Warm HTK donor pretreatment reduces liver injury during static cold storage in experimental rat liver transplantation
2015-12-24
Berlin, Germany
Warm HTK donor pretreatment reduces liver injury during static cold storage in experimental rat liver transplantation
Wenzel Schoening, Veeravorn Ariyakhagorn, Thomas Schubert, Peter Olschewski, Andreas Andreou, Peter Neuhaus, Johann Pratschke and Gero Puhl
Berlin, Germany
BACKGROUND: Organ shortage has led to an increased number of transplantations from extended criteria donors. These organs are more vulnerable to ischemia-reperfusion injury. Thus, improvement of organ preservation is needed. HTK is a widely used preservation solution for static cold storage in liver transplantation. The present study was to investigate the beneficial effect of warm HTK donor pretreatment on liver preservation.
METHODS: Male inbred Wistar rats (weighing 230-260 g) served as donors and recipients (n=6/group). Donors of treatment groups received i.v. 0.01 mL/g body weight (BW) warm (21 ℃) HTK systemically 15 minutes prior to cold perfusion. Control groups received 0.01 mL/g BW warm (21 ℃) NaCl 0.9%. Following pretreatment, donors were flushed with 4 ℃cold HTK, livers were explanted and stored in 4 ℃ HTK for six hours. Thereafter orthotopic liver transplantation was performed. Recipients were harvested four hours, two and five days after reperfusion and blood and liver tissue samples were obtained. Blood samples were analyzed for AST, ALT, lactate dehydrogenase and bilirubin. Liver histological analysis as well as tissue analysis for pro-MMP2, MMP2 and pro-MMP9 using zymography was conducted.
RESULTS: Treatment groups showed significantly lower ALT and lactate dehydrogenase levels as well as significantly lower activities of pro-MMP2, MMP2 and pro-MMP9. Histological analysis revealed only minor damage in all groups.
CONCLUSIONS: The new concept of warm HTK pretreatment significantly reduced ischemia-reperfusion injury. The reduced ischemia-reperfusion injury was due to MMP inhibition. Warm HTK donor pretreatment is easy to handle and could further improve HTK's potency in liver preservation.
(Hepatobiliary Pancreat Dis Int 2015;14:596-602)
experimental liver transplantation;
static cold storage;
organ preservation;
ischemia-reperfusion injury
Introduction
Over the last decades, improved outcomes after liver transplantation have led to an alarming"organ shortage". Thus, more transplants of socalled "extended criteria donor" (ECD) livers are performed. ECD organs are more vulnerable to ischemiareperfusion injury (IRI). This is reflected by higher rates of initial poor and non-function, as well as worse graft and patient outcome.[1]Nevertheless, expanding criteria for donation reduces waiting time[2]and mortality on the waiting list.[3]
Using ECD organs puts more challenges on preservation. Liver preservation is currently based on static cold storage at 4 ℃ to reduce metabolism and decelerate damage caused by oxygen and substrate shortage. However, cold storage leads to damage itself (e.g. by inducing apoptosis and reduction of substrate intake into the cell by lowering activity of trans-membraneous transporter activity).[4]For a better preservation, not only metabo-lism has to be reduced, but also substrate supply has to be guaranteed. The formulation of Bretschneider's Histidine-Tryptophan-Ketoglutarate (HTK) solution was initially conceived for mild hypothermia and cardioplegia in cardiac surgery with the concept to protect against ischemia by accumulation of a potent buffer (histidine), energy and membrane stabilizing substrates (ketoglutarate and tryptophan).[5]Besides buffering capacity and substrate supply HTK provides inhibitors of matrix metalloproteinases (MMP).[6]Especially the activation of so-called "gelatinases A and B" pro-MMP2, MMP2 and pro-MMP9, MMP9 is harmful during cold ischemia and warm reperfusion.[7]Recently MMP9 inhibition was anew shown to attenuate IRI.[8]
We suppose that an essential part of HTKs protective potency is lost by using it only as cold (4 ℃) flushing and storage solution because the reduction of uptake of its ingredients is inevitable: the activity of trans-membranous transporters at 4 ℃ is substantially lowered. We conducted an experimental study with 21 ℃ warm HTK intravenous infusion to the donor in a rodent liver transplant model,[9]aiming to enrich the donor liver with HTK prior to organ procurement and static cold storage and thus, reduce IRI and achieve a better preservation.
