高压氧治疗噪声性耳聋的实验研究
2016-02-15李欢刘晨乔月华3于宁
李欢刘晨乔月华,3于宁
1徐州医科大学
2解放军总医院耳鼻咽喉头颈外科 耳鼻咽喉研究所
3徐州医科大学附属医院耳鼻咽喉头颈外科
·噪声性聋专辑·
高压氧治疗噪声性耳聋的实验研究
李欢1刘晨2乔月华1,3于宁2
1徐州医科大学
2解放军总医院耳鼻咽喉头颈外科 耳鼻咽喉研究所
3徐州医科大学附属医院耳鼻咽喉头颈外科
目的通过探讨高压氧治疗噪声性耳聋的时间点和疗效的关系,为临床应用提供参考。方法取清洁级健康白色红目、ABR阈值正常的豚鼠50只,雌雄不限,体重250~300g。随机分成3组,空白对照组、噪声组、噪声+高压氧治疗组(压力为2ATA,疗程10天),分别于噪声暴露后即刻、7天后、14天后给予高压氧治疗。另取5只作为噪声暴露后即刻取材组。给予脉冲噪声(压力峰值142dB SPL,脉宽0.25ms)连续暴露100次。于脉冲噪声暴露前、暴露后即刻及高压氧治疗2次后、治疗6次后、治疗10次后测听性脑干反应(ABR)。治疗结束后通过对炎症因子及氧自由基的测定观察耳蜗的代谢变化。结果与噪声组相比,噪声暴露后即刻高压氧治疗可以减轻16 kHz的ABR阈值,有统计学意义(P<0.05)。噪声暴露7天后给予高压氧治疗在click、4kHz、8 kHz、16 kHz上的ABR阈值比噪声组低(P<0.05)。噪声暴露14天后给予高压氧治疗在各频率上与噪声组相比,均无统计学差异,甚至在click、4kHz时高压氧治疗组ABR阈值高于噪声组。噪声+高压氧治疗组的8-OHdG、TNF-α、IL-1β含量较噪声组低(P<0.05),噪声+高压氧治疗组的HIF-1α含量虽较噪声组低,但无统计学意义。结论高压氧在治疗噪声性耳聋方面有显著效果,噪声暴露7天后给予高压氧治疗效果最好,噪声暴露14天后不但效果差,有的甚至有不利影响。
高压氧;噪声性耳聋;治疗
Financial funds:This work was supported by grants from the National Basic Research Program of China(973 Program)(# 2012CB967900 and#2014CB943002),the National Natural Science Foundation of China(#81271081,#81528005,#81470700 and# 81470684),theArmy Noise Project(JDZYY20132、BWS14J045、2014ZX09J14101-06C)
Declaration of interest:The authors report no conflicts of interest.
据世界卫生组织报道有11亿的青少年和青壮年由于不安全的使用个人音频设备和暴露在嘈杂的娱乐场所面临听力下降的风险[1]。噪声性耳聋是由强噪声刺激引起内耳毛细胞损伤后所产生的一种感音神经性耳聋,目前有机械性损伤和代谢性损伤学说两种机制。有学者发现强噪声可以引起耳蜗组织缺氧、缺血,产生大量的活性氧(reactive oxygen species,ROS)与活性氮(reactive nitrogen species,RNS),在直接破坏内耳细胞DNA的同时,还可启动细胞凋亡的发生[2],从而使听力下降甚至丧失。高压氧在临床广泛应用,能够通过显著提高组织血液的氧分压及血氧含量,增加血氧弥散距离,从而改善内耳听器的缺氧环境,恢复内耳听器的功能[3]。目前关于噪声性耳聋的高压氧治疗的研究虽较多[3-4],但关于干预时机的选择尚无统一的标准。本实验通过高压氧治疗噪声性听力损失后听力学的变化和分子机制的研究,探讨高压氧在噪声性耳聋治疗中的应用,为临床治疗噪声性耳聋提供直接依据。
1 材料和方法
1.1 实验动物
SPF级健康白色红目、耳廓反射灵敏、ABR阈值正常的Hartley豚鼠50只,体重250~300g,雌雄不限,购自北京维通利华实验动物有限公司。
1.2 实验试剂
8-羟基脱氧鸟苷(8-OHdG)酶联免疫检测试剂盒;肿瘤坏死因子-α酶联免疫检测试剂盒(TNF-α);白细胞介素-1β酶联免疫检测试剂盒(IL-1β);低氧诱导因子-1α酶联免疫检测试剂盒(HIF-1α)。
1.3 动物分组
随机分成3组,空白对照组(A组)15只、噪声组(B组)15只、噪声+高压氧治疗组(C组)15只,每组再随机分成3小组,分别为噪声暴露后即刻组(即A1组、B1组、C1组),噪声暴露后7天组(即A2组、B2组、C2组),噪声暴露后14天组(即A3组、B3组、C3组),每小组5只,另取5只作为噪声暴露后即刻取材组D组。
1.4 噪声暴露
将清醒状态的豚鼠固定于特制的笼内,放在专用的消声室自由声场中,扬声器置于动物头前方水平位,距离豚鼠双耳约2cm,给予压力峰值为142dB SPL,脉宽为0.25ms的脉冲噪声,连续暴露100次。
