Retinal asymmetry in Chinese adults measured by cirrus high definition optical coherence tomography
2016-02-27SyedNasirAliShahLinZhangXiaoJuanFanJinDengFaisalShahbazUmerFarooq
Syed Nasir Ali Shah, Lin Zhang, Xiao-Juan Fan, Jin Deng, Faisal Shahbaz, Umer Farooq
1Department of Ophthalmology, First Affiliated Hospital of Xi’an Jiaotong University, School of Medicine, 277 Yanta West Road, Xi’an 710061, Shaanxi Province, China
2Cumberland Infirmary Hospital, Newtown Road, Carlisle, Cumbria CA2 7HY, England, the U.K.
3Department of Community Medicine, Ayub Medical College, Abbotabad 22010, Khyber Pakhtunkhwa, Pakistan
Correspondence to:Lin Zhang. Department of Ophthalmology, First Affiliated Hospital of Xi’an Jiaotong University, School of Medicine, 277 Yanta West Road, Xi’an 710061, Shaanxi Province, China. 1711056348@qq.com
Received: 2015-02-28 Accepted: 2015-08-20
Retinal asymmetry in Chinese adults measured by cirrus high definition optical coherence tomography
Syed Nasir Ali Shah1, Lin Zhang1, Xiao-Juan Fan1, Jin Deng1, Faisal Shahbaz2, Umer Farooq3

1Department of Ophthalmology, First Affiliated Hospital of Xi’an Jiaotong University, School of Medicine, 277 Yanta West Road, Xi’an 710061, Shaanxi Province, China
2Cumberland Infirmary Hospital, Newtown Road, Carlisle, Cumbria CA2 7HY, England, the U.K.
3Department of Community Medicine, Ayub Medical College, Abbotabad 22010, Khyber Pakhtunkhwa, Pakistan
Correspondence to:Lin Zhang. Department of Ophthalmology, First Affiliated Hospital of Xi’an Jiaotong University, School of Medicine, 277 Yanta West Road, Xi’an 710061, Shaanxi Province, China. 1711056348@qq.com
Received: 2015-02-28Accepted: 2015-08-20
引用:Shah SNA, Zhang L, Fan XJ, Deng J, Faisal S, Umer F. 新型频域相关断层扫描对健康年轻人视网膜各参数的测量分析.国际眼科杂志2016;16(2):207-212
Abstract
•AIM: To investigate the physiological asymmetry of retinal parameters with cirrus high-definition optical coherence tomography (Cirrus HD-OCT) in healthy young adults.
•METHODS: In this cross-sectional observational study we included 146 normal young adults. Bilateral eyes retinal parameters such as retinal nerve fiber layer thickness, optic nerve head and macula were assessed with OCT and mean differences for all parameters were established by subtracting the values of left eye from the right eye parameters and evaluated by paired samplet-test. Interocular differences were evaluated and cut off points at 2.5thand 97.5thpercentiles were produced. Retinal parameters were correlated. Effects of gender and blood pressure on retinal parameters were evaluated by regression analysis.
•RESULTS:Average retinal nerve fiber layer (RNFL) thickness was not statistically significant (+0.7 μm,P=0.09). Significant thickness was present in temporal quadrant (+2.51 μm, P=0.02), nasal quadrant (+2.50 μm,P=0.04), clock hours 2/10 (+5.85 μm,P=0.002), 3/9 (+3.20 μm,P=0.005), 11/1 (+3.80 μm,P=0.024), average (-0.034 μm,P=0.013) and vertical cup-to-disc ratio (-0.028 μm,P=0.008), macular inner nasal quadrant (+7.76 μm,P=0.003) in right eyes. Superior quadrant was significantly thicker in left eyes (-2.40 μm,P=0.03). Cut-off values for average RNFL and macular thicknesses were 11.00 μm and 18.00 μm, respectively. Bilateral eyes have moderate interocular correlation (0.41-0.6) for retinal parameters and not correlated with gender and blood pressure (P<0.05 regression). The interocular differences in average RNFL and macular thickness of normal adults should not exceed 11 μm and 18 μm, respectively, if measured with Cirrus HD-OCT.
•CONCLUSION: Asymmetry in retinal parameters exists in healthy eyes and provides valuable assessments in diagnosing retinopathies at early stage.
KEYWORDS:•cirrus high-definition optical coherence tomography; asymmetry; retinal parameters
Citation:Shah SNA, Zhang L, Fan XJ, Deng J, Faisal S, Umer F. Retinal asymmetry in Chinese adults measured by cirrus high definition optical coherence tomography.GuojiYankeZazhi(IntEyeSci) 2016;16(2):207-212
INTRODUCTION
Paired organs in human body are symmetric up to certain degree. This fact of anatomical symmetry has become an investigative tool in diagnosis when they become asymmetric. Retinal parameters asymmetry has become an important sign for clinical diagnosis in glaucomatous optic neuropathy and maculopathies[1-2]. Although they have bilateral eye effects, yet asymmetry is evident. In addition, some disease entities preferentially affect one eye; for example Duane syndrome is more common in female patients (60%) and more commonly affects the left eye (59%) with no clear explanation for this preponderance[3].