Methods
Experimental protocol
The new concept was to pretreat donor animals systemically with warm (21 ℃) HTK by intravenous administration prior to perfusion with cold (4 ℃) HTK. We hypothesized that (i) warm (21 ℃) donor pretreatment reduces liver transplant injury; and (ii) reduced liver transplant injury is due to (among others) MMP inhibition. To test our hypotheses, the following endpoints were measured at three time points (four hours, two and five days) after transplantation: blood levels of aminotransferases (AST and ALT), lactate dehydrogenase (LDH), bilirubin; tissue activity of MMPs (pro-MMP2, MMP2, and pro-MMP9); and histological analysis.
The three different time points were chosen to ensure measurements at different stages in the development of and regeneration from IRI. The 4-hour time point was chosen as peak level of injury, two and five days as regeneration stages. Cursio et al[10]showed that MMPs have different time courses in their activation in the process of IRI, meaning MMP9 is induced during the early phase of injury associated with inflammation and increased necrosis/apoptosis, whereas MMP2 is essentially detectable during recovery phase of liver injury corresponding to hepatocyte regeneration.
Animals
Healthy male inbred Wistar rats (weighing 230-260 g, aged 8-10 weeks) served as donors and recipients. They were purchased from Harlan and Winkelmann (Borchen, Germany) and were housed in our animal facility located at Charité Campus Virchow Klinikum, Berlin, Germany, approximately one week before each experiment. Animals were examined after delivery and kept in speciesappropriate cages with free access to water and standard rat chow at a day and night cycle of 12 hours. "Principles of laboratory animal care" were conducted, and the current version of the German Law on the Protection of Animals was complied with.[11]
Animals were randomly assigned to three treatment or control groups (G1-G6) (n=6/group) according to three different recipient harvest times after transplantation (four hours, two and five days); treatment groups: G1 (4h), G3 (2d), G5 (5d); control groups: G2 (4h), G4 (2d), G6 (5d). Before any operation procedure (organ retrieval, transplant or harvesting of recipients) animals were starved for 24 hours with free access to water.
Grafting technique and "pretreatment"
Donor and recipient operation was performed according to Lee with modifications concerning arterial and bile duct dissection and reconstruction. Our well established model of rat liver transplantation is described in detail elsewhere.[9]Briefly, after surgical preparation of the liver, application of pretreatment was performed intravenously by slow manual injection of saline or HTK, respectively. Donor animals were pretreated either with warm (21 ℃) HTK solution (Custodiol®, Dr. F. Köhler Chemie GmbH, Alsbach-Hähnlein, Germany) dosage 0.01 mL/g body weight (BW) (treatment groups G1, G3, G5), or warm (21 ℃) commercially available, sterile 0.9% saline solution, dosage 0.01 mL/g BW (control groups G2, G4, G6). For a 250 g weighing rat, 2.5 mL HTK or saline was administered. The dosage of 0.01 mL/g BW was empirically chosen to avoid volume overload of the donor as well as complications that might arise from potassium administration (HTK contains 9 mmol/L potassium). Translated into the clinical field, a dosage of 0.01 mL/g BW would mean approximately 800 mL for an 80 kg BW donor.
During pretreatment, regular circulation and natural perfusion of the liver via the hepatic artery and portal vein were maintained. Fifteen minutes after pretreatment, the portal vein was cannulated and hydrostatic-passive cold perfusion with 30 mL 4 ℃ HTK via a portal vein catheter (16G cannula) was applied, followed by cannulating the coeliac trunk with a 24G cannula and manual rinsing with 2 mL 4 ℃ HTK. Livers were then removedand stored in 4 ℃ HTK 6 hours before transplantation [i.e. cold ischemia time (CIT) 6 hours].
CIT and sew-in time were not different significantly between the groups: CIT (hours): G1, 6.07±0.11; G2, 5.91 ±0.22; G3, 5.98±0.27; G4, 6.13±0.21; G5, 6.06±0.07; G6, 5.88 ±0.15 (P=0.148, one-way ANOVA). Sew-in time (minutes): G1, 12.51±0.74; G2, 13.48±2.38; G3, 12.34± 0.84; G4, 12.72±0.88; G5, 12.81±1.10; G6, 12.26±1.50 (P=0.677, one-way ANOVA).
According to the assigned group, recipients were harvested four hours, two or five days after transplantation. Liver tissue samples were either immediately snap frozen and stored at -80 ℃ until measurements or formalin fixed for later pathological analysis. Blood samples were directly measured (AST, ALT, LDH and bilirubin) by an auto-analyzer at the central laboratory of the departments of laboratory medicine and pathobiochemistry, Charité Campus Virchow Klinikum, Berlin, Germany.
