Performance on the Functional Movement Screen in older active adults
2016-04-25UlrikeH.Mitchell,A.WayneJohnson,PatR.Vehrs等
Performance on the Functional Movement Screen in older active adults
Ulrike H.Mitchella,*,A.Wayne Johnsona,Pat R.Vehrsa,J.Brent Felanda,Sterling C.HiltonbaDepartment of Exercise Sciences,Brigham Young University,Provo,UT 84602,USAbDepartment of Educational Leadership and Foundations,David O.McKay School of Education,Brigham Young University,Provo,UT 84602,USA
Received 1 November 2014; revised 14 February 2015; accepted 21 April 2015 Available online 17 July 2015
Peer review under responsibility of Shanghai University of Sport.
* Corresponding author.
E-mail address: Rike_mitchell@byu.edu (U.H.Mitchell)
http://dx.doi.org/10.1016/j.jshs.2015.04.006
2095-2546/©2016 Production and hosting by Elsevier B.V.on behalf of Shanghai University of Sport.
Abstract
Background: The Functional Movement Screen (FMS™) has become increasingly popular for identifying functional limitations in basic functional movements.This exploratory and descriptive study was undertaken to confirm feasibility of performing the FMS™in older active adults,assess prevalence of asymmetries and to evaluate the relationship between functional movement ability,age,physical activity levels and body mass index(BMI).Methods: This is an observational study; 97 men (n = 53) and women (n = 44) between the ages of 52 and 83 participated.BMI was computed and self-reported physical activity levels were obtained.Subjects were grouped by age (5-year intervals),BMI (normal,over-weight,and obese) and sex.Each participant’s performance on the FMS™was digitally recorded for later analysis.
Results: The youngest age group (50-54 years) scored highest in all seven tests and the oldest age group (75+) scored lowest in most of the tests compared to all other age groups.The subjects in the“normal weight”group performed no different than those who were in the“overweight”group; both groups performed better than the“obese”group.Of the 97 participants 54 had at least one asymmetry.The pairwise correlations between the total FMS™score and age (r =−0.531),BMI (r =−0.270),and the measure of activity level (r = 0.287) were significant (p<0.01 for all).
Conclusion: FMS™scores decline with increased BMI,increased age,and decreased activity level.The screen identifies range of motion- and strength-related asymmetries.The FMS™can be used to assess functional limitations and asymmetries.Future research should evaluate if a higher total FMS™score is related to fewer falls or injuries in the older population.
©2016 Production and hosting by Elsevier B.V.on behalf of Shanghai University of Sport.
Keywords:Age; BMI; Fitness level; FMS™; Functional fitness; Functional limitations
1.Introduction
Physical functional capacity is an important component of quality of life.1Whether one is a competitive athlete,a recreationalist,an employee,or a homemaker,each wants to be able to perform fundamental movements without limitations and pain.Assessments of function are designed to detect or assess abnormal movement patterns,limb asymmetries,pain,range of motion (ROM) limitations,proprioceptive deficits,strength,power,postural control,and core stabilization.Asymmetry is defined as side-to-side differences in strength,flexibility,mobility,and neural control; functional limitation is defined as a limitation in performance at the level of the whole person.2Asymmetries and functional limitations typically develop over time due to weak muscles,poor flexibility,injuries,development of movement compensations,vestibular or neurological disorders,aging,and poor posture.Asymmetries and functional limitations often result from injuries but also rise in number and severity with age.Although asymmetries and functional limitations may be expected following an injury,measureable asymmetries and functional limitations are also commonplace in healthy populations,3possibly due to hand dominance or as a result of the demands of physical work or training.In the aging population,functional limitations can lead to long-term dysfunction and disability.4In any age group—but particularly in an aging population—the results of screenings can be used to counsel participants about functional limitations and create individualized corrective exercise programs that reduce the risk of injury during work,recreation,and sports and decrease the likelihood of long-term dysfunction and disability.
The Functional Movement Screen (FMS™) has become increasingly popular for evaluation of functional movement patterns critical to normal function.The FMS™is a rapid,non-invasive,inexpensive,and easily administered tool5that assesses quality of fundamental whole-body movement patternsand identifies functional limitations and asymmetries.6The screen consists of seven different functional movement test items that assess trunk and core strength and stability,neuromuscular coordination,limb asymmetries during movement,postural control,proprioceptive deficits,and flexibility.5,7The quality of the movement in each of the seven screens is scored on a 0-3 scale based on specific objective criteria.A score of 3 is considered normal while a score of 2 or 1 represents levels of functional limitation.A score of 0 is given when there is pain during the movement.The scores from each of the seven test items are summed to generate a composite score (range 0-21).The scoring system is designed to capture major functional limitations and right-to-left asymmetries.Unlike other fitness assessments,the FMS™emphasizes the efficiency of movement patterns rather than the quantity of repetitions performed or the amount of weight lifted.5This approach is based,in part,on the assumption that identifiable deficits in movement patterns increase the susceptibility to injury.A review of the literature reveals that the majority of articles published about the FMSTMhave focused on the relationship between outcome on the FMSTMand athletic performance or injuries in collegiate and professional sports,6military training,8martial arts,9and firefighters.10Performance on the FMS™has been shown to effectively predict the likelihood of injury in athletes and firefighters.6,11FMSTMscores lower than 14 resulted in injury rates 11 times higher than scores over 15.11Having an asymmetry,regardless of the total FMSTMscore,doubled the risk of injury.5,6Work related injuries in firefighters were also found to decrease with increasing FMSTMscores,and to decrease with exercise programs based on FMSTMfindings.10
Marines with a 3-mile run time greater than 20.5 min had a 1.7 times greater risk of injury than Marines with a 3-mile run time less than 20.5 min.In addition,Marines who had a slow 3-mile run time and an FMSTMscore<14 were 4.2 times more likely to experience an injury.12Perry and Koehle13reported that the total FMSTMscore in adults between 21 and 82 years of age was significantly and positively correlated with physical activity (as measured by the Healthy Physical Activity Participation Questionnaire (HPAPQ)) after controlling for body mass index (BMI) and age.
