左室四极电极在心脏再同步化治疗中的优势
2016-07-18王紫苏立
王 紫 苏 立
左室四极电极在心脏再同步化治疗中的优势
王紫 苏立
400010重庆医科大学附属第二医院心内科
【摘要】成功放置左室起搏电极对于心脏再同步化治疗(CRT/CRT-D)至关重要。与传统起搏电极相比,四极电极具有以下优势:置入成功率较高、能克服膈神经刺激、避免左室高阈值、避免左室心尖部起搏以及导线脱位率较低。
【关键词】心脏再同步化治疗;左室四极电极;心力衰竭
心力衰竭(心衰)是导致60岁以上患者住院及死亡的主要原因[1]。在过去25年中,心脏再同步化治疗(CRT/CRT-D)被广泛用于慢性心衰患者,尤其是伴有左束支传导阻滞及宽QRS波的药物难治性严重心衰。CRT/CRT-D治疗能显著降低心衰患者住院率和死亡率,改善临床症状及生活质量[2-5]。然而,并非所有患者均能从CRT/CRT-D中获益,约有30%的患者对该治疗无反应或无法耐受相关并发症。一项对2 000多例置入CRT/CRT-D患者6个月的随访研究显示,约有8%的患者因并发症需要再次手术[6]。目前认为引起患者对CRT/CRT-D无反应的主要原因有:未严格掌握适应证;患者冠状窦静脉解剖结构与电极不匹配;非最佳左室起搏位点的选择等。既往研究发现,置入传统左室电极可出现以下并发症:不能耐受的膈神经刺激;逐渐增高的左室起搏阈值;电极脱位等[7-14]。上述并发症增加了患者手术时间、感染风险、术者及患者射线暴露时间以及二次手术的风险[9]。Champagne等[11]通过对228例置入双极电极CRT患者的随访研究发现,调整起搏配置可以降低起搏阈值,减少膈神经刺激,并能降低再次手术发生率,但仍有20%的患者出现并发症[15]。
新型左室四极电极直径约4.7 F,它由1个4.0 F的尖端电极(D1)和距电极尖端20、30、47 mm的3个环形电极(M2、M3、P4)组成(见图1)[16]。4个电极与右室环形电极作为阴极,其中2个电极(M2和P4)同时作为阳极,可组合形成10种起搏配置。传统双室起搏仅能提供3种起搏配置,四极电极为术者提供了更多的选择,同时可以更加灵活地选择左室起搏向量,从而极大地减少了膈神经刺激、左室阈值增高、左室心尖部起搏及导线脱位等可能导致CRT/CRT-D置入失败的因素,因此能增加患者对治疗的反应性,提高疗效[9,17-18]。

图1 四极电极示意图
1膈神经刺激
为了避免左室电极移位,通常会选择将电极放置得更靠近心尖部,但却导致电极与膈神经或膈肌紧贴, CRT/CRT-D发放电冲动时易刺激膈神经,引起膈肌跳动,临床上表现为随CRT/CRT-D工作出现呃逆,称为膈神经刺激[8,10-13],发生率约为13%~37%[7,10,18],其中需行二次手术或关闭CRT/CRT-D的发生率为1%~13%[7-11,14,16]。目前,减少膈神经刺激的方法有:减少左室起搏电极输出电量;重新放置左室电极;外科放置心外膜电极;关闭CRT/CRT-D[9]。上述方法均限制了CRT/CRT-D的临床运用。Biffi等[19]纳入1 307例置入左室电极的患者,平均随访14.9个月,结果显示,膈神经刺激与左室电极尖端放置的位置及起搏配置的选择有显著关系;左室电极尖端放置的位点可作为膈神经刺激的独立预测因子;心尖部及侧或侧后中段左室起搏位点的膈神经刺激发生率较高,而基底部起搏则明显降低。
四极电极可提供多达10种起搏配置,通过选择不同的起搏配置而尽可能实现基底部起搏,从而避免膈神经刺激[20-22]。除电极因素外,患者手术时的体位等因素也可导致膈神经刺激,因此降低了在术中即发现膈神经刺激的敏感性。大量研究,包括术中研究、随访3~6个月的短期调查,以及一项长达5年的长期研究证实,四极电极能有效减少膈神经刺激的发生[23-27]。
2电极稳定性