Histological analysis
Parts of retrieved liver grafts were fixed in 10% formalin, processed, and embedded in paraffin. The sections (4 μm thick) were stained with hematoxylin and eosin. The slides were then analyzed by a single pathologist blinded to the preparation of the sections. Histological severity of damage was graded according to a standardized semi-quantitative score (0-3) (0 for no damage, 3 for severe damage) regarding necrosis, apoptosis, "clearing nodules", bile duct proliferates, portal infiltrates and mitoses (maximum score available 18).
Zymography
After standard extraction procedures, proteins (20 μg/sample) in sodium dodecyl sulphate (SDS)-loading buffer were electrophoresed on a Biorad MiniProtean II System® (Biorad, München, Germany) through 10% SDS-polyacrylamid gels containing 0.03% gelatin (Ready Gel Zymogram Gels®, Biorad, München, Germany). A cell medium of human fibrosarcoma cells (HT 1080) containing large amounts of MMP2 and pro-MMP9 was used as an internal positive control.[12,13]After incubation in a development buffer (pH 7.4 and solved in 1 L aqua dest: 6.05 g Tris; 8.766 NaCl; 1.47 g CaCl2; 20 mL Brij 35 solution 1%) for 72 hours, gels were stained with Coomassie brilliant Blue® (Merck, Darmstadt, Germany), and destained with methanol/acetic acid/water(20:10:70).
Relative quantities of MMP activity were determined using a densitometer (GS 800 calibrated densitometer®, Biorad Laboratories, UK) and special software (Quantity one®, Biorad, UK). Optic density was determined in arbitrary units and in this form used as parametric data for statistical analysis.
Statistical analysis
Data are expressed as mean±SD or median and range, respectively. Statistical significance of differences was determined using Student'sttest for parametric data, and the Mann-WhitneyUtest and Wilcoxon's rank-sum test were used for non-parametric data (histology). APvalue of <0.05 was considered statistically significant. Prospective power analysis (forttest andP<0.05 considered significant) with an expected 10% difference of means between treatment and control groups and an expected SD of 5% for a desired power of at least 0.8 revealed a study population of six animals per group. For data processing and display Sigma Plot 2004 for Windows version 9.01 (Systat Software, Inc., Chicago, IL, USA) was used.
Results
Liver damage parameters
AST levels showed a trend towards lower values in pretreatment groups (G1, G3, G5) vs control groups (G2, G4, G6) at all time points after transplantation (P>0.05, Table 1). For ALT levels the same trend and significantly lower values four hours after transplantation were found (G1 vs G2,P<0.05; Table 1). LDH levels in recipients receiving pretreated livers were significantly lower at four hours after transplantation (P<0.05). Two and five days after transplantation no significant differences werefound (P>0.05, Table 1).
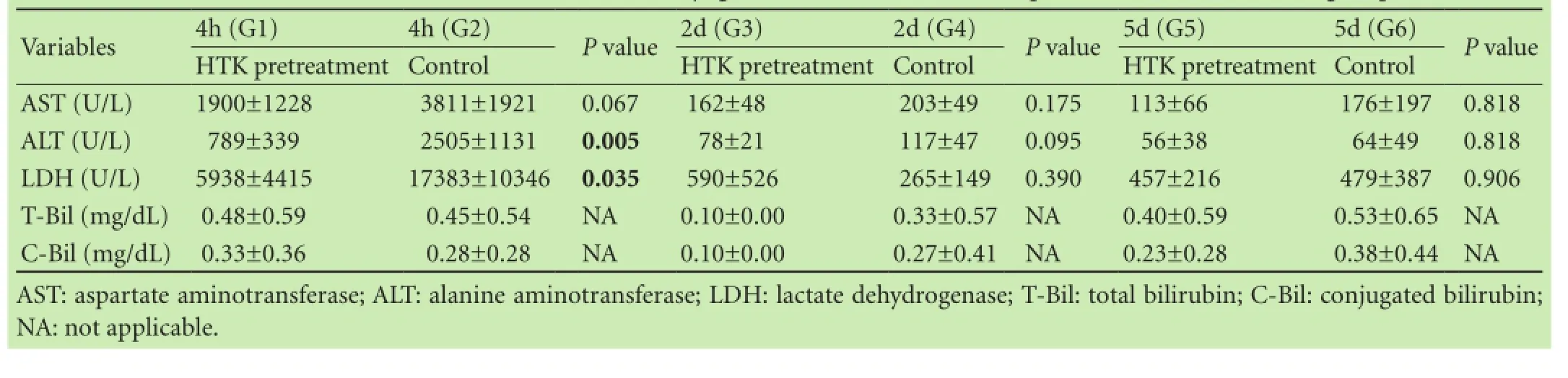
Table 1. Levels of AST, ALT, LDH, total and conjugated bilirubin in the HTK pretreatment and control groups
In general, all groups showed only minor histological damage. Highest scores were found in the control groups G4 (2; 0-4) and G6 (2; 0-7) at 2 and 5 days after transplantation, respectively. All scores are displayed in Fig. 1. Examples of animals from G2 and G6 are displayed in Fig. 2.
