高血压患者夜间血压变化与颅内动脉粥样硬化狭窄的相关性
2016-06-03廖光昊黎红华
崔 敏 濮 捷 廖光昊 吴 乐 吴 倩 武 强 黎红华
广州军区武汉总医院神经内科 武汉 430070
高血压患者夜间血压变化与颅内动脉粥样硬化狭窄的相关性
崔敏濮捷廖光昊吴乐吴倩武强黎红华
广州军区武汉总医院神经内科武汉430070
【摘要】目的探讨高血压患者夜间血压变化与颅内动脉粥样硬化狭窄(ICAS)的相关性。方法对高血压患者进行动态血压监测和脑血管磁共振血管成像(MRA)检查。颅内大动脉内径狭窄程度≥50%定义为ICAS,ICAS病灶数≥2定义为多发性ICAS。根据日间与夜间平均血压水平,将昼夜血压变化分为杓型、非杓型、反杓型。结果共359例高血压患者进入本研究:ICAS患者135例,单发性ICAS 86例,多发性ICAS 49例;226例(63.0%)日间平均血压升高,322例(89.7%)夜间平均血压升高;杓型37例(10.3%),非杓型166例(46.2%),反杓型156例(43.5%)。多因素Logistic回归分析提示:日间平均血压升高、夜间平均血压升高、夜间血压非杓型改变、夜间血压反杓型改变均与ICAS无显著相关性(P>0.05);夜间血压反杓型改变与多发性ICAS密切相关(P<0.05)。结论夜间血压反杓型改变可能是多发性ICAS的独立危险因素。
【关键词】高血压;动态血压监测;磁共振血管成像;夜间血压;颅内动脉粥样硬化狭窄
颅内动脉粥样硬化狭窄(intracranial atherosclerotic stenosis,ICAS)在亚洲人群中显著高发,药物预防的效果欠佳。目前,颅内血管介入治疗ICAS尚未在临床广泛开展,因此,探讨ICAS的危险因素、提高预防效果具有重要临床意义。高血压已被证实是ICAS发生、发展的重要危险因素,但既往研究多采用诊室血压这一诊断标准。近期临床研究提示,动态血压较诊室血压能够更可靠地预测心血管事件的发生,尤其是夜间平均收缩压水平升高是风险最高的预测因子[1]。研究[2]证实,夜间平均血压升高与颈动脉粥样硬化密切相关。目前,夜间血压变化与ICAS发生的关系尚不清楚。本研究应用动态血压监测(ambulatory blood pressure monitoring,ABPM)检查,探讨高血压患者夜间血压变化与ICAS发生的相关性。
1对象与方法
1.1研究对象回顾在我院神经内科住院、并完成了动态血压监测和脑血管磁共振血管成像(MRA)检查的高血压患者的临床资料。入选标准:(1)高血压患者;(2)年龄≥40岁;(3)完成了ABPM和MRA检查的患者。排除标准:(1)年龄<40岁;(2)非高血压患者;(3)非动脉粥样硬化性颅内动脉狭窄(动脉夹层、动脉炎、放疗后、烟雾病、颅内占位病变等);(4)病情危重、颅内高压、昏迷、并发严重心肺肝肾功能障碍的患者;(5)未完成ABPM和MRA检查的患者。