In clinical practice, traditionally fundoscopy and retinography have been remained very important for evaluating disease progression. In the past two decades, revolutions in investigative techniques have paved a path for quantitative and qualitative analysis. Optical coherence tomography (OCT) a non invasive modality is the state-of-the art technique which has gain popularity in clinical practice with high resolution, cross-sectional information and investigating various ocular pathological changes in anterior and posterior segment[4]. Cirrus high-definition optical coherence tomography (Cirrus HD-OCT), prototype of spectral domain (SD) OCT offers high resolution (5-7 μm) allowing precise evaluation of retinal parameters and gaining importance in clinical practice[5]. Normative database have been published by manufacturer for retinal parameters in various age groups in different ethnicity[6,9]. It is important to determine which values of asymmetry should be considered as symptoms of pathology.
In the present study we examined physiological asymmetry in retinal parameters with Cirrus HD-OCT (Carl Zeiss Meditec, Dublin, California, USA) and correlate them with gender and blood pressure in healthy young subjects (18-28y). We also establish the limits beyond which the clinician may suspect the presence of pathology.
SUBJECTS AND METHODS
This was a cross-sectional observation study undertaken in Xi’an Jiaotong Medical University Hospital, China from Oct. 2010 till Mar. 2011. The study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board. Out of 170 university students, 146 (86%) participated in the study and were included as the subjects. Students were informed the nature of the study and signed a consent with questionnaire providing information about their health status and family history. Included in the study were subjects with no ocular abnormality except refractive error less than ±6.00 diopters and normal fundoscopy. Subjects were excluded if they had a history of intraocular surgery, retinal pathology or family history of retinopathies, optic nerve cup to disc ratio >0.5 or asymmetry of >0.2 between fellow eyes. All subjects underwent comprehensive physical and ophthalmic examination.
Visual acuity was recorded using Snellen acuity chart and subject’s own prescription correction. Objective refraction was measured with autorefractometer (RK-F1 autorefractor; Canon, Tokyo, Japan). Axial length was measured using an optical biometer (IOL Master; Zeiss Meditec, Jena, Germany) and calculated as the average of at least three scans. Arterial blood pressure was measured in sitting position after at least 5min of rest.
Evaluation of retinal nerve fiber layer (RNFL), optic nerve head (ONH) and macular parameters were evaluated by Cirrus HD-OCT. The examination was performed without pupil dilatation[10]. Signal strength of six or greater was considered for evaluation[11]. Right eye was scanned first and followed by left eye in all the participants by same operator. Internal fixation was used to prevent ocular movements and to ensure alignment of the eye to prevent the highest reproducibility[12]. The 200×200 Optic disc cube protocol was utilized to assess peripapillary RNFL thickness (average, all four quadrants and clock hours) symmetry , rim area, disc area, average C/D ratio, vertical C/D ratio and cup volume were recorded. For clock hours RNFL thicknesses were defined for right and left eye as; clock hour 1 in right correspond to clock hour 11 in left eye, clock hour 2 in right eye correspond to clock hour 10 in the left eye and so on. By 512×128 macular cube protocol we evaluated macular parameters through Early Treatment Diabetic Retinopathy Study (EDTRS) grid. The grid divided macula into 9 regions with 3 concentric rings centered on the fovea. Innermost ring has 1 mm, inner has 3 mm and outer has 6 mm diameter. The innermost ring measures fovea and outer two rings divided into four equal quadrants, measuring the distance between inner limiting membrane (ILM) and inner boundary of retinal pigment epithelium (RPE). The correlations between right and left eyes were assessed by the intraclass correlation coefficients (ICC). Correlation was considered slight if values were 0-0.2, fair if 0.21-0.4, moderate if 0.41-0.6, substantial if 0.61-0.8, and almost perfect if greater than 0.81[13].