Levels of total and conjugated bilirubin are shown in Table 1. No pathological values or significant differences were found, data were in part not normally distributed, but since no pathological values were detected no statistical testing was performed.
MMP activity
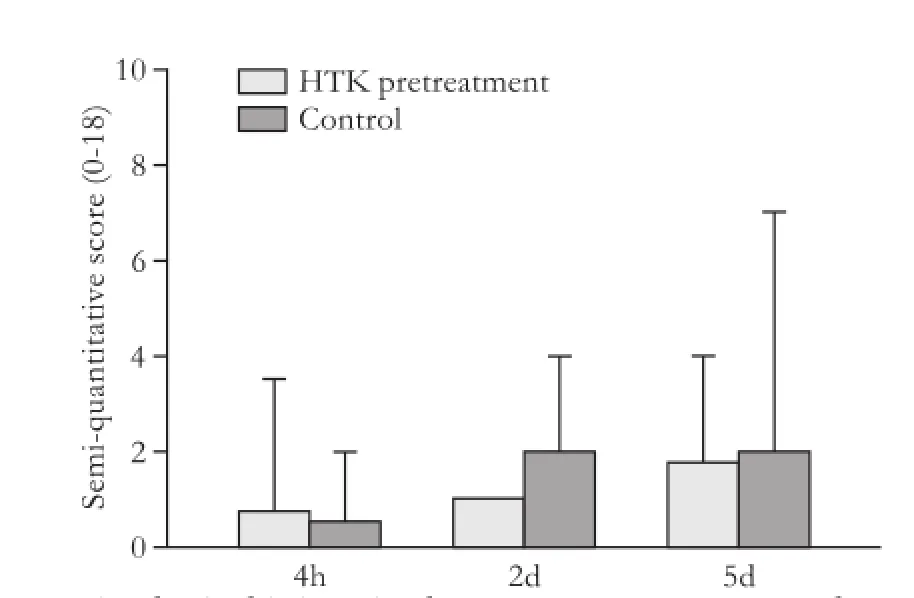
Fig. 1. Histological injury in the pretreatment vs control groups.
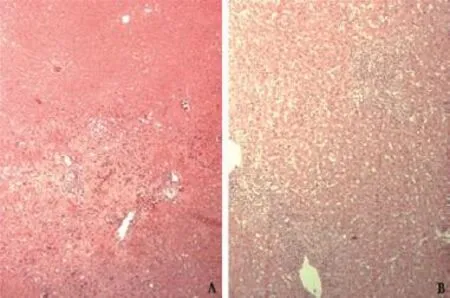
Fig. 2. Examples of tissue injury. A: G2; B: G6.
Zymography-gels showed three analyzable bands at 92 kDa, 72 kDa and 68 kDa, respectively. By use of internal controls and a standardized molecular marker, these bands were identified as regions of gelatolytic activity of pro-MMP9, pro-MMP2 and MMP2.
Differences of MMP activity between pretreatment and control groups
Four hours after transplantation, no difference between pro-MMP2 activities in the pretreatment and control groups could be found (P>0.05). Two and five days after transplantation, pro-MMP2 activity was significantly reduced in pretreated livers (P<0.05, Table 2).
Concerning MMP2 at four hours and five days, a tendency towards lower MMP2 activity in pretreated livers was found (P>0.05). Two days after transplantation, MMP2 activity was significantly reduced in pretreated livers (P<0.05, Table 2).
Four hours after transplantation, the activity of pro-MMP9 was significantly lower in the pretreated group G1 vs control G2 (P<0.05). After two days, pretreatment revealed significantly lower pro-MMP9 activity (G3 vs G4,P<0.05). Five days after transplantation, a trend towards lower pro-MMP9 activity could be detected for pretreated livers (Table 2).
Changes of MMP activity over time
Concerning pro-MMP2 in the control groups, a steady rise over time was found. Comparing 4 hours (G2) to 2 days (G4) showed significant difference (P=0.039), whereas comparing 4 hours vs 5 days (G2 vs G6) and 2 days vs 5 days (G4 vs G6) showed no significant difference. Interestingly, in the treatment groups, this rise was suppressed and no significant changes over time could be found between 4 hours (G1), 2 days (G3) and 5 days (G5) (Table 2).
Analysis of MMP2 changes over time revealed a similar picture, although the rise in the control groups was not statistical significant: 4 hours (G2) vs 2 days (G4); 4 hours (G2) vs 5 days (G6) and 2 days (G4) vs 5 days (G6). In the treatment groups, no increase in MMP2 activity was found over time (Table 2).