对于传统双室起搏电极,为避免出现膈神经刺激,通常将电极放置在靠近心底部,可能增加电极移位风险。传统电极移位率约为6%~14%[28-30]。四极电极直径比传统电极小;其同一导线上的4个电极可将电极放置在更靠近心尖部,保证电极的稳定性;通过激动近心端电极,可实现从左室中间部或基底部起搏而避免心尖部起搏,从而在最大程度上避免膈神经刺激[7,18]。Forleo等[17]一项前瞻性多中心研究对154例置入四极电极CRT/CRT-D的患者进行了为期2年的随访,结果表明四极电极有稳定的起搏参数及安全性。在对四极电极与传统双极电极5年的随访研究亦发现,四极电极具有更高的稳定性,更低的移位率;同时,因四极电极给术者提供更多的选择,使其置入成功率更高(95%~100%)[23,31],并能维持稳定的起搏参数[7]。
3避免心尖部起搏
正如上述,对于传统电极,为了避免出现电极随心脏搏动而从冠状窦静脉系统脱出或者为了获得更稳定的夺获阈值,增加电极的稳定性,术中常选择将电极放置到靠近心尖部[17]。然而,MADIT-CRT研究表明,与心底部起搏相比,采用心尖部起搏的心衰患者的住院率及死亡率明显增高[32]。
四极电极可以满足将电极放置在更靠近心尖部保证其稳定性,而通过调整起搏配置,实现心底部起搏[9,17-18]。Behar等[27]对721例置入CRT/CRT-D患者为期5年的随访研究证实,置入四极电极患者的死亡率较双极电极低(13.2% 对22.5%,P<0.001)。
4避免起搏阈值逐渐增加
电极起搏阈值的逐渐增加一般与电极放置位点有关。使用传统电极时,术者为避免膈神经刺激及心尖部起搏,会将电极放置于近心端,导致起搏阈值随时间逐渐增加,最终导致缩短电池寿命及起搏失败[7,9]。四极电极可将电极放置更靠近心尖部,同时其灵活可变的多种起搏配置,可增加电极稳定性,并能选择最佳起搏位点,避免起搏阈值的逐渐增高[7,9,17-18]。与传统电极相比,四极电极的起搏阈值及阻抗更低,且其夺获左室阈值也较低,提高了电极使用寿命[27-28]。
四极电极的置入成功率达96%~100%,能明显减少术中及术后的电极相关并发症 ,并有利于在冠状窦静脉系统找到最佳电极放置位点,缩短手术时间及减少费用,降低二次手术风险。此外,四极电极能使血流动力学及心功能改善更明显[33]。
5四极电极的新进展
新型“短双极电极”在传统四极电极的基础上进一步改进。该导线远端电极与第二个电极之间以及第三个电极与近端电极之间的距离为21 mm,而中间两个电极之间的距离是1.3 mm,且导线形态不同(见图2),能提供多达16种起搏配置。Crossley等[31]对1 124例置入新型四极电极患者为期至少半年的研究发现,该类型的四极电极具有高置入成功率(97.6%)、低电极移位率(1.4%)、低膈神经刺激发生率(7.2%)及稳定的夺获阈值,其中97%的电极并发症可通过非侵入性治疗得到解决。

图2 短双极电极示意图
因冠状窦静脉的解剖结构不同,且随着冠状静脉向远心端走行,其管径越来越小。因此即使增加同一导线的电极数量,也不能完全实现其与冠状静脉壁的完全贴壁,将导致夺获阈值的明显增加。最近研发的一种新型3D螺旋四极电极已被证实可获得稳定的、低于2.5 V的起搏阈值。该电极管腔直径为5.2 F,尖端直径为2.6 F,由笔直的尖端电极及其后具有3D螺旋形态的3个电极组成,更易将电极放置在心尖部,可增加电极的稳定性。该电极特殊的螺旋结构使其更易贴靠管腔壁,获得更稳定的起搏阈值(见图3)[34]。
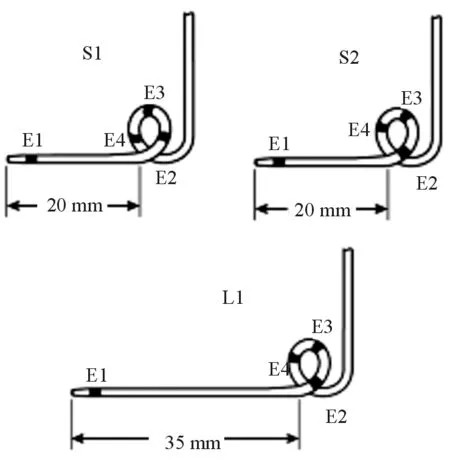
图3 3D螺旋电极示意图
虽然也有个别研究报道,通过四极电极无法减少膈神经刺激、高起搏阈值等并发症[35],但四极电极仍有着极大的临床应用空间。
参考文献
[1]Eriksson H. Heart failure: a growing public health problem[J]. J Intern Med,1995,237(2):135-141.
