OCT-GPA技术在监测原发性开角型青光眼进展中的作用
2016-09-02关新辉
关新辉,李 丽,梁 勇
OCT-GPA技术在监测原发性开角型青光眼进展中的作用
关新辉,李丽,梁勇
Department of Ophthalmology, the Fifth Affiliated Hospital of Xinjiang Medical University, Urumqi 830054, China
Correspondence to:Yong Liang. Department of Ophthalmology, the Fifth Affiliated Hospital of Xinjiang Medical University, Urumqi 830054, China. iohey@163.com
Abstract
•AIM:To evaluate the ability of Cirrus spectral domain optical coherence tomography (SD-OCT)-guided progression analysis (GPA) software to detect glaucomatous progression in primary open angle glaucoma (POAG) patients.
•METHODS:Longitudinal study. The study examined 45 eyes of 36 patients with POAG over a 2y period. All eyes underwent at least four serial retinal nerve fiber layer (RNFL) thickness measurements performed by Cirrus OCT, with the first and last measurement separated by at least 2y. Visual field (VF) testing was performed by using the Swedish interactive threshold algorithm (SITA) Standard 30-2 program of the Humphrey field analyzer within the same week as the optic disc/RNFL photography. Serial RNFL thickness were assessed by the GPA software program. Glaucomatous eyes were classified as either early or advanced stage according to VF severity. At the same time each eye was labeled with status of RNFL (diffuse RNFL defect; localized RNFL defect; no RNFL defect; unidentifiable RNFL status) based on baseline RNFL photographs. Reference standard of glaucoma progression was defined by expert assessment of optic disc/RNFL photographs or VF data. Sensitivity and specificity of OCT GPA, as well as agreement between OCT GPA findings and each reference standard data were estimated.
•RESULTS: Eighteen eyes showed progression by optic disc/RNFL photographs or VF data, while 15 eyes by OCT GPA. When expert assessment of optic disc/RNFL photographs and VF data was used as the reference standard, the sensitivity and specificity of OCT GPA employed to detect glaucoma progression were 38.9% and 70.4%. Agreement between OCT GPA and either optic disc/RNFL photographic evaluation or VF analysis was poor (к=0.211, -0.036 respectively). When expert assessment of optic disc/RNFL photographs was used as the reference standard, 6 eyes were detected progression only by photographs, 2 eyes showed a new disc hemorrhage while 4 eyes with optic disc rim thinning. Among 9 eyes processed only by OCT GPA, 8 eyes were in early stage of POAG, of which 5 eyes had a diffuse RNFL defect and 2 eyes with no RNFL defect at baseline. VF analysis used as the reference standard, 7 eyes were detected progression only by VF testing, of which 5 eyes in advanced stage of POAG. Twelve eyes were processed only by OCT GPA, of which 10 in early stage of POAG.