Pro-MMP9 of the control groups rose slightly from 4 hours (G2) to 2 days (G4) (P>0.05) and then dropped at 5 days (G6); 4 hours (G2) vs 5 days (G6) and 2 days (G4) vs 5 days (G6) (P>0.05). In the treatment groups, pro-MMP9 stayed at a lower level at 4 hours (G1) and 2 days (G3); and it rose slightly but not significantly at 5 days (Table 2).
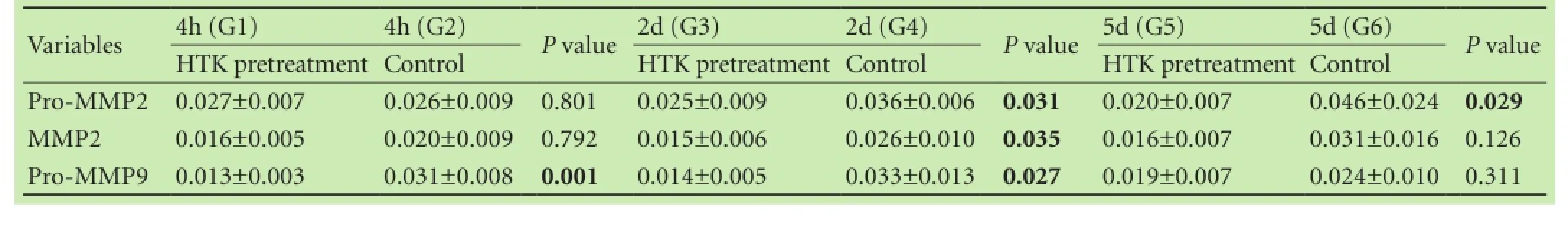
Table 2. Levels of pro-MMP2, MMP2 and pro-MMP9 in the HTK pretreatment and control groups
Discussion
The concept of improved liver preservation by warm (21 ℃) HTK donor pretreatment followed by cold HTK (4 ℃) perfusion and storage was proved to be feasible and easy to perform. No obvious side-effects or loss of donor animals during pretreatment could be detected. The improved preservation compared to controls was reflected in attenuated IRI, as measured by significantly lower enzyme levels post transplantation. This was accompanied by significantly lower activities of pro-MMP2 at two and five days as well as of pro-MMP9 at four hours and MMP2 and pro-MMP9 at two days. The measurement of reduced tissue activity of MMPs gives a mechanistic explanation on a molecular level that the reduced injury is caused, among others, by MMP inhibition. The reduced IRI is not reflected in significant differences of the histological score. Given the experimental design with a short CIT and healthy donors, this is not surprising.
HTK was originally introduced as a cardioplegic solution for protection in hypothermic conditions (23-32 ℃) and only later adapted to cold (4 ℃) preservation of organs.[14]On the basis of an extracellular fluid composition, HTK solely utilizes the intrinsic components histidine, tryptophan, and ketoglutarate. Cold conditions are essential for preserving organs in order to reduce metabolism and delay injury caused by hypoxia and shortage of substrates during storage. However, the cold condition causes injury, even by using the "ideal" preservation solution. This is proportional to storage time and a consequence of coldness itself.[15]Exposing cultivated hepatocytes and endothelial cells to cold conditions results in apoptosis caused by liberation of reactive oxygen species (ROS).[4]Decelerating metabolism not only reduces hypoxia induced injury, but also results in a lower substrate uptake into cells and hypothermic cell swelling due to reduced function of the Na+/K+-ATPase. During cooling, metabolic rate is suppressed about 12 to 13-fold when temperature is reduced from 37 ℃ to 0 ℃; however anaerobic metabolism remains, causing ATP depletion, lactate accumulation and subsequent acidotic intracellular condition.[16]To overcome some of these drawbacks of cold conditions, we applied a dose of (21 ℃) HTK systemically (by intravenous injection) fifteen minutes before cold flushing, whereas normal circulation and liver perfusion are still present, in order to enrich the donor livers with HTK whilst metabolism and transporters are still active. Since HTK is a mostly intracellular working preservation solution, it seems logical to apply at least parts of it during conditions that enable an improved uptake of its ingredients.
To avoid injuries immanent to cold conditions, experimental data on "subnormotherm" machine perfusion recommended temperatures of approximately 20 ℃; at this temperature much better preservation is achieved compared to lower (or higher) temperatures.[17-20]These authors assume improved energy supply in subnormotherm conditions compared to cold (4 ℃) conditions, which seems to be plausible due to higher remaining activity levels of enzymes and transporters within this temperature range. Meaning, the intrinsic ingredients of the preservation solution are transported inside the cell where they can develop their full effectiveness. Although measurements of the exact composition of the preserved livers were not performed in the present study, one plausible explanation for the reduced IRI in the treatment groups is a better accumulation of HTK in the donor livers.