The World Health Organization14and the Centers for Disease Control and Prevention15recommend using BMI (kg/m2) to categorize individuals as underweight (BMI<18.5),normal weight (BMI = 18.5-24.9),overweight (BMI = 25-29.9),or obese (BMI>30).The BMI is strongly associated with increased relative risk of cardiovascular disease and other pathologies.16A higher BMI was found to be more common among those with greater limitations in performing activities of daily living (ADL) and greater number of cardiovascular related disorders in those above the age 65.17Studies have reported a negative association between BMI and performance on the FMSTMin children18and adults.10Adults with a BMI>30 had a mean composite FMSTMscore that was 2 points less than adults with a BMI<30.10
Limited information is available about the efficacy of the FMSTMin an aging population.Perry and Koehle13reported total FMS™normative values in normal community dwelling adults (ages 21-82).Although they reported differences in total FMSTMscores between groups of subjects classified as either obese (BMI>30) or not obese (BMI<30),they did not report difference in the FMSTMscores in other BMI stratifications (i.e.,normal weight and overweight).Perry and Koehle13described the association between self-reported physical activity levels and performance on the FMSTM,but scores on individual test items were not reported and neither were left-to-right limb asymmetries on five of the seven FMSTMtest items.
This exploratory and descriptive study was undertaken to report total FMS™scores in older active adults,to provide preliminary normative reference values of each of the seven individual FMS™scores for both sexes,to report on asymmetries,and to evaluate the relationship between FMSTMscores,sex,age,BMI,and physical activity level.Inclusion criteria were: participants of the Senior Games and/or its associated Health Fair,subjects had to be able to stay for testing for about 30 min.The only exclusion criterion was inability to follow instructions in English.
2.Methods
2.1.Participants
Ninety-seven men (n = 53) and women (n = 44) between the ages of 52 and 83 years participated in this study (Table 1).Participants were recruited from attendees at a Health Fair held in conjunction with the 2012 annual World Senior Games.All participants reported in their pre-participation questionnaire that they followed their normal daily routine in regard to sleep,nutrition,and medication; we did not further control for these factors.This research project was approved by the Institutional Review Board for the use of Human Subjects in Research at Brigham Young University.Each participant provided written informed consent prior to participation in this study.
2.2.Data collection
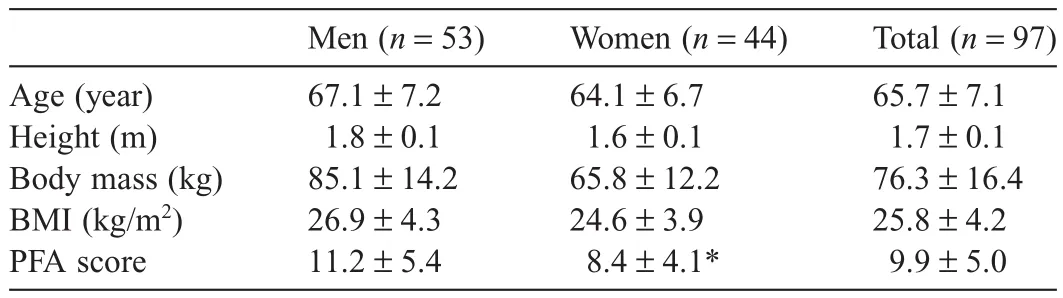
Table 1Participants’descriptive statistics (mean±SD).
Each participant’s height was measured to the nearest onequarter inch using a calibrated wall scale and body mass was measured to the nearest tenth of a pound using a digital scale (Healthometer Professional,Model 349KLX/320KL; Sunbeam Products,Inc.,Boca Raton,FL,USA).BMI was calculated from measures of height and body mass after being converted to cm and kg,respectively.Participants self-reported their age.To quantify activity level,all subjects completed the Perceived Functional Ability (PFA) Questionnaire.19It consists of twoquestions that are designed to quantify participants’perceived ability to walk,jog,or run 1- and 3-mile distances.The first PFA question asks,“Suppose you were going to exercise continuously on an indoor track for 1 mile.Which exercise pace is just right for you not too easy and not too hard?”The second PFA question asked,“How fast could you cover a distance of 3-mile and not become breathless or overly fatigued? Be realistic.”For each of the two questions,participants are to select one of 13 possible responses that best describe their current ability to walk,jog,or run 1 or 3 miles.For example,a 3 on the scale corresponds to“Walking at a medium pace (16 min per mile)”and a 9 corresponds to“Jogging at a medium pace (10 min per mile).”The participant’s PFA score is calculated as the sum of the responses to the two PFA questions.Thus,the range of possible PFA scores is 2-26.
