舒张性和收缩性心衰患者的临床表现差异分析
2015-12-21于彤彤刘双双王菁菁王传合韩苏孙志军
于彤彤,刘双双,王菁菁,王传合,韩苏,孙志军
舒张性和收缩性心衰患者的临床表现差异分析
于彤彤,刘双双,王菁菁,王传合,韩苏,孙志军△
目的比较舒张性心功能衰竭(心衰)和收缩性心衰患者在临床表现及危险因素方面的差异。方法将2 088例心衰患者按左室射血分数(EF)分为舒张性心衰组(EF≥0.45,1 356例)和收缩性心衰组(EF<0.45,732例),比较2组的临床资料,分析影响2种心衰类型的相关因素。结果与收缩性心衰组相比,舒张性心衰组的平均年龄更大,女性及高血压的比例更高,但低蛋白血症、贫血、肾功能不全、高尿酸血症的比例更低,且以心功能Ⅰ、Ⅱ级为主;收缩压、白蛋白、前白蛋白、胆固醇、血钠、血氯水平更高,但心率更慢,肌酐、血尿酸、血钾、脑钠肽水平更低。与收缩性心衰组相比,舒张性心衰组的左室舒末容积、左室缩末容积较低,RAS阻断剂和β受体阻断剂使用率更低,他汀类药物使用率更高。Logistic多因素回归分析发现,性别、高血压对舒张性心衰影响更强;低蛋白血症、高尿酸血症则对收缩性心衰影响更强。结论舒张性心衰和收缩性心衰存在诸多差异,不同类型的心衰需采取不同的诊治及预防方案。
心力衰竭,舒张性;心力衰竭,收缩性;临床特点;危险因素
随着人口老龄化的到来,心衰的发病率逐渐升高并造成了沉重的社会负担。舒张性心功能衰竭(心衰)[又称左室射血分数(EF)保留的心衰,HFPEF]约占心衰总数的50%,其EF基本正常,同时存在舒张功能不全[1],虽然具有和收缩性心衰(又称EF降低的心衰,HF-REF)相似的症状和体征,但两者在临床特征、发病机制、诊疗措施等方面存在显著差异。本研究通过比较HF-PEF和HF-REF患者在病因、临床表现及危险因素方面的差异,为临床采取更加针对性的防治措施提供依据。
1 对象与方法
1.1 研究对象选取2005年11月—2012年1月就诊于我院的心衰患者2 088例,其中HF-PEF组1 356例(EF≥0.45),HF-REF组732例(EF<0.45);平均年龄(67±14)岁。纳入标准:(1)符合2014年中国心力衰竭诊断和治疗指南的诊断标准[2]。(2)入院时纽约心脏病协会(NYHA)心功能分级Ⅰ~Ⅳ级。(3)年龄>18岁。
1.2 方法以查阅病历的方式收集符合入选标准的慢性心衰患者的临床资料,包括人口统计学资料、既往疾病史、基础心血管病史、危险因素、体格检查、实验室指标、心脏超声检查、用药情况等。其中实验室指标均为入院次日清晨空腹取外周静脉血检测的结果;心脏超声数据取自入院3 d内首次测定的超声心动图。
高血压定义为收缩压≥140 mmHg(1 mmHg=0.133 kPa)和(或)舒张压≥90 mmHg(至少测量2次),或正在进行降压治疗。2型糖尿病定义为患者有糖尿病症状,且随机血糖≥11.1 mmol/L,或空腹血糖≥7.8 mmol/L,或口服糖耐量试验的餐后2 h血糖≥11.1 mmol/L(至少测量2次),或正在进行降糖治疗。血脂异常定义为总胆固醇(TC)>5.2 mmol/L,或低密度脂蛋白胆固醇(LDL-C)>3.4 mmol/L,或高密度脂蛋白胆固醇(HDL-C)<1.0 mmol/L,或血脂正常但正在服用调脂药物。高尿酸血症定义为血清中尿酸,男性超过416 μmol/L,女性超过357 μmol/L。贫血定义为血红蛋白,成年男性<130 g/L,成年女性<120 g/L,孕妇<110 g/L。低血清白蛋白定义为血清白蛋白<35 g/L。