1.2颅内动脉检查方法应用1.5T MRI检查颅内大动脉。ICAS定义为大脑中动脉、大脑前动脉、大脑后动脉、颈内动脉颅内段、基底动脉、椎动脉颅内段主干血管内径狭窄程度≥50%[3]。将ICAS病灶数≥2定义为多发性ICAS。采用WASID方法测量颅内动脉狭窄率[4]。
1.3动态血压监测方法应用无创袖带式动态血压监测仪观察患者的24 h血压。24 h平均血压≥130/80 mmHg、日间平均血压≥135/85 mmHg、夜间平均血压≥120/70 mmHg定义为血压升高。根据日间与夜间平均血压水平,将夜间血压变化分为以下几种类型:(1)杓型:夜间平均血压水平低于日间平均血压≥10%;(2)非杓型:夜间平均血压水平低于日间平均血压<10%;(3)反杓型:夜间平均血压水平高于日间平均血压[5]。将发生ICAS的患者分入ICAS组,未发生ICAS的患者分入对照组。

2结果
2.12组临床资料比较2012-10—2014-07共359例高血压病患者进入本研究。男236例,平均年龄(62.1±12.1)岁;女123例,平均年龄(64.8±11.6)岁。ICAS患者135例,单发病灶86例,多发病灶49例(见图1)。ICAS组患者的年龄高于对照组,且糖尿病和血脂异常的发病率高于对照组(P<0.05)。2组性别、冠心病、吸烟方面无显著差异(P>0.05)。见图1。
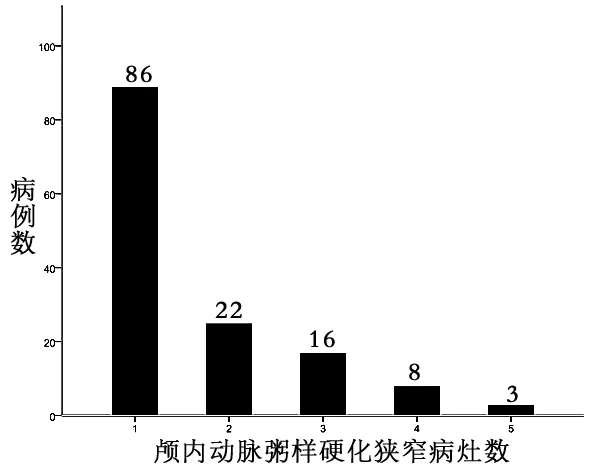
图1 颅内动脉粥样硬化狭窄病灶分布情况
2.22组昼夜血压变化情况比较ICAS组患者的全天平均收缩压、日间平均收缩压、夜间平均收缩压均显著高于对照组,组间平均舒张压无显著差异。2组日间平均血压升高、夜间平均血压升高、夜间血压杓型改变、夜间血压非杓型改变、夜间血压反杓型改变的发生率无显著差异(P>0.05)。见表1。
表1 2组昼夜血压变化情况比较
2.3昼夜血压变化与ICAS发生的相关性分析单因素Logistic回归分析结果提示,日间平均血压升高、夜间平均血压升高、夜间血压非杓型改变、夜间血压反杓型改变均与ICAS的发生无显著相关性(P>0.05)。校正性别、年龄、糖尿病、血脂异常、吸烟、冠心病等因素后,亦得到相似的结果。见表2。
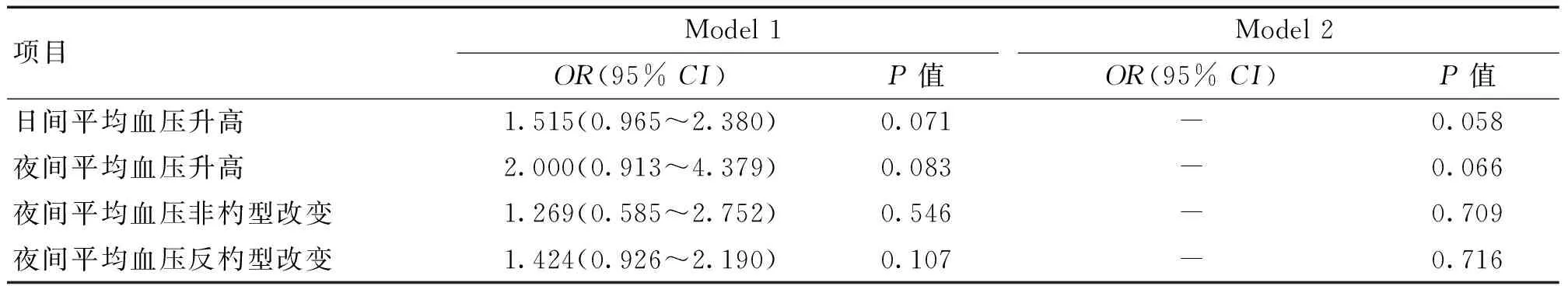
表2 高血压患者昼夜血压变化与ICAS的相关性分析
注:Model 1:未校正混杂因素;Model 2:校正了年龄、性别、糖尿病、血脂异常、吸烟、冠心病等混杂因素
2.4昼夜血压变化与多发性ICAS发生的相关性分析单因素Logistic回归分析结果显示,日间平均血压升高、夜间平均血压升高、夜间血压非杓型改变与多发性ICAS的发生无显著相关性(P>0.05);而夜间血压反杓型改变与多发性ICAS的发生密切相关(P<0.05)。校正性别、年龄、糖尿病、血脂异常、吸烟、冠心病等因素后,亦得到相似的结果。见表3。
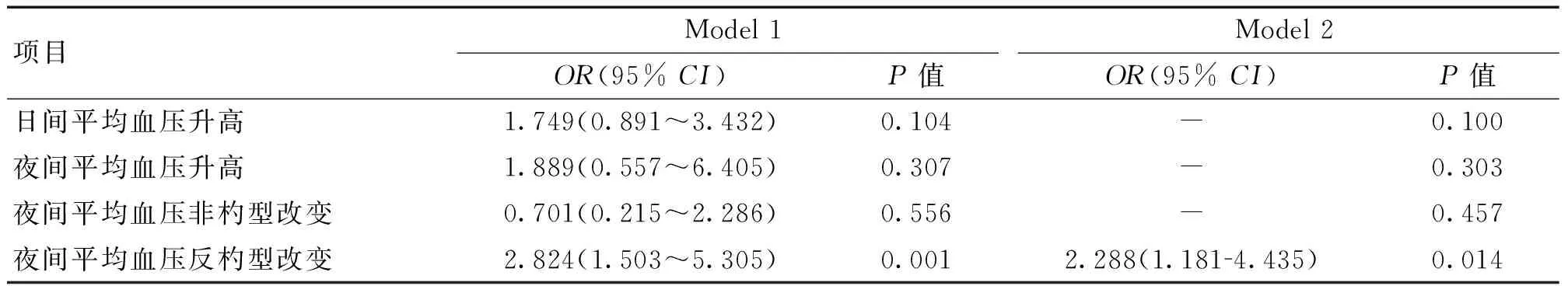
表3 高血压患者昼夜血压变化与多发性ICAS的相关性分析
3讨论