Participants completed the FMS™with guidance from an investigator trained in using the FMSTM.The seven functional movements are: deep squat,hurdle step,inline lunge,shoulder mobility,active straight leg raise,trunk stability push-up,and rotary stability in quadruped position.20Further details about the FMS™,including pictures,can be found in the previous studies.5,7,21With the exception of the shoulder mobility exercise,each movement was performed three times.All exercises were video recorded to assure proper scoring at a later time.Two raters reviewed all videos and scored each of the FMS™exercises individually according to the scoring criteria.5
2.3.Scoring
The scores were compared between the two raters,and,in case of inconsistency,the video was reviewed until a consensus between the raters was reached.The FMS™has been studied extensively for inter- and intra-tester reliability.21-23A score of 3 was given when the exercise was performed completely,correctly,and without any visible compensation; a 2 was given when there was compensation,faulty form,or loss of alignment; a 1 was given when the movement was incomplete; and a 0 was given if the subject experienced pain during the movement.For calculating the total score the highest score of the three attempts was recorded for the deep squat and trunk stability.For those test items that included bilateral assessments (i.e.,hurdle step,inline lunge,shoulder mobility,rotary stability,and active straight leg raise) the lower of the two scores for the test item was used.However,in order to identify asymmetries,the scores for both sides were recorded and compared.
2.4.Statistical analysis
Basic descriptive statistics (means,standard deviations,and frequencies) are used to describe the functional movement scores for both sexes,for 5-year age groups,and for BMI groups.Three BMI groups were created using standard definitions: normal (<25),overweight (25-30),and obese (>30).14,15Two women had a BMI lower than 18.5 (17.2 and 17.9),which is considered“underweight”or“mild thinness”.We grouped them together with the“normal”group.Average differences by sex (independent variable) in functional movement scores (dependent variables) were compared using t tests and one-way ANOVA.Since the ANOVA main effect was significant a post hoc test with Bonferroni correction was performed.Correlations were estimated between the total functional movement score and age,BMI,and PFA.A multiple regression model was used to estimate the linear relationships between total FMSTMscore and age,BMI,and PFA.All interactions (three-way and two-way) between the explanatory variables were examined and none were significant; therefore,main effects are interpretable.
3.Results
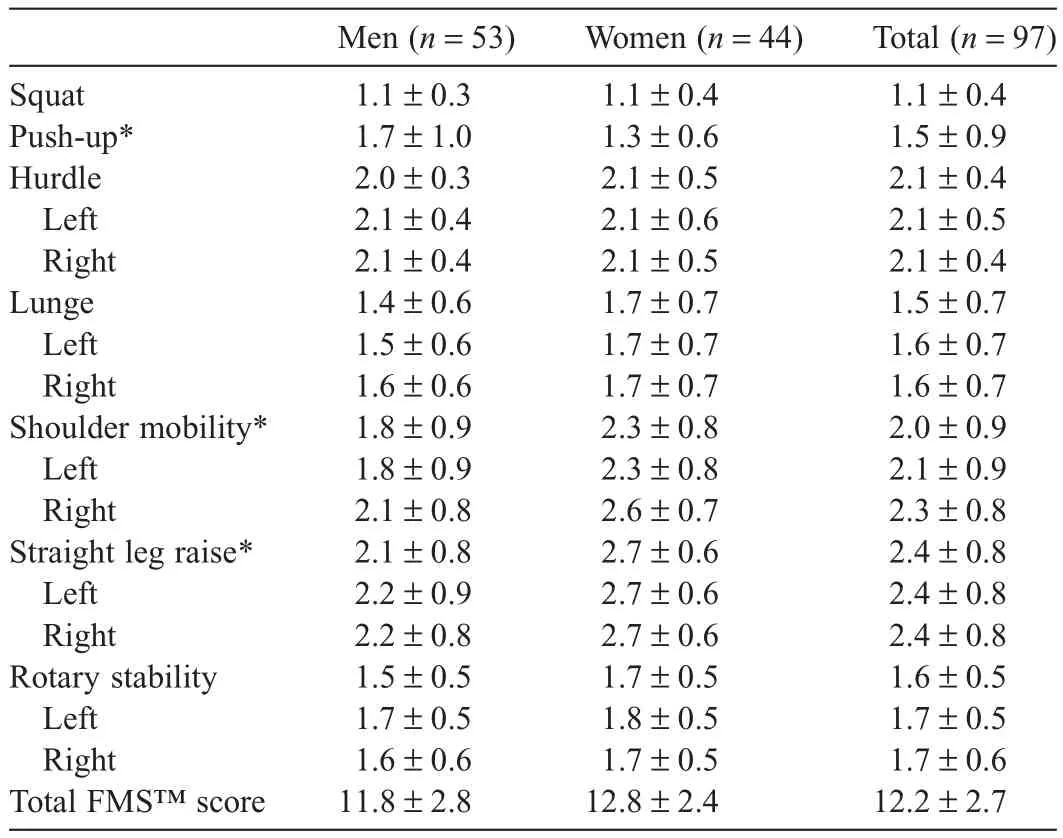
Table 2aIndividual and total scores on the FMS™stratified by sex (mean±SD).