1.3 统计学方法所有数据均采用SPSS19.0软件包进行统计学分析,正态分布计量资料以均数±标准差()表示,组间比较采用独立样本t检验;偏态分布计量资料组间比较采用Mann-Whitney U检验。计数资料以率或构成比表示,组间比较采用χ2检验。对单变量分析中有显著差异的指标,采用二元Logistic回归分析影响心衰类型的因素。以P<0.05(双侧)为差异有统计学意义。
2 结果
2.1 一般资料及合并症比较HF-PEF组年龄更大,女性及合并有高血压者更多,合并有低蛋白血症、贫血、肾功能不全及高尿酸血症者较少。HFREF组以心功能Ⅲ、Ⅳ级为主,HF-PEF组以心功能Ⅰ、Ⅱ、Ⅲ级为主。2组间糖尿病、缺血性心脏病、吸烟、高脂血症比例差异无统计学意义,见表1。

Tab.1Comparison of clinical characteristics and complications between two groups of patients表1 2组患者一般资料及合并症比较
2.2 生化指标及超声心动图检查结果比较见表2。与HF-REF组比较,HF-PEF组的收缩压、白蛋白、前白蛋白、TC、LDL-C、HDL-C、三酰甘油(TG)、血钠、血氯更高,肌酐(Cr)、血尿酸、血钾相对较低。超声心动图检查结果示,HF-PEF组的心率、左室舒末容积(EDV)、左室缩末容积(ESV)明显低于HF-REF组,但2组的每搏量(SV)差异无统计学意义。HFPEF组的脑钠肽(BNP)水平明显低于HF-REF组;HF-PEF组中BNP轻中度升高(BNP<250 ng/L及BNP 250~750 ng/L)的比例高于HF-REF组。2组间舒张压、血红蛋白、空腹血糖差异无统计学意义。
2.3 患者药物应用情况比较与HF-REF组相比,HFPEF组的肾素-血管紧张素系统(RAS)阻断剂和β受体阻断剂使用率较低,他汀类药物使用率较高,见表3。
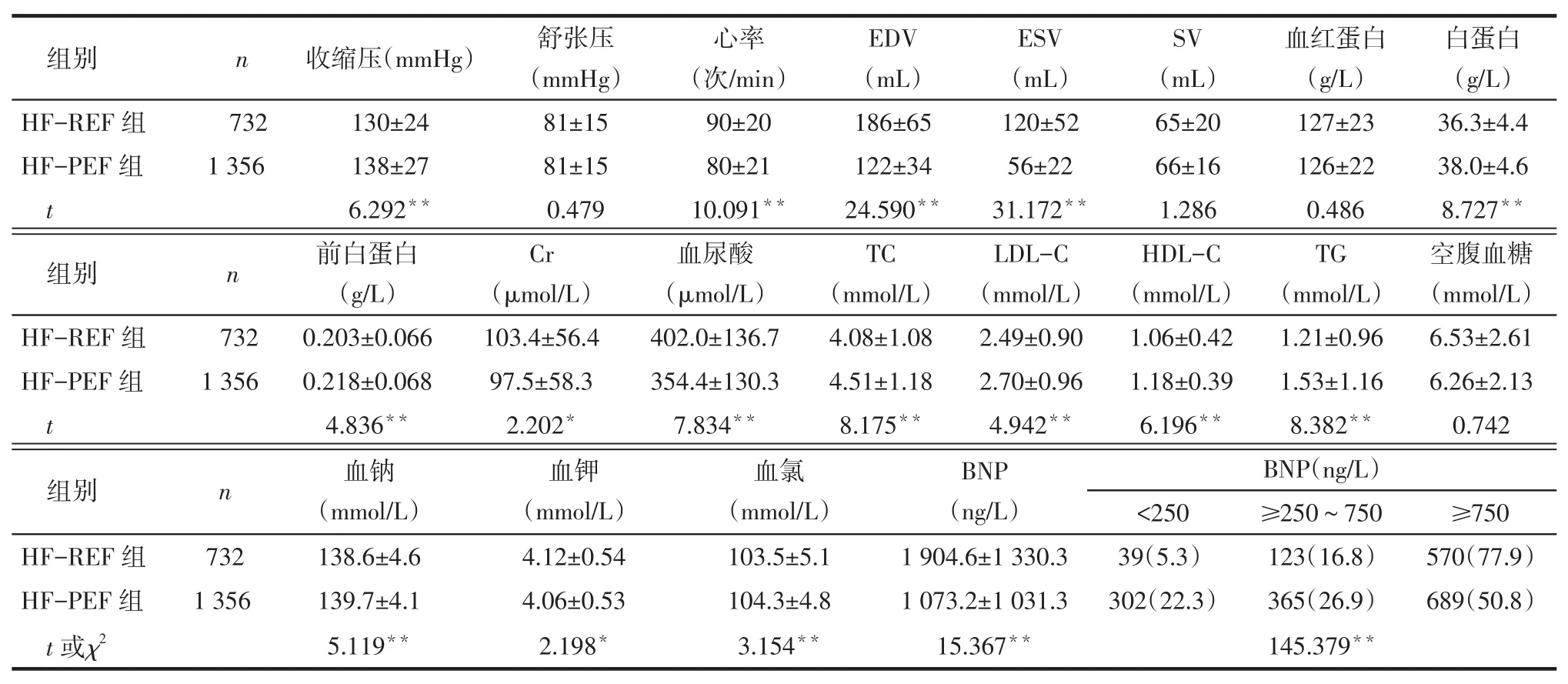
Tab.2Comparison of laboratory index and echocardiographic results on admission between two groups of patients表2 入院时2组患者生化指标及超声心动图检查结果比较

Tab.3 Comparison of medication on admission between two groups of patients表3 入院时2组患者药物应用情况比较例(%)
2.4 HF-PEF影响因素分析以心衰类型为因变量(HF-REF=0,HF-PEF=1),以年龄、性别(男=0,女= 1)、高血压病史、低蛋白血症、肾功能不全、贫血、高尿酸血症(赋值均为是=1,否=0)为自变量进行二元Logistic多因素回归分析,结果显示性别、高血压对HF-PEF组影响更强;低蛋白血症、高尿酸血症则对HF-REF组影响更强,见表4。

Tab.4Multivariate analysis of precipitating factors in HF-PEF patients with chronic heart failure表4 HF-PEF影响因素的二元Logistic回归分析结果