[2]Cleland JG, Daubert JC, Erdmann E, et al.Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure[J]. N Engl J Med,2005,352(15):1539-1549.
[3]Abraham WT, Fisher WG, Smith AL,et al. Cardiac resynchronization in chronic heart failure[J]. N Engl J Med,2002,346(24):1845-1853.
[4]Moss AJ,Hall WJ,Cannom DS,et al.Cardiac-resynchronization therapy for the prevention of heart-failure events[J]. N Engl J Med,2009,361(14):1329-1338.
[5]朱华,张瑜,邱建平. 心脏再同步化治疗充血性心力衰竭的临床分析[J].国际心血管病杂志,2010,37(5),304-305.
[6]Leon R,Abraham WT,Curtis AB,et al.Safety of transvenous cardiac resynchronization system implantation in patients with chronic heart failure: combined results of over 2,000 patients from a multicenter study program[J]. J Am Coll Cardiol,2005,46(12):2348-2356.
[7]Forleo GB, Della Rocca DG, Papavasileiou LP,et al.Left ventricular pacing with a new quadripolar transvenous lead for CRT: early results of a prospective comparison with conventional implant outcomes[J]. Heart Rhythm,2011,8(1):31-37.
[8]Biffi M, Moschini C, Bertini M,et al.Phrenic stimulation:a challenge for cardiac resynchronization therapy[J]. Circ Arrhythm Electrophysiol,2009,2(4):402-410.
[9]Tomassoni G,Baker J,Corbisiero R,et al.Postoperative performance of the quartet left ventricular heart lead[J].J Cardiovasc Electrophysiol,2013,24(4):449-456.
[10]Gurevitz O,Nof E, Carasso S,et al.Programmable multiple pacing configurations help to overcome high left ventricular pacing thresholds and avoid phrenic nerve stimulation[J].Pacing?Clin Electrophysiol,2005,28(12):1255-1259.
[11]Champagne J, Healey JS, Krahn AD,et al. The effect of electronic repositioning on left ventricular pacing and phrenic nerve stimulation[J].Europace,2011,13(3):409-415.
[12]Thibault B, Krst E, Ryu K,et al. Pacing electrode selection in a quadripolar left heart lead determines presence or absence of phrenic nerve stimulation[J].Europace,2010,12(5):751-753.
[13]Biffi M, Boriani G. Phrenic stimulation management in CRT patients: are we there yet? [J]. Curr Opin Cardiol,2011,26(1):12-16.
[14]Uslan DZ, Gleva MJ, Warren DK, et al. Cardiovascular implantable electronic device replacement infections and prevention: results from the REPLACE Registry[J]. Pacing Clin Electrophysiol,2012,35:81-87.
[15]Klein N, Klein M, Weglage H,et al.Clinical efficacy of left ventricular pacing vector programmability in cardiac resynchronization therapy defibrillator patients for management of phrenic nerve stimulation and/or elevated left ventricular pacing thresholds: insights from the Efface Phrenic Stim study[J].Europace,2012,14(6):826-832.
[16]Shetty AK,Duckett SG,Bostock J,et al.Initial single-center experience of a quadripolar pacing lead for cardiac resynchronization therapy[J]. Pacing Clin Electrophysiol,2011,34(4):484-489.
[17]Forleo GB,Mantica M,Di Biase L,et al.Clinical and procedural outcome of patients implanted with a quadripolar left ventricular lead: Early results of a prospective multicenter study[J]. Heart Rhythm,2012,9(11):1822-1828.