Statistical analysis was carried out with SPSS(version 20.0,USA). Data normality was assessed with Shapiro-Wilk test. Descriptive statistics were reported as means and SDs. Categorical variables were presented as number and percentages. Mean differences for all parameters were established by subtracting the values of left eye from the right eye parameters and their respective significant values by paired samplet-test. Normal ranges of interocular differences
Table 1Baseline characteristics of study population
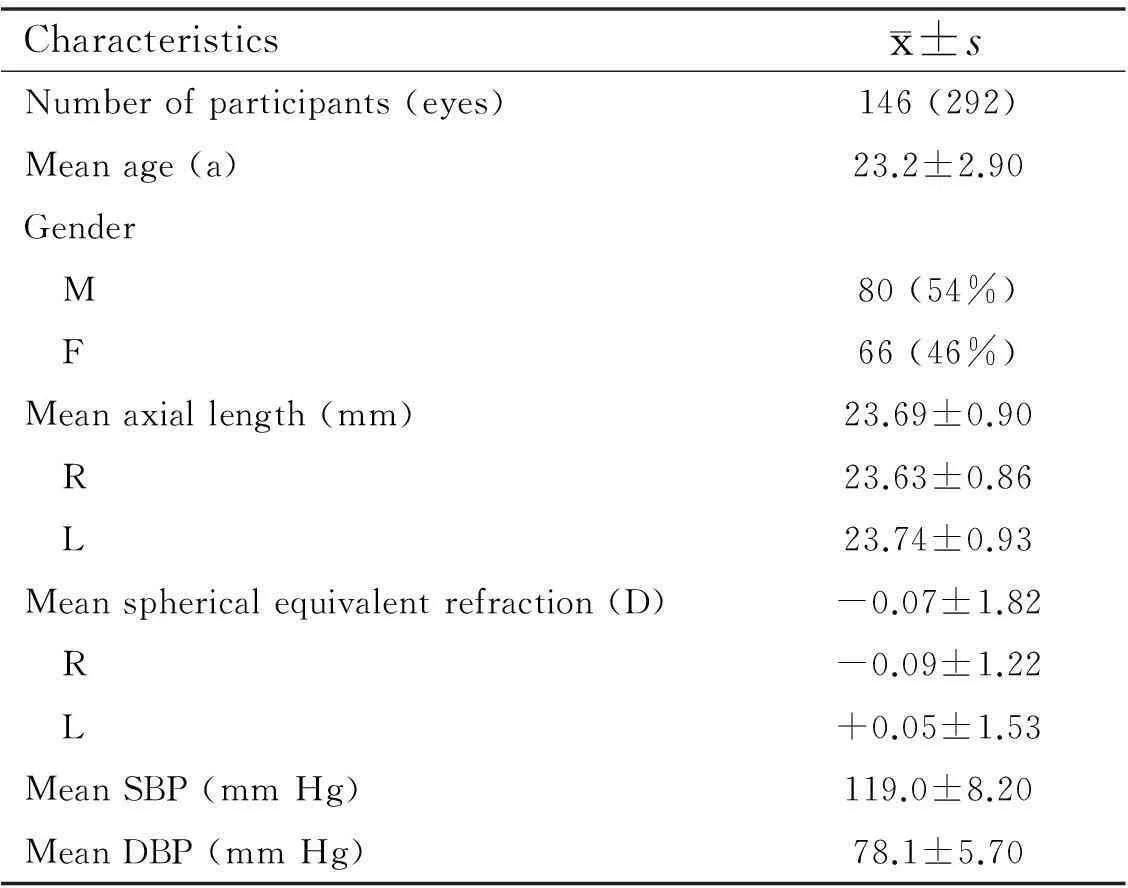
Characteristicsx±sNumberofparticipants(eyes)146(292)Meanage(a)23.2±2.90Gender M80(54%) F66(46%)Meanaxiallength(mm)23.69±0.90 R23.63±0.86 L23.74±0.93Meansphericalequivalentrefraction(D)-0.07±1.82 R-0.09±1.22 L+0.05±1.53MeanSBP(mmHg)119.0±8.20MeanDBP(mmHg)78.1±5.70
SBP: Systolic blood pressure; DBP: Diastolic blood pressure.
were established as 2.5thand 97.5thpercentiles for continuous variables. Mean differences for all parameters were calculated by subtracting left eye parameters and considered positive when right eyes had higher values and negative when left eyes had greater measurements. The correlation/ (intraocular agreement) between right and left eye were computed by ICC. Influence of sex and blood pressure monometry on interocular asymmetry was analyzed by regression model and reported along with thePvalues.Pvalues less than 0.05 were considered as statistically significant.
RESULTS
A total of 150 subjects were enrolled for this study.Four subjects were excluded because of signal strength below 6. The mean age was 23.2±2.90 (range 18 to 28) y with 54% male. No statistically significant differences were noted in baseline characteristics of and mentioned in Table 1.
Table 2 presents the OCT parameters including RNFL, optic nerve head and macular differences between right and left eyes. Interocular differences were concluded by right eye minus left eye. Average RNFL was thicker on right eye but was not statistically significant. RNFL was thicker in temporal and nasal quadrant on right eye and thicker in superior quadrant on left eye and their differences were statistically significant. For clock hours 1/11, 5/7 and 6/6 were thicker on left eye and significant difference was present at 2/10, 3/9 and 11/1. Optic nerve head parameters demonstrated significant difference in average and vertical cup/disc ratio. In macular parameters left eye showed high parameters and significant difference was demonstrated at inner nasal quadrant.
Table 3 reports percentile distribution of interocular asymmetry in peripapillary RNFL thickness, optic nerve head and macular parameters. For average RNFL thickness 2.5thand 97.5thpercentiles were -7.38 μm and 11.00 μm respectively depending of which eye has thicker average RNFL. Cut off points for quadrant RNFL thickness has higher values than
Table 2Mean interocular difference in retinal parameters (OD-OS)

VariablesODOSDifferencePRNFLT(μm) Average98.6597.920.7±2.20.09 Superior120.33122.75-2.4±3.20.03 Inferior124.42123.361.06±4.60.28 Nasal70.7268.222.50±2.10.04 Temporal69.4566.942.51±4.90.02Clockhour(μm) C12/12140.32140.47-0.42±5.50.873 C1/11122.12124.55-2.42±7.50.350 C2/1093.5787.725.85±2.60.002 C3/957.8254.633.20±9.80.005 C4/866.8964.872.01±9.10.181 C5/799.80103.50-3.70±9.70.222 C6/6137.37138.66-1.2±6.80.647 C7/5133.68133.560.12±4.70.961C8/470.7368.482.25±1.20.201 C9/357.2557.95-0.70±3.50.625 C10/279.2779.50-0.23±2.60.845 C11/1131.44127.683.80±5.00.024Opticnerve Rimarea(mm2)1.3821.3800.002±4.20.927 Discarea(mm2)2.472.51-0.041±1.20.319 AverageC/Dratio0.440.47-0.034±6.20.013 VerticalC/Dratio0.430.48-0.028±4.90.008 Cupvolume(mm3)0.0290.0260.003±2.50.243Macularthickness(μm) MacularThickness262.673262.5640.108±5.60.590 Innertemporal291.650292.240-0.594±3.20.647 Innersuperior291.073288.0872.987±2.40.278 Innerinferior292.513293.19-0.6800±4.20.746 Innernasal302.15294.397.7647±4.30.003 Outertemporal254.560254.90-0.3400±2.80.785 Outersuperior279.640279.280.3600±7.80.541 Outerinferior254.56254.90-0.2800±2.10.758 Outernasal292.25292.68-0.427±2.30.642Macularvolume(mm3)9.6269.665-0.039±2.80.539
OD: Right eye; OS: Left eye; RNFLT: Retinal nerve fiber layer thickness; C: Clock hour, 1/11 nominator represents right eye and denominator represents left eye; C/D: Cup to disc ratio.P<0.05.