1.5 高压氧治疗(Hyperbaric oxygen therapy,HBOT)
C1组于噪声暴露后即刻、C2组于噪声暴露后第7天、C3于噪声暴露后第14天分别开始给予高压氧治疗,采用NG90-ⅢB单人医用高压氧舱,压力为2ATA,升压、稳压、降压时间分别为15min、60min、15min,总用时为90min,每天1次,疗程为10天。
1.6 听力检测
于脉冲噪声暴露前、暴露后即刻、高压氧治疗2次后、治疗6次后、治疗10次后测试听性脑干反应(ABR)阈值。测试采用美国TDT系统,在隔声屏蔽室内将清醒状态的豚鼠固定于特制的装置中,使用针式电极,记录电极置于颅顶正中皮下,参考电极置于测试耳耳廓皮下,接地电极置于对侧耳耳廓皮下,采用短声(click)、短纯音(Tone Burst)4000Hz、8000Hz、16000Hz、32000Hz为刺激声,每次刺激1024次,以能分辨出可重复的ABR波Ⅲ的最低刺激强度来判断阈值。
1.7 酶联免疫吸附测定试剂盒(Elisa试剂盒)测定耳蜗组织中8-OHdG、TNF-α、IL-1β、HIF-1α的水平
高压氧治疗结束并测试完ABR阈值后,A1、B1、C1、D组中分别取5只动物,D组噪声暴露后即刻进行,10%水合氯醛(0.4mL/100g)腹腔注射麻醉,断头后取出双耳听泡,分离出耳蜗,放入预冷生理盐水中,冰浴下在解剖显微镜下去除骨性蜗壳,在基底部断窝轴,取蜗壳内所有组织,放入2mL EP管中,1只豚鼠的2个耳蜗组织作为1个标本,操作过程需迅速,最好控制在3分钟之内,称重后,以标本重量g:生理盐水体积mL=1:9的比例,加入相应体积的生理盐水,冰浴下用一次性研磨杵研磨,研磨充分后,放入离心机中,4℃、9000G离心20分钟,取上清,放入-80℃冰箱中备用。8-OHdG、TNF-α、IL-1β、HIF-1α含量的测定方法按照Elisa试剂盒的说明书进行。
1.8 统计学方法
2 结果
2.1 听力检测结果
脉冲噪声暴露前,各组的ABR阈值基本相同,差异无统计学意义(P>0.05),脉冲噪声暴露后即刻,噪声组与噪声+高压氧治疗组的ABR阈值均较空白对照组的阈值高,差异有统计学意义(P<0.01),而噪声组和噪声+高压氧治疗组之间的ABR阈值的差异无统计学意义(P>0.05)。与噪声组相比,噪声暴露后即刻高压氧治疗可以减轻16 kHz的ABR阈值,差异有统计学意义,P<0.05(F=6.721,P=0.018),噪声暴露7天后给予高压氧治疗在click、4kHz、8 kHz、16 kHz上的ABR阈值比噪声组低,P<0.05(F=6.453,P= 0.021;F=12.393,P=0.002;F=12.827,P=0.002;F= 8.627,P=0.009),其中在4kHz、8 kHz、16 kHz上的ABR阈值与噪声组相比,差异有显著的统计学意义(P<0.01),噪声暴露14天后给予高压氧治疗在各频率上与噪声组相比,差异均无统计学意义,甚至在click、4kHz时高压氧治疗组ABR阈值高于噪声组。在高压氧治疗开始后,比较各时间点的ABR阈值结果,噪声暴露后即刻组中,在频率为16 kHz时,高压氧治疗2次后、6次后、10次后噪声+高压氧治疗组的ABR阈值均较噪声组低(P<0.05);噪声暴露后7天组中,在给予click、4kHz、8 kHz、16 kHz声音时,高压氧治疗2次后、6次后、10次后噪声+高压氧治疗组的ABR阈值明显低于噪声组(P<0.01),在给予32 kHz声音时,高压氧治疗10次后噪声+高压氧治疗组的ABR阈值低于噪声组(P<0.05);噪声暴露后14天组中,各频率在高压氧治疗后各时间点的ABR阈值噪声+高压氧治疗组与噪声组之间的差异无统计学意义(P>0.05)。(见图1-图3)
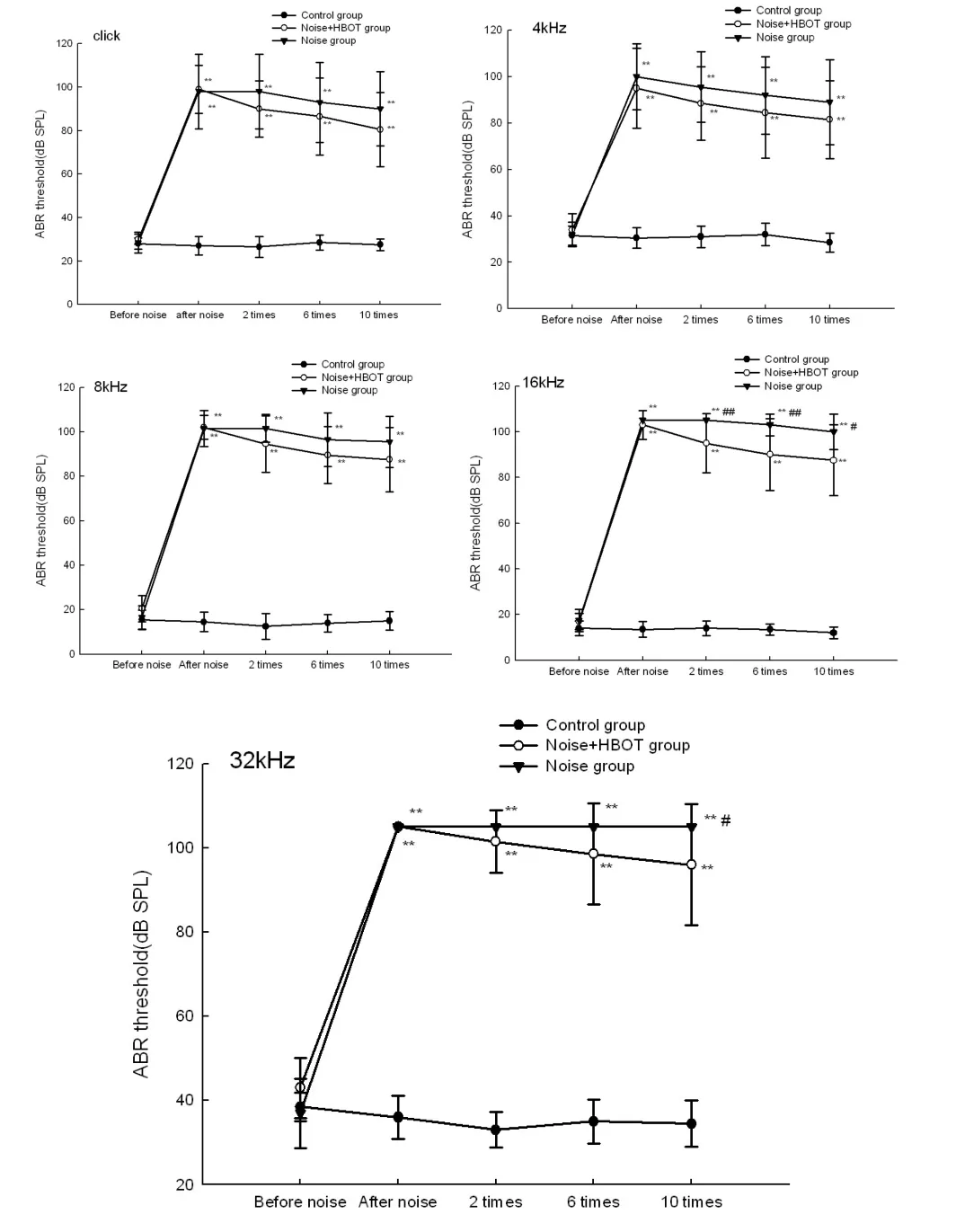
图1 噪声暴露后即刻组各组豚鼠ABR阈值的比较。脉冲噪声暴露前,各组的ABR阈值正常,差异无统计学意义(P>0.05),脉冲噪声暴露后即刻,噪声组与噪声+高压氧治疗组的ABR阈值均较空白对照组的阈值高,差异有统计学意义(P<0.01),而噪声组和噪声+高压氧治疗组之间的ABR阈值的差异无统计学意义(P>0.05)。与噪声组相比,噪声暴露后即刻高压氧治疗可以减轻16 kHz的ABR阈值,差异有统计学意义,P<0.05(F= 6.721,P=0.018),在频率为16 kHz时,高压氧治疗2次后、6次后、10次后噪声+高压氧治疗组的ABR阈值均较噪声组低(P<0.05)。注:**P<0.01:vs.空白对照组;#P<0.05,##P<0.01:噪声+高压氧治疗组vs.噪声组。