Participant characteristics are shown in Table 1.The average age of the 97 participants was 65.7 years,with the men being slightly older than the women.The average BMI was 25.8,which classifies the participants as a whole as“overweight”; however,the women’s average BMI was below 25,classifying this group as“normal”.The PFA scores reported by men were significantly higher (p = 0.003) than the PFA scores reported by women.Scores on each of the seven FMS™test items and the total FMS™score,stratified by sex,are shown in Table 2a.The two tests assessing upper and lower extremity mobility show sex differences (women being more flexible) as does the push-up test,a screen for strength (men being stronger).The sex difference in the total FMS™score was not statistically significant.Total FMSTMscores stratified by age groups and BMI groups are shown in Tables 2b and 2c,respectively.The youngest age group (50-54 years) scored highest in all seven tests compared to all other age groups and the oldest age group (75+) scored lowest in most of the tests compared to all other groups.The subjects in the“normal weight”group performed no different than those who were in the“overweight”group; both groups performed better than the“obese”group.Nofurther statistical analyses were performed with the data shown in Tables 2b and 2c; they are meant for description only.
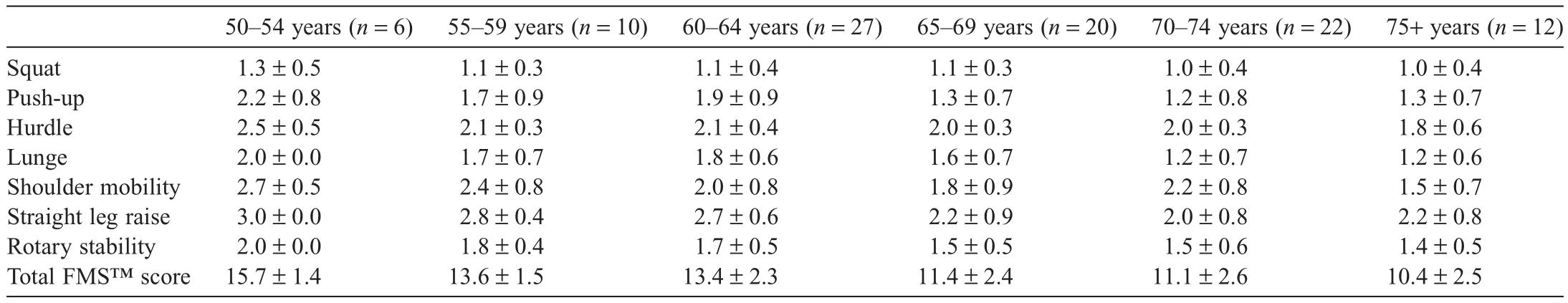
Table 2bTotal scores on the FMS™stratified by age groups (mean±SD).
Of the 97 participants in this study,55 (57%) had an asymmetry (strength or ROM) in at least one of the five FMSTMtest items that include bilateral assessments (Table 3).No further statistical analyses were performed with the data shown in Table 3; they are meant for description only.
The pairwise rank-based correlations between the total FMS™score and age (r =−0.531),BMI (r =−0.270),and the PFA score (r = 0.284) were significant (p<0.01).
Results from the multiple regression model with four predictors are found in Table 4.Age and BMI were significant predictors (p<0.01) of total FMSTMscores,but PFA and sex were not.Therefore,the significant bivariate relationship between total FMSTMscores and PFA disappears after adjusting for age and BMI.The regression model explained about 37% of the variability in total FMSTMscores.
4.Discussion
This study confirms the feasibility of performing the FMSTMin an active aging population when assessing functional limitations and asymmetries.This study also confirms the previously reported18significant negative correlation between performance on the FMSTMand age and BMI and a positive correlation to physical activity levels.To the best of our knowledge,this is the first study to report on the relationships between performance on the FMSTMand multiple BMI categories as well as the prevalence of asymmetries in older active people.
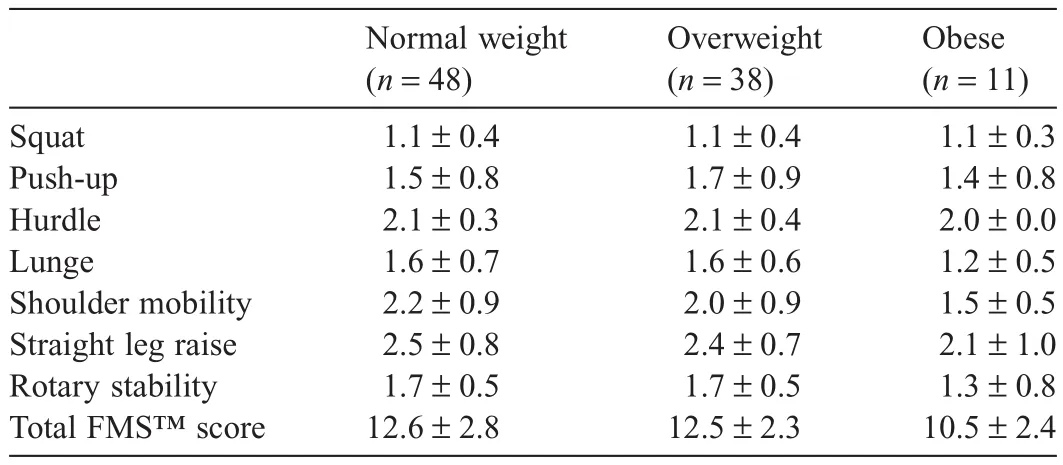
Table 2cTotal scores on the FMS™stratified by BMI groups (mean±SD).