3 讨论
国外研究发现,HF-PEF在所有心衰中的占比在40%~71%,平均54%[3]。本研究中,HF-PEF占64.9%(1 356/2 088),与既往国内研究类似[4],但高于国外研究[3]。这可能与本研究入选人群年龄偏大及选取的EF临界值较低有关。目前,判定HF-PEF的EF临界值标准不一,欧洲心衰调查以EF≥0.40为临界值,发现HF-PEF占46.3%,平均年龄71岁[5];ADHERE研究发现,若以EF≥0.40为临界值,HFPEF占50.4%,若以EF≥0.55为临界值,HF-PEF占22.7%[6];OPTIMIZE-HF研究发现,若以EF≥0.40为临界值,HF-PEF占51.2%[7]。本研究参照2014年中国心力衰竭诊断和治疗指南的诊断标准,将HFPEF的EF临界值设定为0.45,发现HF-PEF在因心衰住院的患者中非常普遍,占64.9%。HF-PEF的EF临界值设定的过高或过低均存在问题,究竟应该设为多少还需要更进一步的研究。观察EF值处于临界区(0.50~0.54)人群的自然演变过程也许有助于研究者寻找到一个理想的临界值。
本研究表明,HF-PEF患者的平均年龄高于HF-REF患者,与之前的研究结果相同[6-7]。主要原因是随着年龄的增加,心肌僵硬化增加,即使不存在高血压,左心室心肌肥厚的发生率也可能大大增加[4],并进一步引起心室重构[8],造成心脏舒张性心功能不全。HF-PEF组高血压的比例高于HF-REF组,且高血压是HF-PEF的影响因素,与之前的研究结果相同[6]。HF-PEF组女性的比例要高于HF-REF组;且性别是HF-PEF的影响因素。有研究表明,女性心衰以舒张性心衰更多见[9]。在心导管检查中发现,女性心衰患者伴发舒张性心功能不全的比例较高,虽然左室舒张末期压力相似,但是女性的左室舒张末期容积要小于男性[10]。
既往研究发现,HF-PEF组的贫血患病率≥HFREF组[9,11],而本研究表明,HF-PEF组的贫血患病率低于HF-REF组,但2组间血红蛋白差异无统计学意义,与既往研究相反[12]。本研究表明HF-PEF组的肾功能不全比例低于HF-REF组,肌酐值也偏低,但回归分析未发现其是HF-PEF的影响因素。
与HF-REF组相比,HF-PEF组的RAS阻断剂和β受体阻断剂使用率更低,与既往研究相符[13]。但HF-PEF组他汀的使用率高于HF-REF组,可能与本研究入选的HF-PEF患者中缺血性心脏病比例较高有关。RAS阻断剂和β受体阻断剂的低使用反映出目前对HF-PEF的治疗尚缺乏有循证基础的有效措施。
由于左室射血分数基本正常,过去曾认为HFPEF的预后要好于HF-REF,对HF-PEF的治疗关注也不足,但目前研究发现HF-PEF的预后与HFREF相仿,全因死亡率也并不低[14]。HF-PEF的临床研究均未能证实对HF-REF有效的药物如血管紧张素转换酶抑制剂(ACEI)、血管紧张素受体拮抗剂(ARB)、β受体阻滞剂等可明显改善HF-PEF患者的预后和降低病死率[15]。因此,HF-PEF的治疗目前仍以经验性治疗为主,现在无统一的有循证基础的规范化治疗。