[18]Mehta PA, Shetty AK, Squirrel M,et al. Elimination of phrenic nerve stimulation occurring during CRT: follow-up in patients implanted with a novel quadripolar pacing lead[J]. J Interv Card Electrophysiol,2012,33(1):43-49.
[19]Biffi M, Exner DV, Crossley GH,et al.Occurrence of phrenic nerve stimulation in cardiac resynchronization therapy patients: The role of left ventricular lead type and placement site[J]. Europace,2013,15(1):77-82.
[20]Seifert M, Schau T, Moeller,et al. Influence of pacing configurations, body mass index, and position of coronary sinus lead on frequency of phrenic nerve stimulation and pacing thresholds under cardiac resynchronization therapy[J]. Europace,2010,12(7):961-967.
[21]Jastrzebski M, Bacior B, Wojciechowska W,et al.Left ventricular lead implantation at a phrenic stimulation site is safe and effective[J]. Europace,2011,13(4):520-525.
[22]Sperzel J,Dänschel W,Gutleben KJ,et al. First prospective, multi-centre clinical experience with a novel left ventricular quadripolar lead[J].Europace,2012,14(3):365-372.
[23]Arias MA, Pachón M, Puchol A, et al.Acute and mid-term outcomes of transvenous implant of a new left ventricular quadripolar lead versus bipolar leads for cardiac resynchronization therapy: results from a single-center prospective database[J].Cardiol J,2012,19(5):470-478.
[24]Biffi M, Bertini M, Ziacchi M,et al.Management of phrenic stimulation in CRT patients over the long term: still an unmet need?[J]. Pacing Clin Electrophysiol,2011,34(10):1201-1208.
[25]Biffi M, Bertini M, Saporito D, et al.Automatic management of left ventricular stimulation: hints for technologic improvement[J].Pacing Clin Electrophysiol,2009,32(3):346-353.
[26]Burri H, Gerritse B, Davenport L,et al. Fluctutations of left ventricular threshold and required safety margin for left ventricular pacing with cardiac resynchronization therapy[J]. Europace,2009,11(7):931-936.
[27]Behar JM, Bostock J, Zhu Li AP,et al.Cardiac resynchronization therapy delivered via a multipolar left ventricular lead is associated with reduced mortality and elimination of phrenic nerve stimulation: long-term follow-up from a multicenter registry[J].J Cardiovasc Electrophysiol,2015,26(5):540-546.
[28]折剑青,袁祖贻.心脏再同步化治疗的自动阈值管理功能[J].国际心血管病杂志,2014,41(3):148-150.
[29]Alonso C, Leclercq C, D’Allonnes FR, et al. Six year experience of transvenous left ventricular lead implantation for permanent biventricular pacing in patients with advanced heart failure: technical aspects[J].Heart,2001,86(4):405-410.
[30]Valls-Bertault V, Mansourati J, Gilard M, et al. Adverse events with transvenous left ventricular pacing in patients with severe heart failure: early experience from a single centre[J]. Europace,2001,3(1):60-63.
[31]Crossley GH, Biffi M, Johnson B, et al.Performance of a novel left ventricular lead with short bipolar spacing for cardiac resynchronization therapy: primary results of the Attain Performa quadripolar left ventricular lead study[J].Heart Rhythm,2015,12(4):751-758.
[32]Singh JP, Klein HU, Huang DT,et al.Left ventricular lead position and clinical outcome in the multi-center automatic defibrillator implantation trial cardiac resynchronization therapy (MADIT-CRT) trial[J].Circulation,2011,123(11):1159-1166.
[33]Asbach S, Hartmann M, Wengenmayer T, et al.Vector selection of a quadripolar left ventricular pacing lead affects acute hemodynamic response to cardiac resynchronization therapy: a randomized cross-over trial[J].PLoS One,2013,8(6):e67235.
[34]Philippon F,Liu L,Fung JW,et al.Left ventricular three-dimensional quadripolar lead acute clinical study: the LILAC study[J].Pacing Clin Electrophysiol,2015,38(4):438-447.
[35]Parahuleva MS, Chasan R, Soydan N,et al.Quadripolar left ventricular lead in a patient with CRT-D does not overcome phrenic nerve stimulation[J].Clin Med Insights Cardiol,2011,5:45-47.
(收稿:2015-11-25修回:2015-12-29)
(本文编辑:丁媛媛)

doi:10.3969/j.issn.1673-6583.2016.03.006