average RNFL thickness values and have greater limit difference (e.g. superior quadrant -29.10 μm to 24.40 μm). Cut off points for macular thickness in 2.5thand 97.5thpercentiles were -15.30 μm to 18.00 μm, whereas the inner inferior quadrant has -15.00 μm to 16.00 μm, presenting small variation in average and quadrant analysis at EDTRS ring. We have computed ICC between right and left eye for retinal parameters. ICC was in the range of moderate (0.41-0.6) for all the measurements. Gender and blood pressure difference showed no influence on interocular asymmetry in retinal parameters (P>0.05, regression analysis).
DISCUSSION
Many diseases present unilateral or asymmetric patho-physiology in adults, including optic neuropathies[11]and maculopathies[17,19]. Changes in OCT measurements compared with other ancillary tests should be considered warning signs
Table 3Percentile distribution of interocular differences
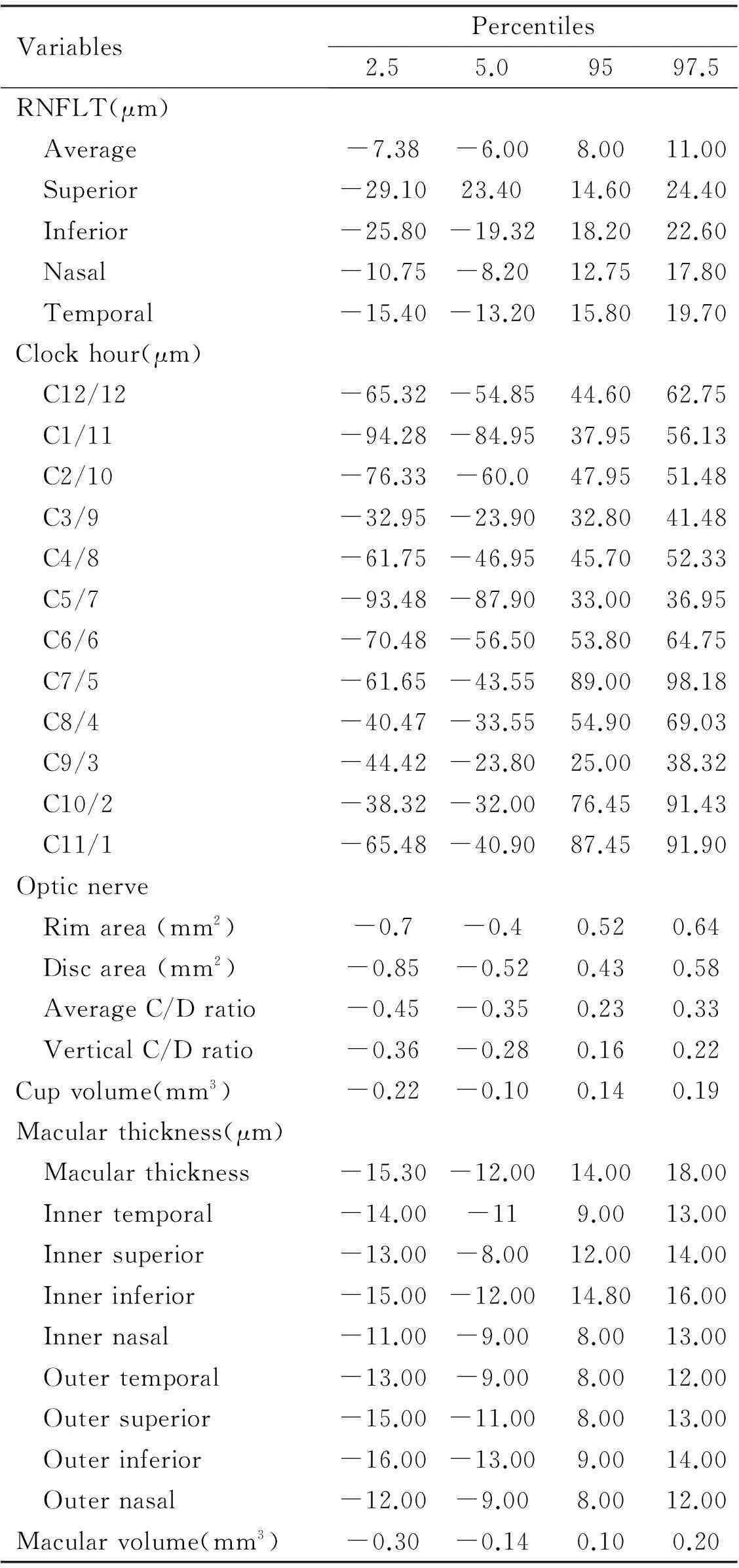
VariablesPercentiles2.55.09597.5RNFLT(μm) Average-7.38-6.008.0011.00 Superior-29.1023.4014.6024.40 Inferior-25.80-19.3218.2022.60 Nasal-10.75-8.2012.7517.80 Temporal-15.40-13.2015.8019.70Clockhour(μm) C12/12-65.32-54.8544.6062.75 C1/11-94.28-84.9537.9556.13 C2/10-76.33-60.047.9551.48 C3/9-32.95-23.9032.8041.48 C4/8-61.75-46.9545.7052.33 C5/7-93.48-87.9033.0036.95 C6/6-70.48-56.5053.8064.75 C7/5-61.65-43.5589.0098.18 C8/4-40.47-33.5554.9069.03 C9/3-44.42-23.8025.0038.32 C10/2-38.32-32.0076.4591.43 C11/1-65.48-40.9087.4591.90Opticnerve Rimarea(mm2)-0.7-0.40.520.64 Discarea(mm2)-0.85-0.520.430.58 AverageC/Dratio-0.45-0.350.230.33 VerticalC/Dratio-0.36-0.280.160.22Cupvolume(mm3)-0.22-0.100.140.19Macularthickness(μm) Macularthickness-15.30-12.0014.0018.00 Innertemporal-14.00-119.0013.00 Innersuperior-13.00-8.0012.0014.00 Innerinferior-15.00-12.0014.8016.00 Innernasal-11.00-9.008.0013.00 Outertemporal-13.00-9.008.0012.00 Outersuperior-15.00-11.008.0013.00 Outerinferior-16.00-13.009.0014.00 Outernasal-12.00-9.008.0012.00Macularvolume(mm3)-0.30-0.140.100.20
RNFLT: Retinal nerve fiber layer thickness; C: Clock hour, 1/11 nominator represents right eye and denominator represents left eye; C/D: Cup to disc.
and indication for further examinations[13]. Previous studies report that OCT measurements of the macula, RNFL, and optic nerve are reliable and highly reproducible in adults[14]. Compared with other imaging techniques, HD-OCT has been proven to provide higher resolution and more detail led images, which should result in more precise quantitative analysis of the retinal structures[2,6,13,15]. To determine the physiological ranges of interocular asymmetry in retinal structures, it is essential to detect abnormal values. Our study is the first to assess the physiological asymmetry in the RNFL, ONH, and macular measurements with HD-OCT in a community sampling of young adults.