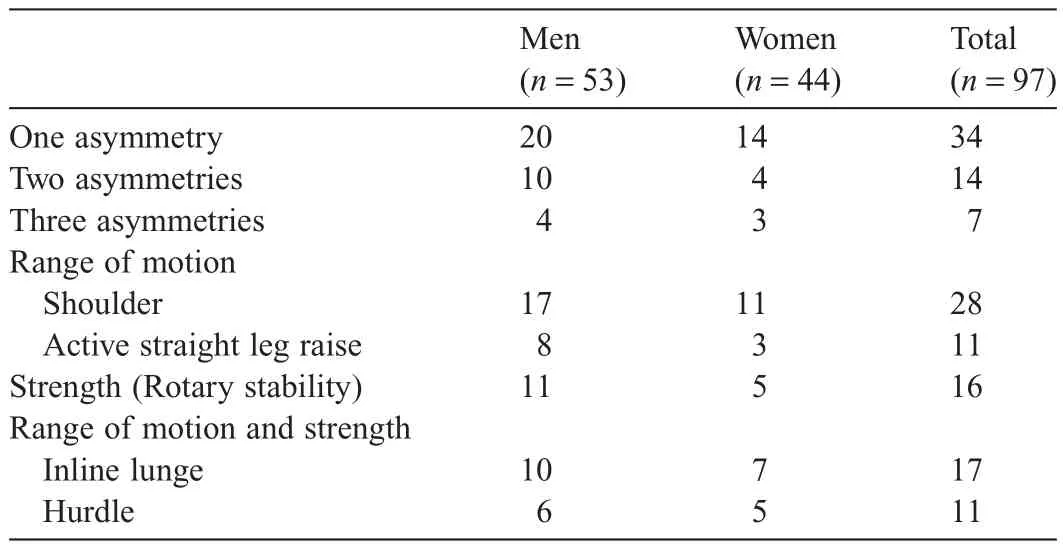
Table 3Asymmetry distribution.

Table 4Multiple regression results for total FMS™scores.
The total FMS™scores for the combined group of men and women ranged from 6 to 18 and the average score was 12.2 (of a possible21).The average total FMS™ score of the subjects in the present study (Table 2a) is lower than the average score (13.39) of the 357 subjects 50 years of age and older in the study conducted by Perry and Koehle.13One possible explanation of this discrepancy could be related to the methods of scoring participant’s performance on the FMSTM.In the present study,we videotaped all the test items for later evaluation by two trained investigators.This permitted the reviewers to scrutinizea test item if there were discrepancies between the two reviewers and reach a consensus in that score.Perry and Koehle13used an undisclosed number of certified physiologists to score the participants’performances on the FMSTM.Performance on the FMSTMwas scored by a single reviewer and reviewers didnot have the luxury of watching the test item on video to clarify any questions about the score.
Our study confirms the negative association between age and performance on the FMSTM.The subjects in our study who were in the age group of 75 years and older had the lowest FMSTMscores compared to the other age groups (Table 2b).This is not surprising as it is well established that most of the factors challenged by the FMS™,such as trunk and core strength,neuromuscular coordination,balance and flexibility,decline with age.24Strength is tested in five FMS™items: deep squat,hurdle step,inline lunge,trunk stability push up,and rotary stability.Muscle strength decreases with age at a rate of 1%-2% per year and muscle power even more so at a rate of 3.5% per year.25The decline in strength is more rapid than the simultaneous loss of muscle mass,hiding the weakening from visual inspection.Several FMS™test items challenge balance,such as the deep squat,hurdle step,inline lunge,and rotary stability tests.Coordination and balance deteriorate with age.26This decline can be caused by several factors,e.g.,somatosensory impairment,vestibular problems,and neuromuscular diseases,but it can also stem from muscle weakness.27Physiologically normal flexibility is required during the deep squat,shoulder mobility,and active straight leg raise exercises.It declines most drastically with age in knee flexion,followed by ankle dorsiflexion,and shoulder flexion in both sexes.28This directional range of motion changes coincides with the first two movements mentioned above tested during the FMS™.
