成人烟雾病患者不同分期脑内缺血性病变MRI特点
2015-09-29乔鹏岗韩聪左智炜王一托邢旭东钱天翼李功杰
乔鹏岗,韩聪,左智炜,王一托,邢旭东,钱天翼,李功杰*
成人烟雾病患者不同分期脑内缺血性病变MRI特点
乔鹏岗1,韩聪2,左智炜1,王一托1,邢旭东1,钱天翼3,李功杰1*
目的 分析不同分期烟雾病患者脑内缺血性病变磁共振成像(magnetic resonance imaging,MRI)特点及可能的发病机制。材料与方法 回顾性分析94例成人烟雾病患者174侧受累大脑半球脑内缺血病灶分布特点,进行脑血管意外(cerebrovascular accident,CVA)评分,并比较其与数字减影血管造影(digital subtraction angiography,DSA)分期的相关性。结果 174侧受累大脑半球Ⅰ期6侧,Ⅱ期 26侧,Ⅲ期 23侧,Ⅳ期50侧,Ⅴ期49侧,Ⅵ期 20侧;其中156侧大脑半球出现缺血病灶,114侧大脑半球缺血病灶仅累及皮层下组织,42侧大脑半球缺血病灶累及皮层,145侧大脑半球缺血灶仅累及前循环,11侧大脑半球缺血病灶累及后循环;174侧受累大脑半球CVA评分0分18侧,1分74侧,2分40侧,3分42侧。随着血管造影分期的进展,脑内缺血病灶由皮层下区域逐渐累及皮层(r=0.32859,P<0.0001),且缺血病灶CVA评分逐渐增加(r=0.30375,P <0.0001)。结论 成人烟雾病患者脑内缺血病灶的分布模式和病灶大小随着病情进展有一定的变化规律,了解该特点对烟雾病的早期诊断及病情评估有一定的临床价值。
烟雾病;脑缺血;磁共振成像;血流动力学;脑血管意外;血管造影术,数字减影;成人
1Department of Radiology, Affiliated Hospital of Academy of Military Medical Sciences, Beijing 100071, China
2Department of Neurosurgery, Affiliated Hospital of Academy of Military Medical Sciences, Beijing 100071, China
3Siemens Healthcare, MR Neuro Applications, Erlangen, Germany, Shenzhen 518057, China
*Correspondence to: Li GJ, E-mail: ligj307@163.com
烟雾病(moyamoya disease,MMD)是一种原因不明的慢性进行性脑血管闭塞性疾病,以颈内动脉末端及大脑前、大脑中动脉起始部内膜缓慢增厚、动脉管腔逐渐狭窄以至闭塞、脑底穿通动脉代偿性扩张为特征[1]。烟雾病在临床上主要表现为缺血性或出血型,并以缺血型为主[2]。与急性栓塞性脑卒中相比,烟雾病由于其侧枝循环的独特性及多态性,其脑内缺血性病灶会有不同的表现模式。本文回顾性分析成人烟雾病脑内缺血性病变磁共振成像(magnetic resonance imaging,MRI)特点,并与数字减影血管造影(digital subtraction angiography,DSA)分期进行比较,分析不同分期烟雾病患者脑内缺血性病灶的分布模式及其可能的发病机制。
1 材料与方法