正常人群中昼夜血压呈杓型变化,即夜间血压较日间血压降低10%~20%。在高血压患者中,常出现夜间血压升高,甚至出现非杓型、反杓型昼夜血压变化[6]。本组高血压患者中,夜间血压升高发生率明显高于日间血压升高,夜间血压非杓型、反杓型改变的发生率高达80%以上。
夜间血压升高与心脑血管事件的发生密切相关。Sierra等[7]报道,夜间收缩压升高是发生冠心病和脑卒中的独立预测因素。Mesquita-Bastos等[1]发现,夜间平均收缩压升高患者发生冠心病和脑卒中的风险高于日间平均收缩压升高者,尤其是夜间初始4 h平均收缩压升高者的风险更高。Hermida等[8]报道,降低高血压患者夜间血压水平可以有效降低心血管事件的发生率和病死率。
夜间血压升高也与动脉粥样硬化早期亚临床改变相关。临床研究发现,夜间血压非杓型改变患者的内皮功能损伤显著重于夜间血压杓型改变患者[9]。青少年代谢综合征患者夜间平均收缩压升高与颈动脉内中膜增厚密切相关[10]。中年高血压患者夜间平均血压升高、非杓型改变是颈动脉内中膜增厚的独立预测因素[2]。降低夜间平均血压,使非杓型血压转变为杓型血压,也可能改善颈动脉内中膜增厚[11]。
夜间血压变化与ICAS发生相关性的临床资料很少。史惠霞等[12]报道ICAS患者的夜间平均脉压显著高于对照组患者;而ICAS组与对照组之间,夜间平均血压升高和非杓型的发生率无显著差异。本研究结果也提示,夜间平均血压升高、非杓型和反杓型改变与ICAS的发生无关。但进一步分析提示,多发性ICAS的发生与夜间血压反杓型改变密切相关。由此推断,夜间平均脉压增大可能是颅内动脉早期损伤的重要因素;而夜间血压的反杓型改变则是颅内动脉硬化进展的重要因素。颅内动脉、颈动脉与夜间血压变化的相关性存在着差异,可能与不同研究中动脉硬化标准有所差异有关,也可能提示颅内、颅外动脉对高血压病理损害的反应性存在差异。
本研究结果提示,高血压患者中夜间血压升高、夜间血压非杓型、反杓型改变的发生率高;夜间平均血压升高、夜间血压非杓型改变、夜间血压反杓型改变与ICAS的发生无关;但是,夜间血压反杓型改变可能是多发性ICAS的独立危险因素。
4参考文献
[1]Mesquita-Bastos J,Bertoquini S,Polonia J.Cardiovascular prognostic value of ambulatory blood pressure monitoring in a Portuguese hypertensive population followed up for 8.2years[J].Blood Press Monit,2010,15(5):240-246.
[2]Vasunta RL,Kesaniemi YA,Ylitalo A,et al.Nondipping pattern and carotid atherosclerosis in a middle-aged population: OPERA Study[J].Am J Hypertens,2012,25(1):60-66.