The two age groups (55-59 and 60-64) had almost identical averages (and variability) for each of the test items.The averages of the total FMS™scores for the subsequent two age groups (65-69 and 70-74) were also very similar (Table 2b).This finding is consistent with the results of a very recent study24that found that elderly people in their 60s and 70s had similar functional characteristics in terms of physical performance,balance,mobility,and muscle strength.These characteristics decline in the elderly in their 80s with a concomitant increase in falls.24
The negative pairwise correlation between the total FMS™score and BMI indicates that functional movement patterns are adversely affected by excess body weight.Normal-weight participants (i.e.,BMI≤24.99) as well as overweight participants (i.e.,BMI 25.0-29.9) in this study had a total FMS™score that was two points greater than that of the obese participants (i.e.,BMI>30) (Table 2c).The findings of our study concur with the recent findings of Perry and Koehle13who also reported that subjects with a BMI<30 had a total FMS™score that was nearly two points higher than subjects with a BMI≥30.The adverse effects of a high BMIon FMSTMperformance may seem intuitive in that excess body mass could affect mobility,flexibility,stability,and balance.Limitations in these areas can lead to impairments and eventually to physical disability.The association between obesity and risk for physical disability has been previously reported.29,30In addition,high BMI values that are associated with physical inactivity may result in a poor performance on the FMSTMdue to the relative lack of physical activity that helps maintain or develop proprioception,neuromuscular control,balance,and stability.Of interest is also the fact that overweight participants demonstrated almost identical scores in each of the exercises when compared to the normal-weight participants.This could be a reflection of two factors:1)a higher BMI could be due to more and therefore heavier muscle tissue,skewing the true body composition (which is very likely in light of our athletic sample population),and 2) functionality might only be negatively affected once one enters the“obese”category.Regardless,the relationship between BMI and performance on the FMSTMreported in this study and that of Perry and Koehle13supports a growing need to emphasize the reduction of obesity in the aging population.Although the impact of excess body weight on health is well publicized,the results of this study confirm the impact of BMI on quality of life by adversely affecting the ability to perform fundamental movement patterns.
Multiple regression allowed us to explore the relationship between total FMS™score and the other variables simultaneously.Age and BMI were significantly associated with the FMSTMscore,accounting for about 37% of the variance in total FMS scores; sex and PFA (measuring physical activity) were not.In contrast,Perry and Koehle13reported that age,BMI,and physical activity levels were predictors in their model,but they accounted for only 24% of the variance in the total FMSTMscore.Our ability to explain more variability (37% vs.24%) with fewer variables (2 vs.3) compared to Perry and Koehle can likely be explained by our sample being more homogeneous in terms of physical activity,health status,and disease status compared to their sample,which was drawn from the general community.Also,while age and BMI would be related to physical activity in their data,age and BMI would not completely account for physical activity variability and its relationship to FMSTMscores,because differences in other factors,such as motivation,could also be related to physical activity.However,in this group of physically active older adults,whose motivation to be physically active is likely to be fairly similar,the variability in self-reported physical activity seems to be completely explained by age and BMI.Thus,in our results,PFA does not predict FMS scores after adjusting for age and BMI.In addition,we need to recognize that the PFA represents subjective information and does not actually measure cardiovascular capacity.It is possible that the subjects were not able to correctly predict their level of activity.Perry and Koehle13reported physical activity ratings of their subjects based on the HPAPQ.We were not able to obtain a copy of this particular questionnaire and were,therefore,not able to comment on it.Its questions might be more related to balance,coordination,postural control,flexibility,strength and power,rather than cardiovascular activity,and thus its outcome would have a greater relationship to the performance on the FMSTMthan our questionnaires.Another point to consider is the fact that the PFA was developed using college students aged 18-29.19Subjects of that (younger) age might have a different understanding of pace compared to subjects of older age.Both younger and older age groups,might have over- or underestimated their abilities due to being unfamiliar with aerobic exercise or other reasons.The fact that our subjects were athletes attending a health fair might diminish the latter concern.Either way,a possible decreased applicability of our findings to the general population has to be recognized.
Our data provide preliminary normative reference values for each of the seven individual FMS™exercises for both sexes of older active adults (Table 2a).While there was no overall sex difference in the total FMS™score,there were sex differences in some of the individual test items.Women scored higher than men on the tests that assessed flexibility or mobility.For example,only eight (18%) of the 44 women had a score of 1 on the shoulder mobility test,whereas 26 (49%) of the 53 men had a score of 1 on the shoulder mobility test.Likewise none of the women had a score of 0 and only three women had a score of 1 on the active straight leg raise test,whereas one man had a score of 0 and 15 men had a score of 1 on the active straight leg raise test.Men performed better on the push-up test,a measure of upper body strength and stability.Of the 53 men,15 (28%) scored a 3,whereas only three (7%) of the 44 women scored a 3 on the push-up test.Sex differences in strength and flexibility are well documented in the literature.28,31
The high prevalence (55 of 97 participants) of asymmetries in strength and flexibility (ROM) is alarming.Both have been linked to increased injury rates in younger athletes32,33and there is an association between leg strength asymmetry and falling in older subjects.3Because asymmetries can create functional limitations,they can lead to long-term dysfunction and disability,especially in the older population.4Over half of the participants in this study,more men than women,presented with an asymmetry in at least one of the five FMSTMtest items that include bilateral assessments,with the shoulder mobility test having the greatest number (n = 28).This is of interest because shoulder hypomobility as well as hypermobility can affect the entire kinematic chain,34lead to labral pathology and subacromial impingement35and ultimately possibly impact a person’s ability to participate in self-care and occupational activities.36The tests that had the next highest numbers in regard to asymmetries are the inline lunge and rotatory stability tests with 17 and 16 subjects,respectively.Both of these tests are quite complex,requiring core stability and available ROM in their respective joints.Core stability is the ability to stabilize the lumbar spine and pelvis area through muscle well-synchronized and strong co-contracting trunk muscles.37Asymmetrical core strength,which could be the result of any problem in the passive (spinal column),active (muscles),or neural components,38could put the stability of the spine at risk and thus jeopardize the proper execution of functional movement,decrease athletic performance,39and threaten postural control and balance.40Thus,early detection of asymmetries,for example by assessing performance on the FMS™,and consequent treatment can lead to decreased likelihood of injury,long-term dysfunction and disability.20
The scientific contribution of this study lies in its findings that the FMS™is feasible for elderly active adults.The screen was originally designed for younger athletes and we showed that the elderly active population is also able to perform the exercises associated with it.There are,however,some limitations to this study.This study was observational in nature,so we cannot establish a cause-and-effect relationship between the variables,but we can report significant correlations.The selfreported activity level was not confirmed by actual direct physiological measures and could,therefore,be skewed.However,self-reported physical activity measures“may provide a reasonable snapshot of population levels”.41Using a questionnaire seemed to be the only viable option for us considering the nature of the (Health Fair) event.