In our study interocular correlations of the retinal measurements were moderate (0.41-0.6) for most parameters. We did not find statistically significant differences in average RNFL thicknesses between both eyes. However, interocular differences between right and left eyes were statistically significant for nasal, temporal, average and vertical C/D ratio and inferior nasal circle with the right eyes showing thicker RNFL than the left eyes. Several studies have assessed the asymmetry of RNFL thickness by OCT. Studies performed with previous versions of OCT showed similar results[6,8].
According to previous literature, only few studies have documented presence of interocular asymmetry in young adults. Budenzetal[6]used Stratus OCT and reported significant interocular difference in RNFL thickness but not significant impact in macular parameters. They conducted their study with TD-OCT with less resolution than Cirrus SD-OCT. In three previous studies, Cirrus SD-OCT was applied to measure interocular difference in adults. Mwanzaetal[9]use evaluated only RNFL symmetry in a population aged 18-84y with a mean age of 46.13±16.87y. Hwangetal[15]evaluated only RNFL symmetry using Cirrus HD-OCT and found interocular significant difference in a population of 36.4±19.8y (range: 5 to 80y) old adults. Our finding of thicker RNFL at nasal and temporal quadrant in right eyes is in consistence with their findings. We similarly observed consistent results with Mwanzaetal[9]in 2/10, 3/9 and 11/1 clock hour difference between right and left eye. Jeeetal[16]studied RNFL symmetry similar to our study in a population of young adults 19-28 year old adults. Our finding of thicker average RNFL at right eye is in consistence with their finding.
In Table 4 previous work on interocular differences by age and OCT device is documented. Thicker nasal and temporal RNFL quadrant in right eyes is common finding among all studies. In our study we have reported significant difference (R>L) in average and vertical C/D ratio which is not with consistence with any mentioned study in the table. Macular parameters been studied by only few investigators. Our Inner nasal circle (R>L) is in consistence with Dalglieshetal[2].
In our study we evaluate cut-off limit values at 2.5thand 97.5thfor retinal perimeters. Values crossing these limits can be considered for further investigation. In previous literature, OCT measurement is higher for quadrants than for the average interocular differences. Our study is also in agreement with previous studies and we have tolerance limits range from 17.80-24.40 μm. Our results have consistency with previous study by Budenzetal[6]11.7 μm, Mwanzaetal[9]8.8 μm and range of 16-17 μm reported by Sydney Childhood Eye Study[8]. Tolerance limits for optic nerve parameters include rim area, disc area, cup-to-disc area, vertical cup-to-disc area and cup volume were 0.64 μm, 0.58 μm, 0.33 μm, 0.22 μm, 0.19 μm respectively. We have found the least difference between right and left eyes in parameters related to optic disc with 0.002 μm, 0.04 μm, 0.034 μm, 0.028 μm and 0.003 μm3for rim area, disc area, average cup-to-disc ratio, vertical cup to disc ratio and cup volume respectively. Interocular differences at macula were 18.0 μm and 0.20 μm3for macular thickness and volume respectively.