[3]Lopez-Cancio E,Galan A,Dorado L,et al.Biological signatures of asymptomatic extra- and intracranial atherosclerosis: the Barcelona-AsIA (Asymptomatic Intracranial Atherosclerosis) study[J].Stroke,2012,43(10):2712-2719.
[4]Chimowitz MI,Lynn MJ,Howlett-Smith H,et al.Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis[J].N Engl J Med,2005,352(13):1 305-1 316.
[5]Hermida RC,Smolensky MH,Ayala DE,et al.2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension,assessment of cardiovascular and other hypertension-associated risk,and attainment of therapeutic goals[J].Chronobiol Int,2013,30(3):355-410.
[6]Gorostidi M,Sobrino J,Segura J,et al.Ambulatory blood pressure monitoring in hypertensive patients with high cardiovascular risk: a cross-sectional analysis of a 20,000-patient database in Spain[J].J Hypertens,2007,25(5):977-984.
[7]de la Sierra A,Banegas JR,Segura J,et al.Ambulatory blood pressure monitoring and development of cardiovascular events in high-risk patients included in the Spanish ABPM registry: the CARDIORISC Event study[J].J Hypertens,2012,30(4):713-719.
[8]Hermida RC,Ayala DE,Mojon A,et al.Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk[J].J Am Coll Cardiol,2011,58(11):1 165-1 173.
[9]Deyneli O,Yazici D,Toprak A,et al.Diurnal blood pressure abnormalities are related to endothelial dysfunction in patients with non-complicated type 1 diabetes[J].Hypertens Res,2008,31(11):2 065-2 073.
[10]Civilibal M,Duru NS,Elevli M.Subclinical atherosclerosis and ambulatory blood pressure in children with metabolic syndrome[J].Pediatr Nephrol,2014,29(11):2 197-2 204.
[11]赵阳,怀丁.CCB矫正非杓型血压对颈内动脉内中膜厚度的影响[J].中国实用神经疾病杂志,2010,13(21):35-36.
[12]史惠霞,李春兰.老年高血压病患者动态血压与脑动脉粥样硬化的关系[J].中国社区医师,2011,13(13):34.
(收稿2015-05-23)
Association between nocturnal blood pressure and intracranial atherosclerotic stenosis in patients with hypertension
CuiMin,PuJie,LiaoGuanghao,WuLe,WuQian,WuQiang,LiHonghua
DepartmentofNeurology,WuhanGeneralHospitalofGuangzhouMilitaryAreaCommand,Wuhan430070,China
【Abstract】Objective To investigate the relationship between changes of nocturnal blood pressure and presence of intracranial atherosclerotic stenosis (ICAS) in patients with hypertension. Methods The patients with hypertensionc aged ≥ 40 years were enrolled in this study. All subjects underwent ambulatory blood pressure monitoring and magnetic resonance angiography (MRA) of the intracranial vessels. The ICAS was defined as that diameter of the stenosed intracranial large arteries was over 50%. The multi-lesion ICAS was defined as that the number of ICAS lesions was ≥2. According to the daytime and nighttime mean blood pressure (BP) level, the circadian BP pattern was divided into three groups: dipper, non-dipper and inverse-dipper. Results A total of 359 patients with hypertension were enrolled in this study. Of all the 359 patients, 135 patients were classified as the ICAS group, including 86 patients with single-lesion ICAS and 49 patients with multi-lesion ICAS. The daytime mean BP increased in 226 patients (63%), and nocturnal mean BP increased in 322 patients (89.7%). The incidence of dipper, non-dipper and inverse-dipper pattern was 10.3%, 46.2% and 43.5%, respectively. Multivariate Logistic regression analysis showed that the elevated nocturnal mean BP, non-dipper and inverse-dipper pattern were not significantly correlated with the presence of ICAS (P>0.05). However, inverse-dipper pattern was significantly associated with presence of multi-lesion ICAS (P<0.05). Conclusion This study suggests that the inverse-dipper pattern may be an independent risk factor for the presence of multiple lesion ICAS.
【Key words】Hypertension; Ambulatory blood pressure monitoring; Magnetic resonance angiography; Nocturnal blood pressure; Intracranial atherosclerotic stenosis
【中图分类号】R743
【文献标识码】A
【文章编号】1673-5110(2016)08-0014-04
基金项目:湖北省卫生计生科研基金项目(编号:WJ2015Z039)