5.Conclusion
The total FMS™score decreases with increased BMI,increased age,and decreased activity level.The screen identifies range of motion- and strength-related asymmetries.While the American College of Sports Medicine identifies functional fitness training as an essential component of a well-rounded exercise program,it does not provide recommendations for assessing functional fitness as it does the other components of health-related physical fitness.42,43Based on our findings,we suggest using the FMS™as one of the tools in the assessment of functional fitness for the active elderly population.Future research should evaluate if a higher total FMS™score is related to fewer falls or injuries in the older population.
Authors’contributions
UHM participated in the design,data collection and writing of the manuscript.AWJ participated in the design,data collection and writing of the manuscript.PRV participated in the writing of the study.JBF participated in the data collection of the study.SCH performed the data analysis and helped in the writing of the manuscript.All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
None of the authors declare competing financial interests.
References
1.Bocalini DS,dos Santos L,Serra AJ.Physical exercise improves the functional capacity and quality of life in patients with heart failure.Clinics 2008;63:437-42.
2.Reiman MP,Manske RC.The assessment of function: how is it measured? A clinical perspective.J Man Manip Ther 2011;19:91-9.
3.Perry MC,Carville SF,Smith ICH,Rutherford OM,Newham DJ.Strength,power output and symmetry of leg muscles: effect of age and history of falling.Eur J Appl Physiol 2007;100:553-61.
4.Griffith L,Raina P,Wu HM,Zhu B,Stathokostas L.Population attributable risk for functional disability associated with chronic conditions in Canadian older adults.Age Ageing 2010;39:738-45.
5.Cook G,Burton L,Hoogenboom B.Pre-participation screening: the use of fundamental movements as an assessment of function—part 1.N Am J Sports Phys Ther 2006;1:62-72.
6.Kiesel K,Plisky PJ,Voight ML.Can serious injury in professional football be predicted by a preseason functional movement screen? N Am J Sports Phys Ther 2007;2:147-58.
7.Cook G,Burton L,Hoogenboom B.Pre-participation screening: the use of fundamental movements as an assessment of function—part 2.N Am J Sports Phys Ther 2006;1:132-9.
8.O’Connor FG,Deuster PA,Davis J,Pappas CG,Knapik JJ.Functional movement screening: predicting injuries in officer candidates.Med Sci Sports Exerc 2011;43:2224-30.
9.Bodden JG,Needham RA,Chockalingam N.The effect of an intervention program on functional movement screen test scores in mixed martial arts athletes.J Strength Cond Res 2015;29:219-25.
10.Peate WF,Bates G,Lunda K,Francis S,Bellamy K.Core strength: a new model for injury prediction and prevention.J Occup Med Toxicol 2007;2:3.
11.Kiesel K,Plisky P,Butler R.Functional movement test scores improve following a standardized off-season intervention program in professional football players.Scand J Med Sci Sports 2011;21:287-92.
12.Lisman P,O’Connor FG,Deuster PA,Knapik JJ.Functional movement screen and aerobic fitness predict injuries in military training.Med Sci Sports Exerc 2013;45:636-43.
13.Perry FT,Koehle MS.Normative data for the functional movement screen in middle-aged adults.J Strength Cond Res 2013;27:458-62.
14.World Health Organization.Global database on body mass index.Available at: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.[accessed 21.11.2013].
15.Centers for Disease Control and Prevention.How is BMI calculated? How is BMI interpreted for adults? Available at: http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html#Interpreted.[accessed 21.11.2013].
16.Canning KL,Brown RE,Jamnik VK,Kuk JL.Relationship between obesity and obesity-related morbidities weakens with aging.J Gerontol A Biol Sci Med Sci 2013;69:87-92.
17.Ahn S,Sharkey JR,Smith ML,Ory MG,Phillips CD.Variations in body mass index among olderAmericans: the roles of social and lifestyle factors.J Aging Health 2011;23:347-66.
18.Duncan MJ,Stanley M.Functional movement is negatively associated with weight status and positively associated with physical activity in British primary school children.J Obes 2012;2012:697563.doi:10.1155/2012/697563
19.George JD,Stone WJ,Burkett LN.Non-exercise VO2maxestimation for physically active college students.Med Sci Sports Exerc 1997;29:415-23.