MMPs, especially the gelatinases (MMP2 and MMP9), play a crucial role in liver IRI due to the complex series of events which lead to a profound rearrangement of the extracellular matrix. This allows cells to migrate into the wounded area and contribute to tissue remodelling and repair.[21]Upadhya et al[7]have clearly shown that a marked gelatinolytic activity corresponding to both MMP2 and MMP9 was observed in rat and human liver perfusates, implicating that these MMPs are released during cold preservation in a manner that is dependent on the time of cold storage. They also identified histidine (one essential component of HTK) as an intrinsic inhibitor of gelatinases.[6]In the same study, the group found HTK to be more effective in MMP inhibition compared to the University of Wisconsin (UW) solution and the inhibition was more effective during warm than cold conditions. To our knowledge, MMP-inhibitory features of HTK were up to now only demonstratedin vitro, and no transplant model was studied to enlighten the data presented by Upadhya and co-workers. Regarding the reduced activity of gelatinases in our pretreatment groups, we were able to enrich the donor liver with MMP-inhibitor histidine during the donor operation and provide evidence for its inhibitory function in experimental liver transplantation. We assume not only a more efficient histidine supply but also an equally effective enrichment with all other protective agents of HTK.
Reduced IRI after inhibition of MMPs was reported in several studies. Fondevila et al[22]demonstrated a reduced IRI accompanied by a profound inhibition of MMP9 expression in an experimental transplant model with steatotic rats after administration of a "cyclic-RGD-peptide". Interestingly, in this paper the protectivesubstance was administeredex vivovia the portal vein before cold storage and immediately prior to reperfusion. Whether an even more distinctive effect is achievable by administration during the donor operation under "warm" conditions would be interesting.
Soccal et al[23]showed a marked attenuation of IRI accompanied by significantly reduced pro-MMP2/ MMP2 and pro-MMP9/MMP9 activity after administration of an unselective MMP inhibitor (Batimastat) to donors (solved in preservation solution) and recipients (post transplantation) in experimental lung transplantation. They used eurocollins preservation solution that has a markedly lower MMP inhibitory action than HTK.[7]Nevertheless, the inhibition of MMP2 and MMP9 reduces IRI, supporting the second hypothesis of the presented study. One major advantage of our new concept is that no additional inhibitor has to be administered. Histidine is already part of HTK.
Ilmakunnas et al[24]described a marked elevation of serum MMP9 during reperfusion in human liver transplantation. They determined a relative lack of endogenous MMP inhibitors (tissue inhibitor of metalloproteinase, TIMPS) during reperfusion contributing to graft injury. Furthermore, they were able to show a correlation between postoperative bilirubin and ALT levels and the gradient of endogenous inhibitors: the less endogenous inhibitors the higher the levels of postoperative bilirubin and ALT. Our results suggested an opportunity for improvement at this point. Warm donor pretreatment resulted in an inhibition of pro-MMP2, MMP2 and pro-MMP9 and reduced liver injury (ALT and LDH levels). We could not determine influences on postoperative bilirubin levels, there were no differences between the pretreatment and control groups.
Another important question that has yet to be solved is the influence of warm HTK donor pretreatment on other possible transplantable organs of the donor. The used dosage of warm HTK did not obviously alter the donors' state during the grafting procedure; no donor animal was lost due to pretreatment.
For kidney availability we do not see a problem since HTK is an established standard preservation solution for kidney grafting. In addition, non-selective gelatinase inhibition with batimastat was not shown to be harmful (nor beneficial) in a renal warm IRI model.[25]Its benefit has yet to be tested for transplant conditions with cold ischemia. Concerning lung and heart transplantation, an inhibition of MMP activity and thus reduction of IRI has already been proved to be beneficial.[23,26]Whether HTK donor pretreatment is feasible in lung and heart transplant experiments has yet to be tested. For pancreas and small intestine transplants there are no respective data available.
In conclusion, our study demonstrates that the new concept of warm (21 ℃) HTK donor pretreatment improves the potency of HTK in the concept of liver preservation prior to transplantation. The finding is of further experimental and clinical relevance, as far as there is an increasing burden with extended criteria donors and the need to further improve the preservation concepts. If the results from this study can be confirmed in steatotic rats and/or after extended cold ischemia times as well as in a large-animal model, clinical trials are warranted. In comparison to other attempts to overcome the extended criteria donor problem, e.g. the most promising results of warm and hypothermic machine perfusion, warm HTK donor pretreatment is easy to use, low priced and could be easily performed during the time-consuming organ allocation.[27-30]Whereas machine perfusion is timeconsuming, expensive and requires special training, an additional room temperature infusion of approximately 800 mL HTK (for a 80 kg BW donor) accompanied by a simple potassium level testing during the allocation process could be easily implemented by any explant team worldwide.