n=10耳Fig.1 Comparison of ABR thresholds for guinea pigs in each group in the group of immediately after exposure to noise.The threshold of ABR was normal before exposure to pulse noise, and there was no significant difference among the groups(P>0.05),The ABR thresholds of the noise group and the noise+ HBOT group were higher than those of the control group at the moment of impulse noise exposure(P<0.01),but between the noise group and the noise+HBOT therapy group The difference of ABR threshold was not significant(P>0.05).Compared with the noise group,hyperbaric oxygen therapy immediately after exposure to noise can reduce the ABR threshold of 16 kHz,the difference was statistically significant,P<0.05(F=6.721,P= 0.018).At the frequency of 16 kHz,the ABR thresholds of the noise+HBOT group were lower than those of the noise group after 2 times,6 times,and 10 times of hyperbaric oxygen therapy(P<0.05).Note:**P<0.01:vs.control group;#P<0.05,##P<0.01:noise+HBOT group vs.noise group.n=10ears
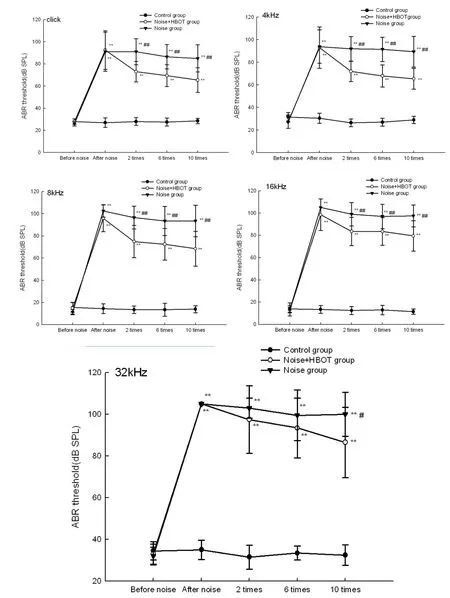
图2 噪声暴露后7天组各组豚鼠ABR阈值的比较。脉冲噪声暴露前,各组的ABR阈值正常,差异无统计学意义(P>0.05),脉冲噪声暴露后即刻,噪声组与噪声+高压氧治疗组的ABR阈值均较空白对照组的阈值高,差异有统计学意义(P<0.01),而噪声组和噪声+高压氧治疗组之间的ABR阈值的差异无统计学意义(P>0.05)。与噪声组相比,噪声暴露7天后给予高压氧治疗在click、4kHz、8 kHz、16 kHz上的ABR阈值比噪声组低,P<0.05(F=6.453,P=0.021;F=12.393,P=0.002;F= 12.827,P=0.002;F=8.627,P=0.009),在给予click、4kHz、8 kHz、16 kHz声音时,高压氧治疗2次后、6次后、10次后噪声+高压氧治疗组的ABR阈值明显低于噪声组(P<0.01),在给予32 kHz声音时,高压氧治疗10次后噪声+高压氧治疗组的ABR阈值低于噪声组(P<0.05)。注:**P<0.01:vs.空白对照组;#P<0.05,##P<0.01:噪声+高压氧治疗组vs.噪声组。n=10耳Fig.2 Comparison of ABR thresholds for guinea pigs in each group in the group of 7 days after noise exposure.The threshold of ABR was normal before exposure to pulse noise,and there was no significant difference among the groups(P>0.05),The ABR thresholds of the noise group and the noise+HBOT group were higher than those of the control group at the moment of impulse noise exposure(P<0.01),but between the noise group and the noise+HBOT therapy group The difference of ABR threshold was not significant(P>0.05).Compared with the noise group,the ABR thresholds of the guinea pigs at click、4kHz、8 kHz、16 kHz which were given the hyperbaric oxygen therapy at 7 days after noise exposure were