[1]Lam CS,Donal E,Kraigher-Krainer E,et al.Epidemiology and clinical course of heart failure with preserved ejection fraction[J].Eur J Heart Fail,2011,13(1):18-28.
[2]Chinese society of Cardiology,Editorial board of Chinese Journal of Cardiology.Chinese guidelines for the diagnosis and treatment of heart failure 2014[J].China J Cardio,2014,42(2):98-122.[中华医学会心血管病学分会,中华心血管病杂志编辑委员会.中国心力衰竭诊断和治疗指南2014[J].中华心血管病杂志,2014, 42(2):98-122].
[3]Owan TE,Redfield MM.Epidemiology of diastolic heart failure[J]. Prog Cardiovasc Dis,2005,47(5):320-332.
[4]Gabriel Y,Pearl H,Kam W,et al.Comparison of Frequencies of Left Ventricular Systolic and Diastolic Heart Failure in Chinese Living in Hong Kong[J].Am J Cardiol,1999,84(5):563-567.
[5]Lenzen MJ,Scholte op Reimer WJ,Boersma E,et al.Differences between patients with a preserved and a depressed left ventricular function:a report from the Euro Heart Failure Survey[J].Eur Heart J,2004,25(14):1214-1220.
[6]Yancy CW,Lopatin M,Stevenson LW,et al.Clinical presentation, management,and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: A report from the Acute Decompensated Heart Failure National Registry(ADHERE)Database[J].J Am Coll Cardiol,2006,47(1): 76-84.
[7]Fonarow GC,Stough WG,Abraham WT,et al.Characteristics,treatments,and outcomes of patients with preserved systolic function hospitalized for heart failure:A report from the-OPTIMIZE-HF Registry[J].J Am Coll Cardiol,2007,50(8):768-777.
[8]Wei JY.Age and the cardiovascular system[J].N Engl J Med, 1992,327(24):1735-1739.