Acknowledgements:We thank to Dr. Shafreena Kühn for improving the use of the English language in this manuscript and Mrs. Anja Schirmeier for her excellent help with Zymography.
Contributors:SW, NP and PG proposed the study. SW and AV performed the research. SW wrote the first draft. SW and OP analyzed the data. ST analyzed histology. AA and PJ revised the manuscript. PG supervised research. SW is the guarantor.
Funding:This study was supported by a grant of "Else-Kröner Fresenius Stiftung" (p49/07//A68/07).
Ethical approval:This study was approved by the local ethics committee.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Gastaca M. Extended criteria donors in liver transplantation: adapting donor quality and recipient. Transplant Proc 2009;41: 975-979.
2 Tector AJ, Mangus RS, Chestovich P, Vianna R, Fridell JA, Milgrom ML, et al. Use of extended criteria livers decreases wait time for liver transplantation without adversely impacting posttransplant survival. Ann Surg 2006;244:439-450.
3 Barshes NR, Horwitz IB, Franzini L, Vierling JM, Goss JA. Waitlist mortality decreases with increased use of extended criteria donor liver grafts at adult liver transplant centers. Am J Transplant 2007;7:1265-12670.
4 Rauen U, Polzar B, Stephan H, Mannherz HG, de Groot H. Cold-induced apoptosis in cultured hepatocytes and liver endothelial cells: mediation by reactive oxygen species. FASEB J1999;13:155-168.
5 Lee CY, Mangino MJ. Preservation methods for kidney and liver. Organogenesis 2009;5:105-112.
6 Upadhya GA, Strasberg SM. Glutathione, lactobionate, and histidine: cryptic inhibitors of matrix metalloproteinases contained in University of Wisconsin and histidine/tryptophan/ketoglutarate liver preservation solutions. Hepatology 2000;31:1115-1122.
7 Upadhya AG, Harvey RP, Howard TK, Lowell JA, Shenoy S, Strasberg SM. Evidence of a role for matrix metalloproteinases in cold preservation injury of the liver in humans and in the rat. Hepatology 1997;26:922-928.
8 Duarte S, Shen XD, Fondevila C, Busuttil RW, Coito AJ. Fibronectin-α4β1 interactions in hepatic cold ischemia and reperfusion injury: regulation of MMP-9 and MT1-MMP via the p38 MAPK pathway. Am J Transplant 2012;12:2689-2699.
9 Ariyakhagorn V, Schmitz V, Olschewski P, Polenz D, Boas-Knoop S, Neumann U, et al. Improvement of microsurgical techniques in orthotopic rat liver transplantation. J Surg Res 2009;153:332-339.
10 Cursio R, Mari B, Louis K, Rostagno P, Saint-Paul MC, Giudicelli J, et al. Rat liver injury after normothermic ischemia is prevented by a phosphinic matrix metalloproteinase inhibitor. FASEB J 2002;16:93-95.
11 National Research Council (US) Institute for Laboratory Animal Research, ed. Guide for the Care and Use of Laboratory Animals. Washington (DC): National Academies Press (US); 1996.
12 Morodomi T, Ogata Y, Sasaguri Y, Morimatsu M, Nagase H. Purification and characterization of matrix metalloproteinase 9 from U937 monocytic leukaemia and HT1080 fibrosarcoma cells. Biochem J 1992;285:603-611.
13 von Bredow DC, Cress AE, Howard EW, Bowden GT, Nagle RB. Activation of gelatinase-tissue-inhibitors-of-metalloproteinase complexes by matrilysin. Biochem J 1998;331:965-972.
14 Bretschneider HJ. Myocardial protection. Thorac Cardiovasc Surg 1980;28:295-302.
15 Vogel T, Brockmann JG, Friend PJ. Ex-vivo normothermic liver perfusion: an update. Curr Opin Organ Transplant 2010;15: 167-172.
16 Clavien PA, Harvey PR, Strasberg SM. Preservation and reperfusion injuries in liver allografts. An overview and synthesis of current studies. Transplantation 1992;53:957-978.
17 Bessems M, Doorschodt BM, Kolkert JL, Vetelainen RL, van Vliet AK, Vreeling H, et al. Preservation of steatotic livers: a comparison between cold storage and machine perfusion preservation. Liver Transpl 2007;13:497-504.