lower than that of the noise group,P<0.05(F=6.453,P=0.021;F=12.393,P=0.002;F=12.827,P=0.002;F=8.627,P=0.009).The thresholds of ABR in noise+HBOT group were significantly lower than those in the noise group after 2 times,6 times,and 10 times of hyperbaric oxygen therapy at click,4 kHz,8 kHz,16 kHz(P<0.01).At the frequency of 32 kHz,The ABR threshold of the noise+HBOT group after 10 times of hyperbaric oxygen therapy was lower than that of the noise group(P<0.05).Note:**P<0.01:vs.control group;#P<0.05,##P<0.01:noise+HBOT group vs.noise group.n=10ears
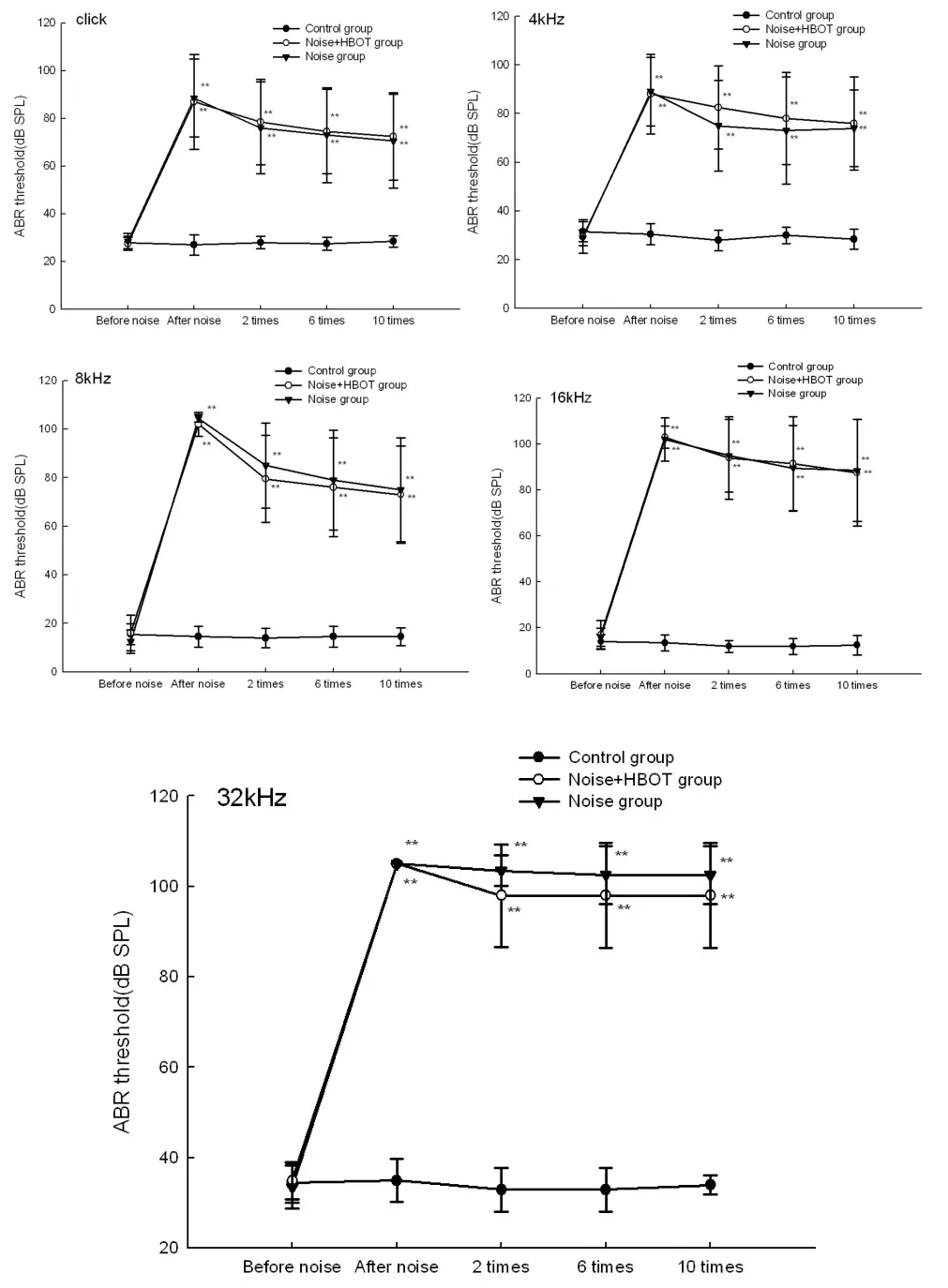
图3 噪声暴露后14天组各组豚鼠ABR阈值的比较。脉冲噪声暴露前,各组的ABR阈值正常,差异无统计学意义(P>0.05),脉冲噪声暴露后即刻,噪声组与噪声+高压氧治疗组的ABR阈值均较空白对照组的阈值高,差异有统计学意义(P<0.01),而噪声组和噪声+高压氧治疗组之间的ABR阈值的差异无统计学意义(P>0.05)。噪声暴露14天后给予高压氧治疗在各频率上与噪声组相比,差异均无统计学意义(P>0.05),各频率在高压氧治疗后各时间点的ABR阈值噪声+高压氧治疗组与噪声组之间的差异无统计学意义(P>0.05)。注:**P<0.01:vs空白对照组。n=10耳Fig.3 Comparison of ABR thresholds for guinea pigs in each group in the group of 14 days after noise exposure.The threshold of ABR was normal before exposure to pulse noise,and there was no significant difference among the groups(P>0.05), The ABR thresholds of the noise group and the noise+HBOT group were higher than those of the control group at the moment of impulse noise exposure(P<0.01),but between the noise group and the noise+HBOT therapy group The difference of ABR threshold was not significant(P>0.05).Given the hyperbaric oxygen therapy at 14 days after noise exposure, there was no significant difference in all frequency between the noise+HBOT group and the noise group(P>0.05).There was no statistically significant difference in ABR threshold between noise+HBOT group and noise group at each time point after hyperbaric oxygen therapy in each frequency(P>0.05).Note:** P<0.01:vs.control group.n=10ears
2.2 耳蜗内细胞因子测定结果
噪声暴露后即刻,耳蜗组织中的8-OHdG较空白对照组增加,P<0.05(P=0.029),噪声组8-OHdG的含量高于空白对照组和噪声+高压氧治疗组,P<0.05(P=0.033;P=0.039),空白对照组与噪声+高压氧治疗组之间的8-OHdG含量基本相同,无统计学差异。(见图4)
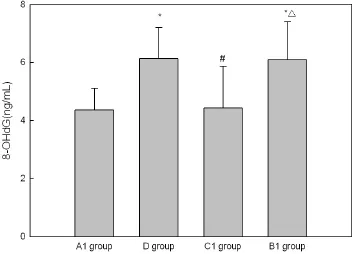