•CONCLUSION:The Cirrus OCT GPA is more sensitive in eyes with a diffuse RNFL defect and may be useful for progression detection in earlier stage of glaucoma to complement other reference standard strategies.
目的:探讨频域光学相干断层扫描(spectral-domain optical coherence tomography,SD-OCT)的青光眼进展引导分析(guided progression analysis,GPA)技术在判断原发性开角型青光眼(primary open angle glaucoma,POAG)进展中的作用。
方法:随访36例45眼POAG患者2a,行视盘OCT、眼底照相及视野检查,至少有4次可信的OCT检查结果。根据视野结果将受试者划分为早期和中晚期。根据基线眼底照相判断视网膜神经纤维层(retinal nerve fiber layer,RNFL)情况(弥漫RNFL缺损、局限缺损、无缺损及无法判断缺损者)。由两位青光眼专家根据眼底照相及视野结果将其分为进展型及非进展型。分析OCT-GPA技术同视野、眼底照相判断的一致性,计算灵敏度及特异度。
结果:眼底照相或视野判断为POAG进展者18眼(40%),OCT-GPA判断POAG进展者15眼(33%)。以眼底照相及视野判断为标准,OCT-GPA技术的灵敏度和特异度为38.9%和70.4%。OCT-GPA同眼底照相及视野判断结果的一致性较差(к=0.211、-0.036)。以眼底照相为标准,仅眼底照相判断进展者6眼,2眼为新的盘周出血,4眼为盘沿变窄;仅OCT-GPA判断为进展者9眼,8眼为早期,其中5眼基线眼底照相提示弥漫性RNFL缺损,2眼无明显RNFL缺损。以视野为判断标准,仅视野判断进展者7眼,5眼为中晚期;仅OCT-GPA判断进展者12眼,10眼为早期。
结论:OCT-GPA在判断早期POAG进展及弥漫性RNFL缺损上有一定优势,但最好联合视野及眼底照相检查共同判断。
光学相干断层扫描;原发性开角型青光眼;青光眼进展分析;眼底照相
引用:关新辉,李丽,梁勇. OCT-GPA技术在监测原发性开角型青光眼进展中的作用.国际眼科杂志2016;16(9):1687-1691
0引言
原发性开角型青光眼是一组具有特征性视网膜神经纤维损害和视野缺损的进行性致盲性眼病。起病及进展隐匿,损害多不可逆,有效的病情监测对原发性开角型青光眼(primary open angle glaucoma,POAG)患者管理极为重要。全面准确判断POAG进展情况应同时行结构性及功能性检查[1]。视野是目前较公认的功能性判断指标,许多大型多中心青光眼临床试验均以此为标准[2-4],但其有一定的滞后性、主观性及波动性。眼底照相为结构性定性判断,专家意见亦可存在较明显的差异[5-6]。目前尚无判断青光眼进展的结构性金标准。光学相干断层扫描作为一种非接触性、非侵入性、高分辨率的生物组织结构显像技术,已成为青光眼眼底结构客观定量检测的重要方法[7-10]。文献报道其不仅有助于POAG的早期诊断,更可用于监测青光眼进展[11-17]。光学相干断层扫描成像青光眼进展引导分析技术(optical coherence tomography-guided progression analysis,OCT-GPA)技术通过追踪视网膜神经纤维层(retinal nerve fiber layer,RNFL)厚度序列变化,自动排列比较基线及随访图像,像素比对,提供可视化的RNFL变化区域及RNFL厚度变化数值,从而判断青光眼进展情况。
目前对OCT-GPA判断青光眼进展诊断效能的相关文献报道较少,本研究拟对POAG患者随访视盘OCT,利用OCT-GPA技术判断进展情况,以视野及眼底照相判断结果为标准,计算OCT-GPA技术的灵敏度及特异度,评价其诊断效能及分析优劣势。
1对象和方法
1.1对象纵向研究。选取2013-01/2015-08我院眼科门诊就诊并确诊的36例45眼POAG患者。此项研究遵循赫尔辛基宣言中的伦理学标准,并经医院临床研究伦理委员会同意,所有参与者均为自愿,对检测予以认可并签署了知情同意书。所有POAG患者均进行了全面的眼科检查,包括视力、非接触性眼压、裂隙灯及前置镜下眼底检查、屈光度、前房角检查。POAG诊断标准:(1)至少2次眼压>21mmHg(1mmHg=0.133kPa);(2)房角镜检查前房角开放;(3)青光眼性视乳头损害和/或视网膜神经纤维层缺损;(4)青光眼性视野缺损。具有(1)、(2)项与(3)或(4)方可诊断成立。纳入标准为:最佳矫正视力不低于0.5,球镜-6.00~+3.00D,无可能影响视网膜的全身及眼部其他疾患,1a内无眼部手术及眼内激光史。采用Hodapp等1993年建议的HPA国际视野分期法分期,将受试者分为早期及中晚期。早期包括初期和早期POAG,中晚期包括中期和晚期POAG。所有POAG患者治疗方案均参见《我国原发性青光眼诊断和治疗专家共识(2014年)》,随访期间均为药物治疗调整,无接受手术及激光者。
1.2方法受试者均行视盘眼底照相、Humphrey视野(中心30-2程序)及视盘OCT(Cirrus HD-OCT,Carl Zeiss Meditec,Dublin,CA)检查,各项检查间隔时间在1wk内,随访2a,OCT至少有4次可信结果。