[9]Bhatia RS,Tu JV,Lee DS,et al.Outcome of heart failure with preserved ejection fraction in a population-based study[J].N Engl J Med,2006,355(3):260-269.
[10]Mendes LA,Davidoff R,Cupples LA,et al.Congestive heart failure in patients with coronary artery disease:the gender paradox[J].Am Heart J,1997,134(2 Pt 1):207-212.
[11]O’Meara E,Clayton T,McEntegart MB,et al.Clinical correlates and consequences of anemia in a broad spectrum of patients with heart failure:Results of the Candesartan in Heart Failure:Assessment of Reduction in Mortality and Morbidity(CHARM)Program [J].Circulation,2006,113(7):986-994.
[12]Tsuchihashi-Makaya M,Hamaguchi S,Kinugawa S,et al.Characteristics and Outcomes of Hospitalized Patients With Heart Failure and Reduced vs Preserved Ejection Fraction:A Report From the Japanese Cardiac Registry of Heart Failure in Cardiology(JCARECARD)[J].Circ J,2009,73(10):1893-1900.
[13]Tsutsui H,Tsuchihashi M,Takeshita A.Mortality and readmission of hospitalized patients with congestive heart failure and preserved versus depressed systolic function[J].Am J Cardiol,2001,88(5): 530-533.
[14]Somaratne JB,Berry C,McMurray JJ,et al.The prognostic signifi cance of heart failure with preserved left ventricular ejection fraction:a literature-based meta-analysis[J].Eur J Heart Fail,2009, 11(9):855-862.
[15]Yamamoto K,Origasa H,Hori M.Effects of carvediol on heart failure with preserved ejection fraction:the Japanese diastolic heat failure study[J].Eur J Heart Fail,2013,15(1):110-118.
(2014-07-25收稿2014-09-10修回)
(本文编辑闫娟)
Differences in clinical characteristics between patients with diastolic heart failure and systolic heart failure
YU Tongtong,LIU Shuangshuang,WANG Jingjing,WANG Chuanhe,HAN Su,SUN Zhijun△
Department of Cardiology,Shengjing Hospital of China Medical University,Shenyang 110004,China△
ObjectiveTo analyze the differences in clinical characteristics and risk factors in patients with diastolic heart failure and systolic heart failure.MethodsA total of 2 088 patients with heart failure were divided into two groups, diastolic heart failure group(EF≥0.45,n=1 356)and systolic heart failure group(EF<0.45,n=732),according to ejection fraction(EF).The clinical features and related factors affecting the two types of heart failure were compared between two groups.ResultsThere were higher age,higher proportion of women and higher proportion of hypertensive patients in diastolic heart failure group than those of systolic heart failure group,but lower rates of hypoalbuminemia,anemia,renal insufficiency and hyperuricimia.There was higher incidence of functional class I and II in diastolic heart failure group.And compared with systolic heart failure group,there were higher levels of systolic blood pressure,albumin,prealbumin,cholesterol, sodium and serum chloride in diastolic heart failure group,but lower levels of heart rates,creatinine,blood uric acid,potassium and brain natriuretic peptide.Compared with systolic heart failure group,there were lower left ventricular end diastolic volume(LVEDV)and left ventricular end systolic volume(LVESV)in diastolic heart failure group.And there were lowerRAS blocker and β-blocker usage,higher statin usage in diastolic heart failure group.Logistic regression analysis showed that gender and hypertension were significantly correlated with diastolic heart failure,and hypoalbuminemia and hyperuricimia were significantly correlated with systolic heart failure.ConclusionOur results show that there are differences in clinical features and risk factors in patients with diastolic heart failure and systolic heart failure.We should take the different treatment and prevention programs for the two kinds of heart failures.
heart failure,diastolic;heart failure,systolic;clinical characteristics;risk factors
R541.61
A
10.3969/j.issn.0253-9896.2015.01.018
中国医科大学附属盛京医院心内科,辽宁沈阳(邮编110004)
于彤彤(1983),男,讲师,硕士,主要从事心血管病研究
△通讯作者E-mail:sunzj_99@163.com