图4 脉冲噪声前后各组豚鼠耳蜗组织中8-OHdG含量的比较。脉冲噪声暴露后即刻,豚鼠耳蜗组织中8-OHdG含量增加,P<0.05(P=0.029),噪声组8-OHdG的含量高于空白对照组和噪声+高压氧治疗组,P<0.05(P=0.033;P=0.039)。注:A1组:空白对照组;D组:噪声暴露后即刻取材组;C1组:噪声+高压氧治疗组(噪声暴露后即刻);B1组:噪声组;*P<0.05 VS A1组;#P<0.05 D组VS C1组;△P<0.05 C1组VS B1组。n=5Fig.4 Comparison of 8-OHdG levels in the cochlea of guinea pigs before and after impulse noise.The content of 8-OHdG in the cochlea of guinea pigs was increased immediately after the impulse noise exposure,P<0.05(P=0.029),The content of 8-OHdG in the noise group was higher than that in the control group and noise+HBOT group,P<0.05(P=0.033;P=0.039). Note:A1 group:Control group;D group:Drawn the materials from guinea pigs Immediately after exposure to noise;C1 group:Noise+HBOT group(immediately after noise exposure);B1 group:Noise group;*P<0.05 VS A1 group;#P<0.05 D group VS C1 group;△P<0.05 C1 group VS B1 group.n=5
脉冲噪声暴露后即刻,豚鼠耳蜗组织中IL-1β的含量较空白对照组明显增高,P<0.01(P=0.001),噪声组IL-1β的含量明显高于空白对照组和噪声+高压氧治疗组,P<0.01(P=0.005;P=0.001)。噪声+高压氧治疗组IL-1β的含量低于空白对照组,但无统计学差异。(见图5)
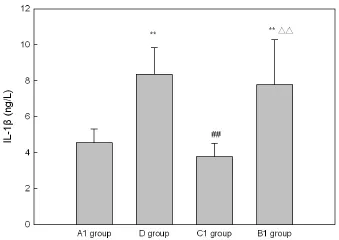
图5 脉冲噪声前后各组豚鼠耳蜗组织中IL-1β含量的比较。脉冲噪声暴露后即刻,豚鼠耳蜗组织中IL-1β含量明显增加,P<0.01(P=0.001),噪声组IL-1β的含量明显高于空白对照组和噪声+高压氧治疗组,P<0.01(P=0.005;P=0.001)。注:A1组:空白对照组;D组:噪声暴露后即刻取材组;C1组:噪声+高压氧治疗组(噪声暴露后即刻);B1组:噪声组;**P<0.01 VS A1组;##P<0.01 D组VS C1组;△△P<0.01 C1组VS B1组。n=5Fig.5 Comparison of the levels of IL-1β in the cochlea of guinea pigs before and after impulse noise.Immediately after exposure to impulse noise,the concentration of IL-1β in the cochlea of guinea pigs was significantly increased,P<0.01(P=0.001). The content of IL-1β in the noise group was significantly higher than that in the control group and noise+HBOT group,P<0.01(P=0.005;P=0.001).Note:A1 group:Control group;D group: Drawn the materials from guinea pigs Immediately after exposure to noise;C1 group:Noise+HBOT group(immediately after noise exposure);B1 group:Noise group;**P<0.01 VS A1 group;##P<0.01 D group VS C1 group;△△P<0.01 C1 group VS B1 group.n=5
脉冲噪声暴露后即刻,豚鼠耳蜗组织中TNF-α的含量较空白对照组增高,P<0.05(P=0.015),噪声+高压氧治疗组TNF-α的含量低于噪声组,P<0.05(P= 0.042)。噪声+高压氧治疗组TNF-α的含量低于空白对照组,但无统计学差异。(见图6)
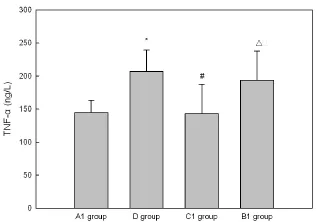