1.1病例选择
回顾性分析2015年1月至2015年6月在我院确诊的成人烟雾病患者94例,其中男性46例,女性48例,年龄21~64岁,平均(40.4±9.1)岁;双侧脑血管受累80例,单侧脑血管受累14例。所有病例均经DSA确诊,并接受MRI检查,MRI检查与DSA检查间隔不超过一周。
1.2MRI扫描方法
采用西门子公司生产的M A G N E T O M Skyra 3.0 T磁共振扫描仪。扫描序列及参数:横轴位T1WI(TR/TE:1600 ms/8.5 ms,矩阵:320×320)、横轴位T2WI(TR/TE:6000 ms/ 99 ms,矩阵256×256)、冠状位T2WI-水抑制(TR/ TE:9000 ms/85 ms,矩阵256×256)、横轴位高分辨DWI(TR:4200 ms,TE:64 ms/103 ms,矩阵164×164,b=0/1000 s/mm2),所有序列FOV 220 mm,层厚5 mm,采集次数1。
1.3脑内缺血性病灶评价
由两名放射科高级职称医师对所有患者常规MRI图像进行分析,判定174侧受累大脑半球脑缺血病灶的位置,并按有无皮层受累分为无病灶、病灶仅累及皮层下组织、病灶累及皮层;按有无后循环供血区受累分为无病灶、前循环供血区受累、后循环供血区受累。同时,将脑内病灶进行CVA评分,具体标准[3]为:以T2WI水抑制像结果进行判断,无病灶为0分,小病灶(最大长径<10 mm)为1分,中等大小病灶(10 mm≤最大长径≤30 mm)为2分,大病灶(最大长径>30 mm)为3分。
1.4烟雾病DSA分期
1名高年资神经外科主治医师对所有患者受累侧大脑半球DSA图像进行铃木分期[1],标准如下,Ⅰ期:颈内动脉末端分叉狭窄,无其它异常所见;Ⅱ期:颈内动脉(internal carotid artery,ICA)末端分叉狭窄,颅底烟雾状血管形成;Ⅲ期:大脑前动脉(anterior cerebral artery,ACA)和大脑中动脉(middle cerebral artery,MCA)有缺失,烟雾状血管非常明显;Ⅳ期:烟雾状血管衰减;Ⅴ期:从颈内动脉发出的主要动脉完全消失,烟雾状血管明显减少;Ⅵ期:颈内动脉虹吸段完全消失,烟雾状血管完全消失,仅见从颅外到颅内的侧枝循环。
1.5统计分析
采用Spearman相关分析比较烟雾病脑内缺血病灶的位置、CVA评分与DSA分间的相关性,统计软件采用SAS 9.3。P<0.05具有统计学意义。
2 结果
2.1DSA分期
174侧受累大脑半球Ⅰ期 6侧,Ⅱ期 26侧,Ⅲ期 23侧,Ⅳ期50侧,Ⅴ期49侧,Ⅵ期 20侧。
2.2缺血病灶评价
174侧受累大脑半球156侧大脑半球出现缺血病灶,其中114侧大脑半球缺血病灶仅累及皮层下组织,42侧大脑半球缺血病灶累及皮层;156侧缺血半球中145侧大脑半球缺血灶仅累及前循环,11侧大脑半球缺血病灶累及后循环;174侧受累大脑半球CVA评分0分18侧,1分74侧,2分40侧,3分42侧。缺血病灶位置、CVA评分与DSA分期比较见图1、表1。
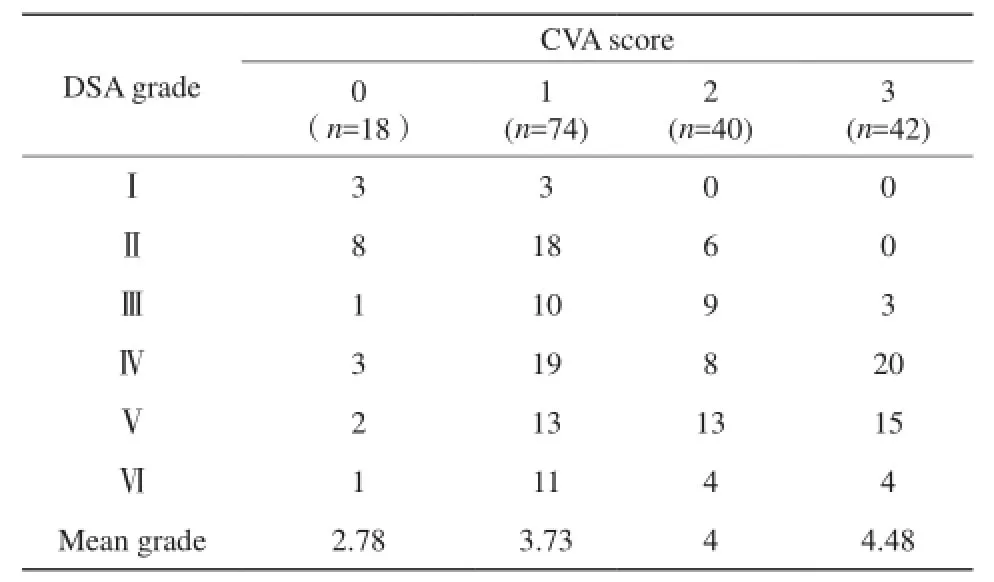
表1 烟雾病患者脑内缺血病灶评分与DSA分期比较Table 1 Comparison of CVA score and DSA grade in MMD patients
2.3统计结果