20.Cook G,Burton L,Kiesel K,Rose G,Bryant M.Functional movement screen descriptions.Movement: functional movement systems: screening,assessment and corrective strategies.Santa Cruz,CA: On Target Publications; 2010.p.87-106.
21.Teyhen DS,Shaffer SW,Lorenson CL,Halfpap JP,Donofry DF,Walker MJ,et al.The functional movement screen: a reliability study.J Orthop Sports Phys Ther 2012;42:530-40.
22.Minick KI,Kiesel KB,Burton L,Taylor A,Plisky P,Butler RJ.Interrater reliability of the functional movement screen.J Strength Cond Res 2010;24:479-86.
23.Shultz R,Anderson SC,Matheson GO,Marcello B,Besier T.Test-retest and interrater reliability of the functional movement screen.J Athl Train 2013;48:331-6.
24.Nakano MM,Otonari TS,Takara KS,Carmo CM,Tanaka C.Physical performance,balance,mobility,and muscle strength decline at different rates in elderly people.J Phys Ther Sci 2014;26:583-6.
25.Skelton DA,Greig CA,Davies JM,Young A.Strength,power and related functional ability of healthy people aged 65-89 years.Age Ageing 1994;23:371-7.
26.Woollacott MH,Shumway-Cook A,Nashner LM.Aging and posture control: changes in sensory organization and muscular coordination.Int J Aging Hum Dev 1986;23:97-114.
27.Orr R.Contribution of muscle weakness to postural instability in the elderly.A systematic review.Eur J Phys Rehabil Med 2010;46:183-220.
28.Soucie JM,Wang C,Forsyth A,Funk S,Denny M,Roach KE,et al.Range of motion measurements: reference values and a database for comparison studies.Haemophilia 2011;17:500-7.
29.Rejeski WJ,Marsh AP,Chmelo E,Rejeski JJ.Obesity,intentional weight loss and physical disability in older adults.Obes Rev 2010;11: 671-85.
30.Gariepy G,Wang JL,Lesage A,Schmitz N.Obesity and the risk of disability in a 12-year cohort study: the role of psychological distress.Soc Psychiatry Psychiatr Epidemiol 2011;46:1173-9.
31.Epstein Y,Yanovich R,Moran DS,Heled Y.Physiological employment standards IV: integration of women in combat units physiological and medical considerations.Eur J Appl Physiol 2013;113:2673-90.
32.Nadler SF,Malanga GA,Feinberg JH,Prybicien M,Stitik TP,DePrince M.Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study.Am J Phys Med Rehabil 2001;80:572-7.
33.Fousekis K,Tsepis E,Poulmedis P,Athanasopoulos S,Vagenas G.Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: a prospective study of 100 professional players.Br J Sports Med 2011;45:709-14.
34.Manske R,Wilk KE,Davies G,Ellenbecker T,Reinold M.Glenohumeral motion deficits: friend or foe? Int J Sports Phys Ther 2013;8:537-53.
35.Cools AM,Johansson FR,Cagnie B,Cambier DC,Witvrouw EE.Stretching the posterior shoulder structures in subjects with internal rotation deficit: comparison of two stretching techniques.J Shoulder Elbow 2012;4:56-63.
36.Johnson AJ,Godges JJ,Zimmerman GJ,Ounanian LL.The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis.J Orthop Sports Phys Ther 2007;37:414-5.
37.Kong Y,Cho Y,Park W.Changes in the activities of the trunk muscles in different kinds of bridging exercises.J Phys Ther Sci 2013;25: 1609-12.
38.Panjabi MM.The Stabilizing System of the Spine.Part I.Function,dysfunction,adaptation,and enhancement.J Spinal Disord 1992;5: 383-9.
39.Leetun DT,Ireland ML,Willson JD,Ballantyne BT,Davis IM.Core stability measures as risk factors for lower extremity injury in athletes.Med Sci Sports Exerc 2004;36:926-34.
40.Oliver GD,Adams-Blair HR.Improving core strength to prevent injury.J Phys Educ Recreat Dance 2010;81:15-9.
41.Bauman A,Phongsavan P,Schoeppe S,Owen N.Physical activity measurement—a primer for health promotion.Promot Educ 2006;13:92-103.
42.American College of Sports Medicine.ACSM’s guidelines for exercise testing and prescription.9th ed.Baltimore,MD: Wolters Kluwer/Lippincott Williams & Wilkins; 2014.p.162-93.
43.Garber CE,Blissmer B,Deschenes MR,Franklin BA,Lamonte MJ,Lee IM,et al.American College of Sports Medicine position stand.Quantity and quality of exercise for developing and maintaining cardiorespiratory,musculoskeletal,and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise.Med Sci Sports Exerc 2011;43:1334-59.
杂志排行
Journal of Sport and Health Science的其它文章
- Non-linearity in the dynamic world of human movement
- Comparing dynamical systems concepts and techniques for biomechanical analysis
- Multi-scale interactions in interpersonal coordination
- Can coordination variability identify performance factors and skill level in competitive sport? The case of race walking
- Multiscale entropy: A tool for understanding the complexity of postural control
- A history of low back pain affects pelvis and trunk coordination during a sustained manual materials handling task