图6 脉冲噪声前后各组豚鼠耳蜗组织中TNF-α含量的比较。脉冲噪声暴露后即刻,豚鼠耳蜗组织中TNF-α含量增加,P<0.05(P=0.015),噪声组TNF-α的含量高于噪声+高压氧治疗组,P<0.05(P=0.042)。注:A1组:空白对照组;D组:噪声暴露后即刻取材组;C1组:噪声+高压氧治疗组(噪声暴露后即刻);B1组:噪声组;*P<0.05 VS A1组;#P<0.05 D组VS C1组;△P<0.05 C1组VS B1组。n=5
脉冲噪声暴露后即刻,豚鼠耳蜗组织中HIF-1α的含量较空白对照组增高,P<0.05(P=0.031),噪声组HIF-1α的含量高于空白对照组,P<0.05(P=0.03),噪声组HIF-1α的含量高于噪声+高压氧治疗组,但无统计学意义。噪声+高压氧治疗组HIF-1α的含量高于空白对照组,但无统计学差异。(见图7)
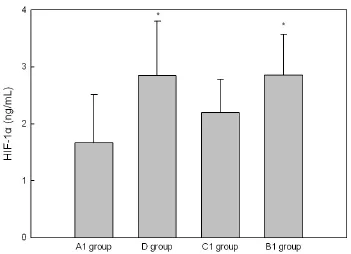
图7 脉冲噪声前后各组豚鼠耳蜗组织中HIF-1α含量的比较。脉冲噪声暴露后即刻,豚鼠耳蜗组织中HIF-1α含量增加,P<0.05(P=0.031),噪声组HIF-1α的含量高于空白对照组,P<0.05(P=0.03),噪声+高压氧治疗组的HIF-1α含量比噪声组低,但无统计学意义。注:A1组:空白对照组;D组:噪声暴露后即刻取材组;C1组:噪声+高压氧治疗组(噪声暴露后即刻);B1组:噪声组;*P<0.05 VS A1组。n=5Fig.7 Comparison of HIF-1α levels in the cochlea of guinea pigs before and after impulse noise.The content of HIF-1αin the cochlea of guinea pigs was increased immediately after the impulse noise exposure,P<0.05(P=0.031),The content of HIF-1αin the noise group was higher than that in the control group,P<0.05(P=0.03).The level of HIF-1α in the noise+ HBOT group was lower than that in the noise group,but there was no statistical significance.Note:A1 group:Control group; D group:Drawn the materials from guinea pigs Immediately after exposure to noise;C1 group:Noise+HBOT group(immediately after noise exposure);B1 group:Noise group;*P<0.05 VSA1 group.n=5
3 讨论
强脉冲噪声引起的噪声性耳聋的致病机制[2,5,6]主要为机械性损伤学说以及继发的代谢性损伤学说。强脉冲噪声首先引起毛细胞损伤或缺失,纤毛倒伏,支持细胞损伤,血管破裂,听神经损伤等机械性损伤,导致耳蜗组织内缺血、缺氧,产生大量的ROS与RNS,破坏耳蜗内的酶代谢平衡以及离子浓度的稳定,引起耳蜗内的细胞膜和细胞核内的DNA损伤,启动细胞凋亡的发生,也能引起促炎细胞因子的释放,从而使听力下降甚至丧失。
8-OHdG是DNA损伤的标志物,Kurioka等[7]的研究表明在豚鼠中8-OHdG的免疫反应性在噪声暴露后5h最强。TNF-α、IL-1β是参与炎症反应的主要细胞因子,Fujioka等[8]的研究显示IL-6和IL-1β在噪声暴露后的第3小时增加并在24小时内下降至基线水平。在TNF-α中也观察到类似的趋势。Arslan等[9]研究结果表明HBOT-3小时组的IL-1β水平显著高于噪声组、地塞米松组和HBOT-24小时组(P<0.05);在3个治疗组,噪声组和对照组中,TNF-α没有显著差异(P>0.05)。HIF-1α是反应体内低氧情况的指标,氧浓度的降低可以诱导HIF-1α的表达。本文中主要检测了以上这四种物质在各组中的含量,噪声暴露后即刻,耳蜗组织中这四种物质均增多(P<0.05),给予高压氧治疗后,8-OHdG、TNF-α、IL-1β的含量较噪声组低(P<0.05),HIF-1α含量虽较噪声组低,但无统计学意义。综合以上结果,可以看出,高压氧治疗噪声性耳聋的机制与减少DNA损伤、减轻炎症反应及改善缺氧情况有关。