1.2.1眼底照相眼底照相为对视盘20°范围照相及RNFL 45°范围无赤光照相。在患眼散瞳后,由技术熟练的同一技师采用眼底彩色照相机获取。两位青光眼专家采用双盲法独立评估基线眼底照相,将受试者分为弥漫性RNFL缺损、局限楔状缺损、无明显RNFL缺损及不确定RNFL缺损者。弥漫及局限楔状缺损混合者划为弥漫性缺损。不确定RNFL缺损多因为盘周色素沉着及绝对期青光眼。两位青光眼专家采用双盲法独立评估2a内眼底照相结果,判断青光眼进展与否及注明判断依据。当意见不一致时,以第三位青光眼专家判断为准。眼底照相中盘沿变窄、RNFL缺损增宽加深或出现新的RNFL缺损、新的盘周出血判定为青光眼进展[18-20]。
1.2.2视野视野采用Humphery自动视野计,中心30-2程序。所有受试者均有两次以上视野检查经验,第1次正式检查,至少行3次检查,每次间隔至少30min,取最近一次检查的视野结果。各次视野检查均在相同条件下由同一视野师进行操作。符合以下条件认为视野结果可信:注视丢失<20%、假阳性率和假阴性率<30%;视野缺损的位置和视盘损害的位置相对应。两位青光眼专家采用双盲法独立评估2a内视野结果,判断青光眼进展情况。意见不一致时以第3位青光眼专家判断为准。视野进展标准:(1)基线暗点范围内两个或两个以上的暗点加深10dB;(2)暗点扩大:两个或两个以上加深10dB的位点与基线暗点相连;(3)出现新的暗点:基线暗点范围内或者与基线暗点相邻的两个或更多位点出现缺损,其模式偏差概率P值=1%;或者视野中心10°内之前正常的位点敏感度下降10dB。以上改变,在同一位点至少有一种改变在以后两次或三次连续随访视野结果中出现,则认为青光眼可能或极可能进展[21]。
1.2.3视盘OCT检查所有受试者均进行Cirrus HD-OCT检查。扫描模式为“optic disc cube mode”,为6mm×6mm×2mm立体扫描,分析计算直径3.46mm圆周上的RNFL平均、象限及钟点厚度。信号强度≥5并无眨眼、头位等引起假阳性结果等认为结果可信。均进行GPA分析。各次检查均在同一条件下由同一熟练技师操作。GPA分析时要求核对眼别、采用可信结果比较。Cirrus SD-OCT GPA技术分析内容包括视网膜神经纤维层厚度地图(RNFL thickness maps)、神经纤维层厚度散点图(RNFL thickness value)及神经纤维层厚度折线图(RNFL thickness profiles),见图1。本研究中可能进展(Possible Progression)和极可能进展(Likely Progression)均视为青光眼进展。

图1Cirrus HD-OCT RNFL GPA随访报告A:视网膜神经纤维层厚度地图;B:神经纤维层厚度散点图;C:神经纤维层厚度折线图。
表1受试者一般情况

参数总数早期中晚期眼数452916进展眼数1899年龄(x±s,岁)63.7±14.165.3±13.861.0±15.6球镜度数(x±s,D)-0.9±2.2-0.7±2.0-1.3±2.6OCT信号强度(x±s)7.2±0.77.1±0.57.4±0.9平均MD(x±s,dB)-7.5±5.6-3.8±2.3-11.9±7.2平均PSD(x±s,dB)±6.01.8±0.512.3±3.9基线平均RNFL厚度(x±s,μm)71.3±18.978.0±15.361.3±16.5基线平均RNFL厚度(进展型,x±s,μm)68.9±15.277.5±14.960.2±13.1基线平均RNFL厚度(非进展型,x±s,μm)72.1±16.778.9±16.162.8±17.12a后平均RNFL厚度(x±s,μm)70.2±16.375.8±14.859.1±18.42a后平均RNFL厚度(进展型,x±s,μm)66.9±17.474.1±16.758.7±15.42a后平均RNFL厚度(非进展型,x±s,μm)71.6±16.576.8±15.860.1±18.3
统计学分析:采用SPSS 22.0统计软件,以眼底照相和/或视野判断青光眼进展为标准,对OCT-GPA判断数据进行配对卡方检验,计算OCT-GPA技术灵敏度、特异度及Kappa值。以P≤0.05为差异具有统计学意义。
2结果
2.1受试者一般情况本研究共36例45眼受试者,女20例20眼(44%),平均随访2.1±0.3a,平均间隔时间为0.62(0.60~0.68)a,见表1。
2.2眼底照相/视野判断POAG进展情况患者18眼被判断为青光眼进展,其中早期9眼、中晚期9眼。早期组中,眼底照相判断者8眼,视野判断者4眼,两者一致者3眼。中晚期组中,眼底照相判断者4眼,视野判断者6眼,两者一致者1眼。
表2各组受试者基线信息

检查判断进展情况仅OCT-GPA仅视野和/或眼底照相tP眼数811年龄(x±s,岁)64.8±14.562.7±14.20.3040.765球镜度数(x±s,D)-1.0±0.5-1.2±1.10.4370.668OCT信号强度(x±s)7.2±0.47.3±0.8-0.3000.768平均MD(x±s,dB)-4.8±2.6-10.0±5.12.7010.015平均PSD(x±s,dB)3.8±3.68.3±4.5-2.3420.032平均RNFL厚度(x±s,μm)76.4±11.562.4±9.92.8490.011
表3OCT-GPA技术和不同判断标准的一致性分析

OCT-GPA技术眼底照相视野眼底照相及视野灵敏度50.0%30.0%38.9%特异度72.7%65.7%70.4%χ21.1510.0000.104P0.2831.0000.747κ值(SE)0.211(0.152)-0.036(0.141)0.095(0.149)早期κ值(SE)0.253(0.177)0.054(0.147)0.336(0.176)中晚期κ值(SE)0.091(0.262)-0.037(0.220)-0.159(0.187)