Table 4Previous results of interocular differences and cut off point
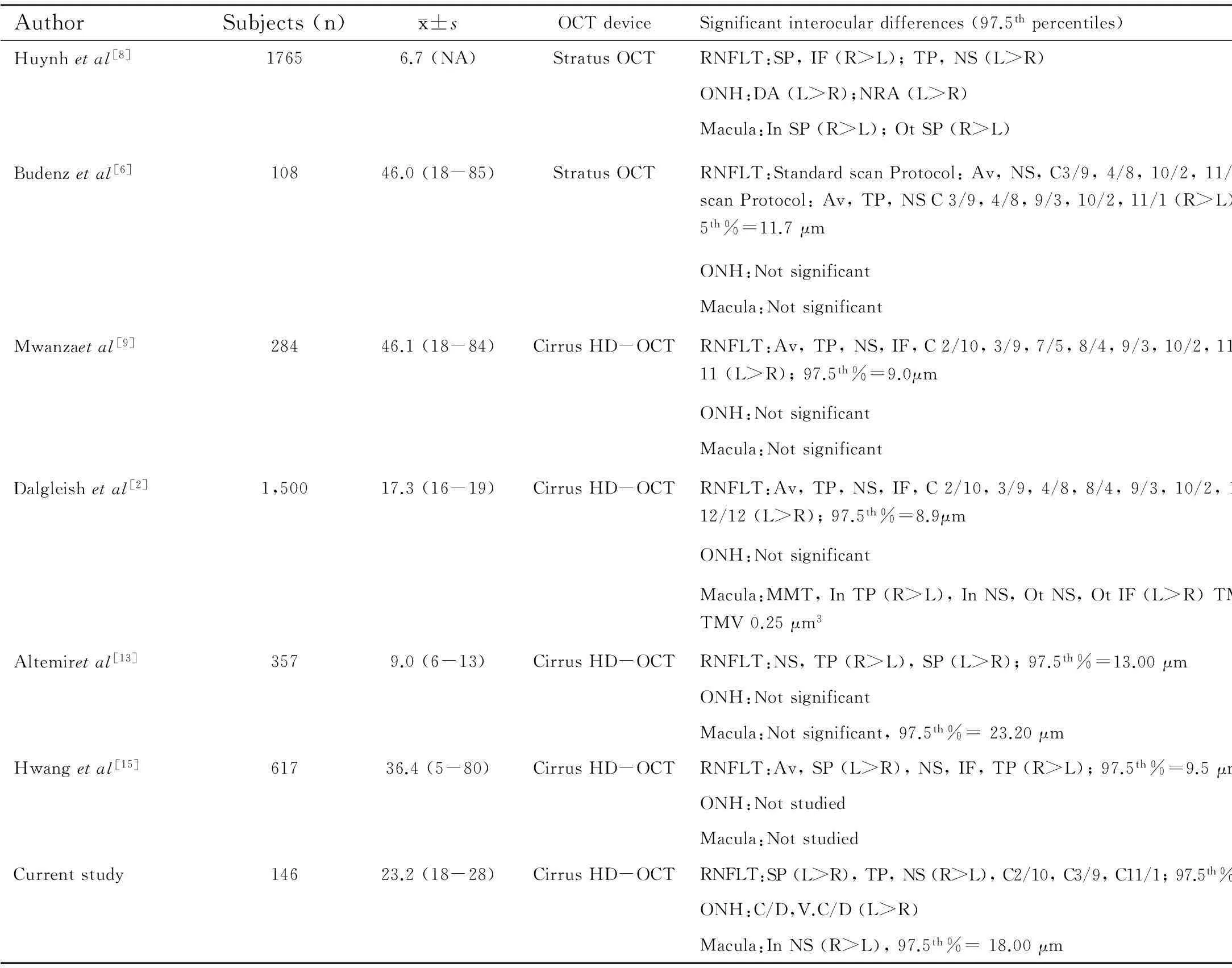
AuthorSubjects(n)x±sOCTdeviceSignificantinteroculardifferences(97.5thpercentiles)Huynhetal[8]17656.7(NA)StratusOCTRNFLT:SP,IF(R>L);TP,NS(L>R)ONH:DA(L>R);NRA(L>R)Macula:InSP(R>L);OtSP(R>L)Budenzetal[6]10846.0(18-85)StratusOCTRNFLT:StandardscanProtocol:Av,NS,C3/9,4/8,10/2,11/1(R>L)C1/11(L>R);FastscanProtocol:Av,TP,NSC3/9,4/8,9/3,10/2,11/1(R>L)SP,C1/11,12/12(L>R);97.5th%=11.7μmONH:NotsignificantMacula:NotsignificantMwanzaetal[9]28446.1(18-84)CirrusHD-OCTRNFLT:Av,TP,NS,IF,C2/10,3/9,7/5,8/4,9/3,10/2,11/1(R>L),SPC12/12,5/7,1/11(L>R);97.5th%=9.0μmONH:NotsignificantMacula:NotsignificantDalgleishetal[2]1,50017.3(16-19)CirrusHD-OCTRNFLT:Av,TP,NS,IF,C2/10,3/9,4/8,8/4,9/3,10/2,11/1(R>L);SP,C1/11,7/5,12/12(L>R);97.5th%=8.9μmONH:NotsignificantMacula:MMT,InTP(R>L),InNS,OtNS,OtIF(L>R)TMV(L>R);97.5th%=10.0μm,TMV0.25μm3Altemiretal[13]3579.0(6-13)CirrusHD-OCTRNFLT:NS,TP(R>L),SP(L>R);97.5th%=13.00μmONH:NotsignificantMacula:Notsignificant,97.5th%=23.20μmHwangetal[15]61736.4(5-80)CirrusHD-OCTRNFLT:Av,SP(L>R),NS,IF,TP(R>L);97.5th%=9.5μmONH:NotstudiedMacula:NotstudiedCurrentstudy14623.2(18-28)CirrusHD-OCTRNFLT:SP(L>R),TP,NS(R>L),C2/10,C3/9,C11/1;97.5th%=11.00μmONH:C/D,V.C/D(L>R)Macula:InNS(R>L),97.5th%=18.00μm
P<0.05; Av: Average; RNFLT: Retinal Nerve Fiber Layer Thickness; ONH: Optic Nerve Head; SP: Superior; IF: Inferior; NS: Nasal; TP: Temporal; L: Left; R: Right; DA: Disc area; NRA: Neuroretinal rim area; MMT: Mean Macular Thickness; In: Inner; Ot: Outer; TMV: Total Macular Volume; CDR: Cup-to-disc ratio; C: Clock hour; C/D: Cup/Disc; V: Vertical.