高压氧治疗噪声性耳聋的效果及开始干预的时机目前仍存在很大争议,尚无公认的统一标准。Co⁃lombari等[10]的研究表明,噪声暴露后即刻给予高压氧治疗,ABR阈值与对照组相比无统计学差异,但可减少外毛细胞的损伤。Lamm等[11]的实验结果显示在噪声暴露后1h给予高压氧治疗更有效。Kuok⁃kanen等[12]提到HBOT在声创伤后2-3h开始给予有有益的效果。但也有部分研究有相反的结果,如Ca⁃kir等[13]的研究显示在给予高压氧治疗10d后,对照组和6h治疗组、24h治疗组、48h治疗组的信噪比均恢复到噪声暴露前水平而噪声暴露后1h治疗组和噪声暴露后2h治疗组未完全恢复。另一项研究也显示HBOT-24小时组的ABR阈值显著低于HBOT-3小时组,噪声暴露后3h给予HBOT不但没有益处,反而有害[9]。本文中主要选取了三个时间点给予高压氧治疗,从结果看,与噪声组相比,噪声暴露后即刻给予高压氧治疗可以减轻16 kHz的ABR阈值,有统计学意义(P<0.05)。噪声暴露7天后给予高压氧治疗除了32kHz外,其余各频率ABR阈值均较噪声组低(P<0.05)。噪声暴露14天后给予高压氧治疗在各频率上与噪声组相比,均无统计学差异,甚至在click、4kHz时高压氧治疗组ABR阈值高于噪声组。高压氧在治疗噪声性耳聋方面有显著效果,噪声暴露7天后给予高压氧治疗效果最好,噪声暴露14天后不但效果差,有的甚至有不利影响。有实验研究表明,在噪声暴露后7-10天是自由基产生的高峰期,有时自由基的产生甚至可持续到14天[14]。这很好的解释了本实验的测听结果,噪声暴露后即刻给予高压氧治疗,虽有一定效果,但不理想,可能与豚鼠处于损伤的急性期,体内的酶代谢失衡,有害物质产生过多,高压氧虽可改善体内缺氧情况,但高压也可使一些损伤血管闭合,造成血管阻塞,形成血栓,妨碍听力的恢复。噪声暴露后7天给予高压氧治疗,此时正处于自由基产生的高峰期,高压氧治疗可以有效地减少这些自由基的产生,减轻继发的代谢性损伤,从而改善听力。噪声暴露后14天给予高压氧治疗,此时机械性损伤以及继发的代谢性损伤已经形成,高压氧治疗效果不佳。
高压氧治疗有一定的副作用,如中耳压力失衡[15],咽鼓管功能障碍[16],耳部或窦性气压性损伤[17],某种程度的幽闭性焦虑[15、17]等。在临床中,应该给予患者正确的治疗指导以及相应的心理干预,以减少副作用的发生,应该综合考虑患者情况,合理应用这一治疗方法。
本文研究了不同时间点给予高压氧治疗后听力的恢复情况,为临床上使用高压氧治疗噪声性耳聋的干预时机提供了参考。
1 Laura Sminkey.1.1 billion people at risk of hearing loss.http://www. who.int/mediacentre/news/releases/2015/ear-care/en/
2 李兴启,杨仕明,王秋菊,等.耳蜗病理生理学.北京:人民军医出版社.2011:218-220. Li XQ,Yang SM,Wang QJ,et al.Cochlear pathophysiology.Bei jing: People's Military Medical Press.2011:218-220.
3 李斌,郑倩玲,黄家文,等.64例职业性噪声聋患者高压氧治疗效果观察[J].中国职业医学,2012,39(3):218-219.
Li B,Zheng QL,Huang JW,et al.Observation on effect of hyperbar⁃ic oxygen therapy in 64 cases of occupational noise-induced deaf⁃ness[J].China Occupational Medicine,2012,39(3):218-219.
4 谭军武,李良波,彭洪.110例噪声性耳聋患者的高压氧综合治疗效果[J]中华劳动卫生职业病杂志,2014,32(10):767-768.
Tan JW,Li LB,Peng H.Clinical analysis of using hyperbaric oxygen comprehensive therapy for the treatment of 110 cases noise induced deafness[J]Zhong hua lao dong wei sheng zhi ye bing za zhi,2014,32 (10):767-768.
5 朱恒涛,管俐娜,江红群.噪声性耳聋病理机制的研究进展[J].中华耳科学杂志,2016,14(5):681-685.
Zhu HT,Guan LN,Jiang HQ.Pathological mechanisms of noise-in⁃duced hearing loss:A review of recent research[J].Chinese Journal of Otology,2016,14(5):681-685.
6 韩维举,陈星睿.噪声暴露引起耳蜗损伤机制的研究[J].中华耳科学杂志,2013,11(3):357-362.
Han WJ,Chen XR.Mechanisms of Noise Induced Cochlea Injury[J]. Chinese Journal of Otology,2013,11(3):357-362.
