration and family history of myopia. Perhaps high myopia in our population could be due to acquired factors. Absence of sufficient evidence regarding the presence and exact location of myopia susceptibility gene observed by Young[14]and his proposal for further study matches the findings of our study.
Compliance of spectacle wear was 40.1%. This was surprising as their distant vision as presented improved considerably by giving them the best correction. It may also be possible that children with progressive myopia, with frequent change in power of correction cannot afford to procure spectacles too often and hence they were not using spectacles when they visited our institution. More frequent vision testing and provision of affordable refractive services could improve non compliance.
Sight threatening peripheral retinal degeneration can be treated by prophylactic laser treatment. This has shown decline in the risk of retinal detachment[4]. Even central degenerative changes have been managed by using posterior scleral reinforcement[15].
These findings show the importance of early detection of sight threatening types of VR degeneration so that they can be offered intervention at early stages[16].
We found longer axial length of eyeball was negatively associated to vitreo-retinal degeneration. Celarioetal[17]have reported that the longer axial length is associated to the high prevalence of lattice degeneration. A review of literature on myopia suggests that Axial length is the primary determinant of non-syndromic myopia[18]. Negative association of axial length and retinal degeneration need further investigation and explanation.
We did not find gender variation in rates of vitreo retinal degeneration. Taruttaetal[18]had noted higher rates of peripheral vitreo choroidal dystrophies than in males with high myopia. In that study, adults with myopia were observed while in the present study myopic children were included. The differences in age in these two studies should be noted before comparison.
Our study had few limitations. The sample was calculated assuming vitro retinal degeneration rate of 50% (±5%). However, the final rate of vitreo retinal degeneration in our study population of less than 16y was 14.3%. This could have resulted in a systematic error and hence, the extrapolation of our study result should be carried out with a caution. Being a case series, the outcome (Vitreo retinal degeneration) and other co-variables of our study were collected at one point. The spatial relationship between outcome variable and axial length, degree of myopia could not be established and hence causal relationship must not be assumed. The children were not selected randomly from a study population. Hence, the extrapolation of our study results to children with moderate and high myopia of the Indian subcontinent should be carried out with caution.
The prevalence of myopia worldwide and especially in the Asian population is high[19-21].Genes for myopia have been identified, but this knowledge is yet to be useful for the prevention of myopia[22].Children with high myopia should be detected and assessed periodically for retinal degeneration. High risk peripheral retinal degeneration like significant lattice should be monitored. Visual acuity of children with high myopia should be corrected with spectacles and if it is still compromised, low vision rehabilitation should be planned for them.
REFERENCES
1 Rosenfield M, Logan N, Edwards K. Development of refractive error inOptometryScience,Techniquesandclinicalmanagement. 2nd Ed. Elsevier Ltd. USA. 2009;10-21
2 Maduka Okafor FC, Okoye OI, Eze BI. Myopia: a review of literature.NigerJMed2009;18(2):134-138
3 Gwiazda J. Treatment options for myopia.OptomVisSci2009, 86(6):624-628
4 Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications.OphthalmicPhysiolOpt2005;25(5):381-391
5 Banker AS, Freeman WR. Retinal detachment.OphthalmolClinNorthAm2001;14(4):695-704
6 Lai TY, Fan DS, Lai WW, Lam DS. Peripheral and posterior pole retinal lesions in association with high myopia: a cross-sectional community-based study inHong Kong.Eye(Lond) 2008;22(2):209-213
7 Bansal AS, Hubbard GB 3rd. Peripheral retinal findings in highly myopic children < or =10y of age.Retina2010;30:15-19
8 Khandekar R, Kurup P, Mohammed AJ. Determinants of the progress of myopia among Omani school children: a historical cohort study.EurJOphthalmol2007;17(1):110-116
9 Burton TC. The influence of refractive error and lattice degeneration on the incidence of retinal detachment.TransAmOphthalmolSoc1989;87:143-155
10 Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version. Available at www.OpenEpi.com, updated 2013/04/06, accessed 2016/08/01
11 Il’nitskiǐ VV, Saksonova EO, Gur’eva NV, Georgiev N, Balashova LM. Peripheral vitreochorioretinal dystrophies in myopia patients.VestnOftalmol1993;109(4):18-20
12 Change the definition of blindness. Available at http://www.who.int/blindness/Change%20the%20Definition%20of%20Blindness.pdf
13 Gözüm N, Cakir M, Gücukoglu A, Sezen F. Relationship between retinal lesions and axial length, age and sex in high myopia.EurJOphthalmol1997;7(3):277-282
14 Young TL. Molecular Genetics of Human Myopia: An Update.OptomVisSci2009;86(1):E8-E22
15 Zhu Z, Ji X, Zhang J, Ke G. Posterior scleral reinforcement in the treatment of macular retinoschisis in highly myopic patients.ClinExperimentOphthalmol2009;7(7):660-663
16 Hyams S. Prevalence of lattice degeneration and its relation to axial length in severe myopia.AmJOphthalmol1991;112(3):356-357
17 Meng W, Butterworth J, Malecaze F, Calvas P. Axial length of myopia: a review of current research.Ophthalmologica2011;225(3):127-134
18 Tarutta EP, Saksonova EO. State of peripheral sections of the fundus oculi in progressive high myopia.VestnOftalmol1991;107(1):54-58
19 Bloom RI, Friedman IB, Chuck RS. Increasing rates of myopia: the long view.CurrOpinOphthalmol2010;21(4):247-248
20 Lam CS, Lam CH, Cheng SC, Chan LY. Prevalence of myopia among Hong Kong Chinese schoolchildren: changes over two decades.OphthalmicPhysiolOpt2012;32(1):17-24
21 Krishnaiah S, Srinivas M, Khanna RC, Rao GN. Prevalence and risk factors for refractive errors in the South Indian adult population: The Andhra Pradesh Eye disease study.ClinOphthalmol2009;3:17-27
22 Jacobi FK, Pusch CM. A decade in search of myopia genes.FrontBiosci(LandmarkEd) 2010;15:359-372
印度西部近视儿童视网膜变性的病变程度及其决定性因素
Khandekar Rajiv1, Kulkarni Sucheta2, Save Prajacta2, Dole Kuldeep2, Deshpande Madan2, Taras Sudhir2
111462 沙特阿拉伯利雅得阿鲁巴路国王哈立德眼科专科医院研究部门;2411060 印度马哈拉施特拉邦浦那Mohammadwadi路93/2号H.V. Desai眼科医院眼科)
Khandekar Rajiv. rajiv.khandekar@gmail.com
近视;玻璃体视网膜变性;视网膜
10.3980/j.issn.1672-5123.2016.9.03
Khandekar R, Kulkarni S, Save P, Dole K, Deshpande M, Taras S. Magnitude and determinants of retinal degeneration in children with myopia of Western India.GuojiYankeZazhi(IntEyeSci) 2016;16(9):1609-1614
2016-6-20Accepted: 2016-6-22