In this study we have moderate interocular correlation for macular and optic disc parameters in young adults. Physiological symmetry between cups of the optic nerve head has been reported and differences of greater than 0.2 occurring in only 1%-6% of the normal population[17]. Huynh and associates[8]examined interocular differences in macular thickness and optic disc parameters in young children. They found that the interocular correlation was moderate for central macular thickness, with interocular differences of up to 31 μm. In our study conducted in young adults we found that central macular thickness was symmetric parameter of macula. This finding has potential for clinical application while diagnosing maculopathies in young adults such as idiopathic choroidal neovascularization[18-19]and central serous chorioretinopathy[20]. Therefore CMT asymmetry greater than 18 μm between both eyes can be considered for further investigation.
The strength of current study sample we involved young healthy adults with no confounding factors of ocular and systemic illness. All subjects have undergone comprehensive ophthalmic examination as inclusion protocol. We reduce selection bias by examining young university students as a community sampling of young adults which reduce selection bias.
Limitations of our study should be addressed. We have relatively small number of East Asian subjects from 18-28y of age and we included only subjects with less than ±6 diopters, hence our conclusion may not be applicable to subjects with higher refractive errors and other races[21-22]. Another limitation that we did not apply enhanced depth imaging (EDI) analysis of choroid in our study. Blood arterial pressure effects can be correlated with choroidal thickness and many hidden maculopathies can be diagnosed at early stage. More studies can be conducted with a large sample size study to support our results.
In clinical practice,this study has valuable values which help in diagnosing optic neuropathies and maculopathies. We suggest that interocular differences in average RNFL and macular thickness of normal individuals should not exceed 11 μm and 18 μm respectively in young adults if measured with Cirrus HD-OCT. Differences greater than these values should be considered while diagnosing optic neuropathies and maculopathies in association with other clinical parameters.
REFERENCES
1 Ong LS, Mitchell P, Healey PR, Cumming RG. Asymmetry in optic disc parameters: the Blue Mountains Eye Study.InvestOphthalmolVisSci1999;40(5):849-857
2 Dalgliesh JD, Tariq YM, Burlutsky G, Mitchell P. Symmetry of retinal parameters measured by spectral-domain OCT in normal young adults.JGlaucoma2015;24(1):20-24
3 Yüksel D, Orban de Xivry JJ, Lefèvre P. Review of the major findings about Duane retraction syndrome (DRS) leading to an updated form of classification.VisionRes2010;50(23):2334-2347
4 Punjabi OS, Huang J, Rodriguez L,Lyon AT, Jampol LM, Mirza RG. Imaging characteristics of neovascular pigment epithelial detachments and their response to anti-vascular endothelial growth factor therapy.BrJOphthalmol2013;97(8):1024-1031
6 Budenz DL. Symmetry between the right and left eyes of the normal retinal nerve fiber layer measured with optical coherence tomography (an AOS thesis).TransAmOphthalmolSoc2008;106:252-275
7 Hirasawa H, Tomidokoro A, Araie M, Konno S, Saito H, Iwase A, Shirakashi M, Abe H, Ohkubo S, Sugiyama K, Ootani T, Kishi S, Matsushita K, Maeda N, Hangai M, Yoshimura N. Peripapillary retinal nerve fiber layer thickness determined by spectral-domain optical coherence tomography in ophthalmologically normal eyes.ArchOphthalmol2010;128(11):1420-1426
8 Huynh SC, Wang XY, Burlutsky G, Mitchell P. Symmetry of optical coherence tomography retinal measurements in young children.AmJOphthalmol2007;143(3):518-520