7 Kurioka T.Matsunobu T,Satoh Y.et a1.Inhaled hydrogen gas thera⁃py for prevention of noise—induced hearing loss through reducing reactive oxygen species[J].Neurosci Res,2014,89:69—74.
8 Fujioka M,Kanzaki S,Okano HJ,et al.Proinflammatory cytokines expression in noise-induced damaged cochlea.[J]Neurosci Res 2006;83(4):575-583.
9 Arslan HH,Satar B,Serdar MA,et a1.Effects of hyperbaric oxygen and dexamethasone on proinflammatory cytokines of rat cochlea in noise—induced hearing loss[J].Otol Neurotol,2012,33(9):1672—1678.
10 0lomba ri GC,Rossato M,Feres O,et a1.Effects of hyperbaric oxy⁃gen treatment on auditory hair cells after acute noise damage[J].Eur Arch Otorhinolaryngol,2011,268(1):49-56.
11 Lamm K.Arnold W.Successful Treatment of Noise Induced Co⁃chlear Ischemia,Hypoxia,and Hearing Loss[J].Ann NY Acad sci,1999,884:233—248.
12 Kuokkanen J,Aarnisolo AA,Ylikoski J.Efficiency of hyperbaric oxy⁃gen therapy in experimental acute acoustic trauma from firearms.[J] Acta Otolaryngol Suppl 2000;543:132-134.
13 Cakir BO,Ercan I,Civelek S,et a1.Negative effect of immediate hyperbaric oxygen therapy in acute acoustic trauma[J].Otol Neu⁃rotol,2006,27(4):478—483.
14 Yamashita D,Jiang H,Schacht J,et al.Delayed production of free radicals following noise exposure.[J]Brain Res.2004,1019(1-2): 201-209.
15 Plafki C,Peters P,Almeling M,Welslau W,Busch R.Complications and side effects of hyperbaric oxygen therapy.[J]Aviat Space Envi⁃ron Med.2000;71(2):119-124.
16 Fernau JL,Hirsch BE,Derkay C,Ramasastry S,Schaefer SE.Hyper⁃baric oxygen therapy:effect on middle ear and eustachian tube func⁃tion.[J]Laryngoscope.1992;102(1):48-52.
17 Korpinar S,Alkan Z,Yigit O,et al.Factors influencing the outcome of idiopathic sudden sensorineural hearing loss treated with hyper⁃baric oxygen therapy.[J]Eur Arch Otorhinolaryngol.2011;268(1): 41-47.
An experimental study on hyperbaric oxygen therapy for noise-induced hearing loss
LI Huan1,LIU Chen2,QIAO Yuehua1,3,YU Ning2
1 Xuzhou Medical University
2 Department of Otorhinolaryngology Head and Neck Surgery,Chinese PLA General Hospital&Ear Institute
3 Department of Otorhinolaryngology Head and Neck Surgery,Affiliated Hospital of Xuzhou Medical University Corresponding author:QIAO Yuehua Email:oto8558@163.com
ObjectiveTo study the timing and efficacy of hyperbaric oxygen therapy(HBOT)in treating noise-induced hearing loss,for potential translation to clinical applications.MethodsFifty healthy guinea pigs with normal ABR thresholds,weighing 250-300 g were used.Forty five guinea pigs were randomly divided into 3 groups,i.e.control,noise exposure,noise+hyperbaric oxygen therapy(2ATA,10 days)groups.HBOT was given immediately,and at 7 and 14 days after noise exposure.The rest five guinea pigs were randomly selected as specimen donors immediately after noise exposure.Impulse noise(peak sound pressure 142 dB SPL,pulse width 0.25 ms)was given at 100 pulses in succession.Auditory brainstem responses(ABRs)were measured before and immediately after exposure,and repeated after two,six and ten sessions of hyperbaric oxygen therapy.At the end of HBOT,changes in cochlear metabolism were measured by levels of inflammatory cytokines and oxygen free radicals.ResultsCompared with the noise exposure group,hyperbaric oxygen therapy immediately after noise exposure led to reduced ABR threshold shifts at 16 kHz(P<0.05).Thresholds of click ABRs and tone bursts ABRs at 4,8,and 16 kHz were better in the hyperbaric oxygen therapy group on Day 7(P<0.05)than those in thenoise exposure only group.There was no significant difference at all tested frequencies between the noise exposure and the hyperbaric oxygen therapy groups on Day 14 day,with click and 4 kHz tone burst ABR thresholds in the hyperbaric oxygen therapy group being somewhat worse than those in the noise exposure group.Levels of 8-OHdG,TNF-α and IL-1β in the hyperbaric oxygen treated group were lower than those in the noise only group(P<0.05).The level of HIF-1α in noise+hyperbaric oxygen treated group was also lower than that in the noise exposure group,but showing no statistical significance. Conclusion HBOT has a significant effect in treating noise-induced hearing loss,showing its best effects on Day 7 following exposure to noise.Its effects are not only poor on Day14 after exposure to noise,but show signs of adverse effects.
Hyperbaric oxygen;Noise-induced hearing loss;Therapy
R764
A
1672-2922(2016)06-740-7
2016-12-09)
10.3969/j.issn.1672-2922.2016.06.009
本文由国家973计划重大科学研究计划干细胞项目(2012CB967900与2014CB943002)、国家自然基金项目(81271081、81528005、81470700与81470684)、军队噪声项目(JDZYY20132、BWS14J045、2014ZX09J14101-06C)支持完成。
李欢,硕士,研究方向:噪声性耳聋的防治
李欢和刘晨为并列第一作者
乔月华,Email:oto8558@163.com