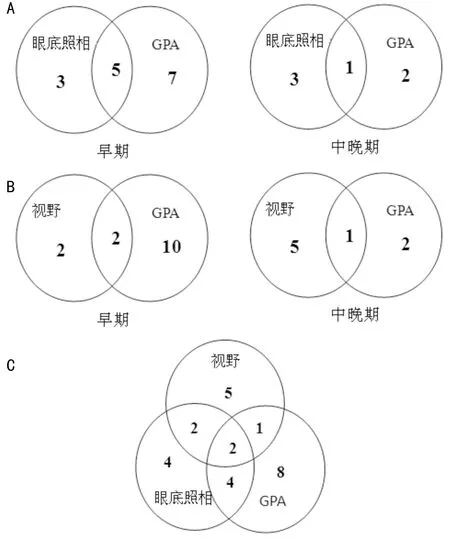
图2眼底照相/视野和OCT-GPA判断POAG进展情况A:眼底照相与GPA判断POAG进展一致性分布情况;B:视野与GPA判断POAG进展一致性分布情况;C:眼底照相、视野与GPA判断POAG进展一致性分布情况。
2.3 OCT-GPA判断POAG进展情况OCT-GPA共判断15眼为青光眼进展,其中早期12眼、中晚期3眼。同眼底照相及视野结果一致性详见图2。26眼被至少3种检查中的一种判断为青光眼进展。8眼仅OCT-GPA判断为进展,11眼仅视野和/或眼底照相判断进展,9眼被3种检查中至少2种判断为进展。其各组基线信息见表2。仅由眼底照相和/或视野判断进展的受试者基线视功能情况更差。
2.4 OCT-GPA同视野、眼底照相一致性分析以眼底照相及视野结果为判断标准,OCT-GPA技术总体判断POAG进展的灵敏度、特异度分别为38.9%和70.40%,Kappa值为0.095,一致性差。单项检查为判断标准,OCT-GPA同眼底照相早期组一致性最佳(κ值=0.253)。OCT-GPA技术和不同判断标准的一致性详见表3。
3讨论
青光眼病理损害基础是视网膜神经节细胞及其轴突(神经纤维)的进行性损害,通常表现为视盘形态和RNFL厚度的改变[22]。当视网膜神经节细胞凋亡达到30%以上,方出现临床上可以检测到的视野缺损[23]。青光眼进展可以是结构性和(或)功能性的改变[24]。SD-OCT因其更快的扫描速率、更高的分辨率及眼球追踪技术,检查结果有较好的可重复性,目前正越来越多地被应用于青光眼诊断和病情进展监测[25]。Cirrus HD-OCT GPA技术是2009年引入配置,通过追踪RNFL序列变化,自动排列比较基线及随访图像,像素比对,提供可视化的RNFL变化区域及RNFL厚度变化数值,从而判断青光眼进展情况[25]。
本组研究中,分别以眼底照相、视野、眼底照相及视野为参考标准,三组P值均大于0.05,提示OCT-GPA技术同视野及眼底照相判断POAG进展检出率无显著性差异。OCT-GPA同眼底照相、视野之间一致性均较差(κ值=0.211、-0.036)。进一步亚型分析中,单项检查为判断标准,OCT-GPA同眼底照相早期组一致性最佳(κ值=0.253),而仅由眼底照相或视野判断进展的受试者基线视功能情况更差。
以眼底照相为判断标准,仅眼底照相判断进展者6眼,2眼为新的盘周出血,4眼为盘沿变窄。考虑盘周出血,OCT-GPA无法识别,同时出血引起神经纤维层水肿,反而出现RNFL厚度增厚,故OCT-GPA判断为假阴性。4眼盘沿变窄,其中3眼为中晚期,OCT-GPA均未能识别,考虑同中晚期RNFL厚度已明显变薄,盘沿变窄,RNFL厚度变化未能让OCT-GPA识别可能。提示OCT-GPA技术在中晚期POAG盘沿变化方面识别度较差。Jong等应用Cirrus SD-OCT GPA发现其对于视盘形态改变灵敏度低,分析同其侧重RNFL厚度测量相关[26],本研究结果符合其发现。同时,仅OCT-GPA判断为进展者9眼,1眼为中晚期,其基线眼底照相为不确定RNFL缺损者,因绝对期青光眼无法判断RNFL缺损。8眼为早期,其中5眼基线眼底照相提示为弥漫性RNFL缺损,2眼无明显RNFL缺损。考虑可能因弥漫性RNFL缺损,眼底照相不易判断,而OCT在测量RNFL厚度方面有定量优势,推测OCT-GPA在判断早期弥漫性RNFL缺损类型的POAG进展方面有一定优势,但上述病例仍需较长时间大样本观察,也不排除OCT-GPA假阳性可能。6眼眼底照相及OCT-GPA判断一致,其中5眼为早期,提示OCT-GPA可能在判断早期POAG进展上有一定优势。
以视野为判断标准,仅视野判断进展者7眼,5眼为中晚期,考虑可能因中晚期RNFL厚度已明显变薄,即使出现阳性的视野恶化,RNFL厚度改变仍不足以被OCT-GPA识别可能,该表现也同OCT-GPA对中晚期POAG盘沿变化识别度欠佳相一致。同时,仅OCT-GPA判断进展者12眼,10眼为早期。考虑同OCT更易识别RNFL厚度,即使尚未出现明显可检测出的视野改变,而OCT-GPA提前监测到RNFL厚度改变。同时并不排除OCT-GPA假阳性可能,尚需更长时间大样本随访评估。
另有病例报道[27],2例病例进行OCT-GPA分析中,1例随访分析图像中出现了对侧眼图像,另1例出现了其他患者的眼底图像,而这2例均未发现明显硬件及操作问题。本组研究中未出现眼别匹配错误。本研究的局限在于受试者数量较少,随访时间短,许多推断尚需大样本和长期临床研究的评价结果。
综上所述,本研究提示OCT-GPA技术更易判断早期POAG进展,对中晚期POAG进展识别欠佳。判断弥漫性RNFL缺损、不确定RNFL缺损变化上有一定优势,对新的盘周出血及盘沿变窄识别欠佳。OCT-GPA在判断早期POAG进展有一定优势,但最好联合视野及眼底照相检查共同判断。
1 Tenkumo K, Hirooka K, Baba T,etal.Evaluation of relation between retinal nerve fiber layer thickness progression and visual field progression in patients with glaucoma.JpnJOphthalmol2013;57(5):451-456
2 Anderson DR, Drance SM, Schulzer M,etal. Natural history of normal-tension glaucoma.Ophthalmology2001;108(2):247-253