18 Saad S, Minor T. Short-term resuscitation of predamaged donor livers by brief machine perfusion: the influence of temperature. Transplant Proc 2008;40:3321-3326.
19 Vairetti M, Ferrigno A, Carlucci F, Tabucchi A, Rizzo V, Boncompagni E, et al. Subnormothermic machine perfusion protects steatotic livers against preservation injury: a potential for donor pool increase? Liver Transpl 2009;15:20-29.
20 Olschewski P, Gass P, Ariyakhagorn V, Jasse K, Hunold G, Menzel M, et al. The influence of storage temperature during machine perfusion on preservation quality of marginal donor livers. Cryobiology 2010;60:337-343.
21 Viappiani S, Sariahmetoglu M, Schulz R. The role of matrix metalloproteinase inhibitors in ischemia-reperfusion injury in the liver. Curr Pharm Des 2006;12:2923-2934.
22 Fondevila C, Shen XD, Duarte S, Busuttil RW, Coito AJ. Cytoprotective effects of a cyclic RGD peptide in steatotic liver cold ischemia and reperfusion injury. Am J Transplant 2009;9:2240-2250.
23 Soccal PM, Gasche Y, Miniati DN, Hoyt G, Berry GJ, Doyle RL, et al. Matrix metalloproteinase inhibition decreases ischemiareperfusion injury after lung transplantation. Am J Transplant 2004;4:41-50.
24 Ilmakunnas M, Höckerstedt K, Mäkisalo H, Siitonen S, Repo H, Pesonen EJ. Endogenous protease inhibitor uptake within the graft during reperfusion in human liver transplantation. J Hepatobiliary Pancreat Sci 2010;17:158-165.
25 Ziswiler R, Daniel C, Franz E, Marti HP. Renal matrix metalloproteinase activity is unaffected by experimental ischemia-reperfusion injury and matrix metalloproteinase inhibition does not alter outcome of renal function. Exp Nephrol 2001;9:118-124.
26 Falk V, Soccal PM, Grünenfelder J, Hoyt G, Walther T, Robbins RC. Regulation of matrix metalloproteinases and effect of MMP-inhibition in heart transplant related reperfusion injury. Eur J Cardiothorac Surg 2002;22:53-58.
27 Brockmann J, Reddy S, Coussios C, Pigott D, Guirriero D, Hughes D, et al. Normothermic perfusion: a new paradigm for organ preservation. Ann Surg 2009;250:1-6.
28 Guarrera JV. Assist devices: machine preservation of extended criteria donors. Liver Transpl 2012;18:S31-33.
29 Guarrera JV, Henry SD, Chen SW, Brown T, Nachber E, Arrington B, et al. Hypothermic machine preservation attenuates ischemia/reperfusion markers after liver transplantation: preliminary results. J Surg Res 2011;167:e365-373.
30 Guarrera JV, Henry SD, Samstein B, Odeh-Ramadan R, Kinkhabwala M, Goldstein MJ, et al. Hypothermic machine preservation in human liver transplantation: the first clinical series. Am J Transplant 2010;10:372-381.
Received July 23, 2014
Accepted after revision June 8, 2015
Author Affiliations:Allgemein-, Visceral- & Transplantationschirurgie, Charité Campus Virchow Klinikum, Berlin 13353, Germany (Schoening W, Ariyakhagorn V, Olschewski P, Andreou A, Neuhaus P, Pratschke J and Puhl G); General and Vascular Surgery, Bumrungrad International Hospital, Bangkok 10110, Thailand (Ariyakhagorn V); Department of Pathology, University of Erlangen, Erlangen 91054, Germany (Schubert T)
Wenzel Schoening, MD, Allgemein-, Visceral-& Transplantationschirurgie, Charité Campus Virchow Klinikum, Augustenburger Platz 1, Berlin 13353, Germany (Tel: +49-176-62564204; Fax: +49-30-450-552900; Email: wenzel.schoening@web.de)
© 2015, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(15)60426-X
Published online September 28, 2015.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Gut microbiota and non-alcoholic fatty liver disease
- Risk factors of metabolic syndrome after liver transplantation
- Combined Hangzhou criteria with neutrophillymphocyte ratio is superior to other criteria in selecting liver transplantation candidates with HBV-related hepatocellular carcinoma
- Intrahepatic distant recurrence following complete radiofrequency ablation of small hepatocellular carcinoma: risk factors and early MRI evaluation
- Oncogenic role of microRNA-423-5p in hepatocellular carcinoma
- Ankaflavin ameliorates steatotic liver ischemiareperfusion injury in mice