9 Mwanza JC, Durbin MK, Budenz DL; Cirrus OCT Normative Database Study Group. Interocular symmetry in peripapillary retinal nerve fiber layer thickness measured with the Cirrus HD-OCT in healthy eyes.AmJOphthalmol2011;151(3):514-521
10 Massa GC, Vidotti VG, Cremasco F, Lupinacci AP, Costa VP. Influence of pupil dilation on retinal nerve fibre layer measurements with spectral domain OCT.Eye(Lond) 2010;24(9):1498-1502
11 Knight OJ, Girkin CA, Budenz DL, Durbin MK, Feuer WJ; Cirrus OCT Normative Database Study Group.Effect of race, age, and axial length on optic nerve head parameters and retinal nerve fiber layer thickness measuredby Cirrus HD-OCT.ArchOphthalmol2012;130(3):312-318
12 Schuman JS, Pedut-Kloizman T, Hertzmark E, Hee MR, Wilkins JR, Coker JG,Puliafito CA, Fujimoto JG, Swanson EA. Reproducibility of nerve fiber layer thickness measurements using optical coherence tomography.Ophthalmology1996;103(11):1889-1898
13 Altemir I, Oros D, Elía N, Polo V, Larrosa JM, Pueyo V. Retinal asymmetry in children measured with opticalcoherence tomography.AmJOphthalmol2013;156(6):1238-1243
14 Paunescu LA, Schuman JS, Price LL, Stark PC, Beaton S, Ishikawa H, Wollstein G, Fujimoto JG.Reproducibility of nerve fiber thickness, macular thickness, and optic nerve head measurements using Stratus OCT.InvestOphthalmolVisSci2004;45(6):1716-1724
15 Hwang YH, Song M, Kim YY, Yeom DJ, Lee JW. Interocular symmetry of retinal nerve fibre layer thickness in healthy eyes:a spectral-domain optical coherence tomographic study.ClinExpOptom2014;97(6):550-554
16 Jee D, Hong SW, Jung YH, Ahn MD. Interocular retinal nerve fiber layer thickness symmetry value in normal young adults.JGlaucoma2014;23(8):e125-e131
17 Armaly MF. Genetic determination of cup/disc ratio of the optic nerve.ArchOphthalmol1967;78(1):35-43
18 Cao XS, Peng XY, You QS, Zhang YP, Jonas JB. Subfoveal choroidal thickness change after intravitrealranibizumab for idiopathic choroidal neovascularization.Retina(Philadelphia,Pa) 2014;34(8):1554-1559
19 Wei WB, Xu L, Jonas JB, Shao L, Du KF, Wang S, Chen CX, Xu J, Wang YX, Zhou JQ, You QS. Subfovealchoroidal thickness: the Beijing Eye Study.Ophthalmology2013;120(1):175-180
20 Kim HC, Cho WB, Chung H. Morphologic changes in acute central serous chorioretinopathy using spectral domain optical coherence tomography.KoreanJOphthalmol2012;26(5):347-354
21 Duan XR, Liang YB, Friedman DS, Sun LP, Wong TY, Tao QS, Bao L, Wang NL, Wang JJ. Normal macular thickness measurements using optical coherence tomography in healthy eyes of adult Chinese persons: the Handan Eye Study.Ophthalmology2010;117(8):1585-1594
22 Asefzadeh B, Cavallerano AA, Fisch BM. Racial differences in macular thickness in healthy eyes.OptomVisSci2007;84(10):941-945
·Original article·
新型频域相关断层扫描对健康年轻人视网膜各参数的测量分析
Syed Nasir Ali Shah1,张林1, 樊小娟1,邓瑾1, Faisal Shahbaz2, Umer Farooq3
(作者单位:1中国,西安 710061,西安交通大学第一附属医院,眼科;2英国,英格兰,卡莱尔,坎伯兰疗养医院;3巴基斯坦,阿伯塔巴德 22010,阿尤布医学院,社区医学系)
摘要
目的:采用新型频域相关断层扫描测量分析健康年轻人中视网膜各参数生理的不对称性。
方法:对146名健康年轻人进行横断面观察研究,采用新型频域相关断层扫描对其双眼视网膜参数(视网膜神经纤维层厚度、视盘、黄斑)进行扫描。通过右眼减去左眼所得参数值的平均差进行配对t检验。两眼间的差异采用2.5%~97.5%之间进行评估。视网膜参数相关。通过回归分析,评价性别和血压对视网膜参数的影响。
结果:两眼的视网膜神经纤维层平均厚度无统计学差异(+0.7μm,P=0.09)。两眼视网膜颞侧象限(+2.51μm,P=0.02),鼻侧象限(+2.50μm,P=0.04),钟表位右眼2点与左眼10点(+5.85μm,P=0.002),右眼3点与左眼9点(+3.20μm,P=0.005),右眼11点与左眼1点(+3.80μm,P=0.024),平均厚度(-0.034μm,P=0.013)和垂直方向杯盘比(-0.028μm,P=0.008),黄斑部鼻侧象限(+7.76μm,P=0.003)。左眼上方视网膜明显较薄(-2.40μm,P=0.03)。平均视网膜神经纤维层厚度和黄斑厚度分别为11μm和18μm。视网膜参数在双眼有中度的相关性(0.41~0.6),而两眼视网膜参数与性别、血压不相关(P<0.05)。研究表明通过新型频域相关断层扫描发现健康年轻人的视网膜神经纤维层厚度和黄斑厚度两眼间的差异分别不应超过11μm和18μm。
结论:视网膜参数的不对称性存在于健康视网膜,并对早期视网膜病变的诊断提供有价值的评估。
关键词:高分辨率光学相关断层扫描;不对称;视网膜参数
DOI:10.3980/j.issn.1672-5123.2016.2.03
通讯作者:张林, 西安交通大学第一附属医院, 研究方向:角膜. 1711056348@qq.com
作者简介:Syed Nasir Ali Shah,西安交通大学,博士,研究方向:视网膜。