3 Musch DC,Lichter PR,Guire KE,etal.CIGTS Study Group.The Collaborative Initial Glaucoma Treatment Study:study design,methods,and baseline characteristic of enrolled patient.Ophthalmology1999;106(4):653-662
4 Leske MC,Heijl A,Hyman L,etal.Early Manifest Glaucoma Trial Group.Early Manifest Glaucoma Trial:design and baseline data.Ophthalmology1999;106(11):2144-2153
5 Gaasterland DE, Blackwell B, Dally LG,etal. The Advanced Glaucoma Intervention Study (AGIS): Variability among academic glaucoma subspecialists in assessing optic disc notching.TransAmOphthalmolSoc2001;99:177
6 Jampel HD, Friedman D, Quigley H,etal. Agreement among glaucoma specialists in assessing progressive disc changes from photographs in open angle glaucoma patients.AmJOphthalmol2009;147(1):39-44
7 Burgansky-Eliash Z, Wollstein G, Chu T,etal. Optical coherence tomography machine learning classifiers for glaucoma detection:a preliminary study.InvestOphthalmolVisSci2005;46(11):4147-4152
8 Lalezary M, Medeiros FA, Weinreb RN,etal. Baseline optical coherence tomography predicts the development of glaucomatous change in glaucoma suspects.AmJOphthalmol2006;142(4):576-582
9 Leung CK, Chan WM, Yung WH,etal. Comparison of macular and peripapillary measurements for the detection of glaucoma: an optical coherence tomography study.Ophthalmology2005;112(3):391- 400
10 Manassakorn A, Nouri-Mahdavi K, Caprioli J.Comparison of retinal nerve fiber layer thickness and optic disk algorithms with optical coherence tomography to detect glaucoma.AmJOphthalmol2006;141(1):105-115
11 Wollstein G, Schuman JS, Price LL,etal. Optical coherence tomography longitudinal evaluation of retinal nerve fiber layer thickness in glaucoma.ArchOphthalmol2005;123(4):464-470
12 Medeiros FA, Zangwill LM, Alencar LM,etal. Detection of glaucoma progression with Stratus OCT retinal nerve fiber layer, optic nerve head, and macular thickness measurements.InvestOphthalmolVisSci2009;50(12):5741- 5748
13 Lee EJ, Kim TW, Park KH,etal. Ability of Stratus OCT to detect progressive retinal nerve fiber layer atrophy in glaucoma.InvestOphthalmolVisSci2009;50(2):662-668
14 Leung CK, Cheung CY, Weinreb RN,etal. Evaluation of retinal nerve fiber layer progression in glaucoma: a study on optical coherence tomography guided progression analysis.InvestOphthalmolVisSci2010;51(1):217-222
15 Sung KR, Sun JH, Na JH,etal. Progression detection capability of macular thickness in advanced glaucomatous eyes.Ophthalmology2012;119(2):308-313
16 Grewal DS, Sehi M, Paauw JD,etal. Detection of progressive retinal nerve fiber layer thickness loss with optical coherence tomography using three criteria for functional progression.JGlaucoma2012;21(4):214-220
17 Na JH, Sung KR, Baek S,etal. Detection of glaucoma progression by assessment of segmented macular thickness data obtained using spectral domain optical coherence tomography.InvestOphthalmolVisSci2012;53(7):3817-3826
18 Drance S, Anderson DR, Schulzer M,etal.Risk factors for progression of visual field abnormalities in normal-tension glaucoma.AmJOphthalmol2001;131(6):699-708
19 Nitta K. Disc hemorrhage is a sign of progression in normal tension glaucoma.JGlaucoma2012;21(4):276
20 Sung KR. Disc hemorrhage: is that a risk factor or sign of progression?JGlaucoma2012;21(4):275-276
21 Asman P,Wild JM,Heijl A.Appearance of the pattern deviation map as a function of change in area of localized field loss.InvestOphthalmolVisSci2004;45(9):3099-3106
22 Weinreb RN, Khaw PT. Primary open-angle glaucoma.TheLancet 2004;363(9422):1711-1720
23李美玉.青光眼学.北京:人民卫生出版社 2004:225-226
24 Kemgan-Banmrind LA,Quigley HA,Pease ME,etal.Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons.InvestOphthalmoIVisSci2000;41(3):741-748
25 Grewal DS, Tanna AP. Diagnosis of glaucoma and detection of glaucoma progression using spectral domain optical coherence tomography.CurrOpinOphthalmol2013;24(2):150-161
26 Lee JR, Sung KR, Na JH,etal. Discrepancy between optic disc and nerve fiber layer assessment and optical coherence tomography in detecting glaucomatous progression.JpnJOphthalmol2013;57(6):546-552
27 Kennedy JB, SooHoo JR, Seibold LK,etal.Misguided progressin analysis by optical coherence tomography:a report of two cases.CaseRepOphthalmol2014;5(2):217-221
Clinical role of Cirrus optical coherence tomography-guided progression analysis in detecting glaucomatous progression
Xin-Hui Guan, Li Li, Yong Liang
Special Scientific Research Foundation for Young Scientific and Technological Talents of Health and Family Planning Commission of Xinjiang Uygur Autonomous Region (No.2014Y10)
2016-05-23Accepted:2016-08-08
•spectral-domain optical coherence tomography; primary open angle glaucoma; guided progression analysis; optic disc photography
2014年度新疆维吾尔自治区卫生厅青年科技人才专项科研项目(No.2014Y10)
(830054)中国新疆维吾尔自治区乌鲁木齐市,新疆医科大学第五附属医院眼科
关新辉,女,毕业于新疆医科大学,硕士,副主任医师,研究方向:白内障、青光眼。
梁勇,男,硕士,主任医师,主任.iohey@163.com
2016-05-23
2016-08-08
Guan XH, Li L, Liang Y. Clinical role of Cirrus optical coherence tomography-guided progression analysis in detecting glaucomatous progression.GuojiYankeZazhi(IntEyeSci) 2016;16(9):1687-1691
10.3980/j.issn.1672-5123.2016.9.22