结果表明,随着烟雾病脑血管DSA分期的进展,脑内缺血病灶由皮层下区域逐渐累及皮层(r=0.32859,P=0.0179,图2),且缺血病灶CVA评分逐渐增加(r=0.30375,P<0.0001)。虽然脑内缺血病灶由前循环累及后循环的趋势无统计学差异(P=0.4769),但累及后循环的11侧大脑半球DSA分期均在Ⅳ期以上。
3 讨论
烟雾病是一组原因不明的慢性进行性脑血管闭塞性疾病,临床表现为缺血型或出血型,既往认为儿童以缺血为主而成人以出血为主。随着无创性诊断技术包括MRI、经颅超声多普勒的广泛应用,越来越多的症状较轻或无症状的烟雾病得到诊断,使缺血型烟雾病,尤其是成年人缺血型烟雾病的发病比例增加。目前,MRI已成为诊断脑缺血性病变的常用而且有效的检查手段[4-5]。烟雾病独特的侧枝循环模式使其脑内缺血病灶有不同的MRI表现特点,不同分期烟雾病患者也会有不同的MRI表现[6],了解该特点对疾病的早期诊断可能会有重要价值。
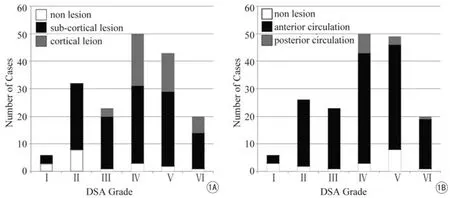
图1 烟雾病患者脑内缺血病灶位置与DSA分期比较。A:随着DSA分期的进展,烟雾病患者脑内缺血病灶皮层下区域逐渐累及皮层;B:显示当烟雾病DSA分期进展至Ⅳ期以上时,开始出现累及后循环的缺血灶Fig. 1 Comparison of location of the ischemic lesions and DSA grade in MMD patients. A: Shows that along with the increasing of stages diagnosed by DSA, the lesions growth from sub-cortical area to cortical area; B: Shows that the ischemic lesions involved posterior circulation areas after grade Ⅳ.
3.1烟雾病侧枝循环模式
在烟雾病进展过程中存在不同模式的侧枝循环[7]:(1)皮层软脑膜吻合:大脑后动脉(posterior cerebral artery,PCA)通过皮层软脑膜向MCA和ACA皮层供血,在MCA或ACA起始部受累时就可以出现;(2)PCA通过胼胝体背侧动脉供应ACA、通过脉络膜后动脉及其它穿支动脉供应MCA深部供血区,常常与皮层软脑膜吻合同时存在;(3)颅外到颅内代偿,包括眼动脉经眶动脉供应ACA额叶供血区、颈外动脉通过硬软脑膜吻合向颅内供血、脑膜中动脉供应MCA供血区,是晚期烟雾病患者重要的代偿通路。
3.2烟雾病患者脑内缺血病灶的变化特点
由于侧枝循环的多变性,烟雾病患者脑内缺血病灶的发生与急性栓塞性脑卒中引起的缺血型病变会有不同的特点,其脑卒中的模式表现为多态性[8-9]。急性栓塞性脑卒中由于栓塞部位的不同常表现为区域性脑梗死或分水岭区脑梗死,区域性脑梗死最为常见;而烟雾病患者脑内缺血性病灶最常发生在大脑前循环供血区皮层下区域即内侧分水岭区,随着病情进展逐渐累及皮层和大脑后循环供血区,且缺血病灶范围逐渐增大。这种变化与烟雾病独特的侧支循环模式有关。在烟雾病早期阶段,大脑前循环的大动脉发生狭窄,此时PCA会通过前述前两型侧枝循环同时向皮层和深部白质供血,脑供血比较充分,受累大脑半球可无缺血灶或仅出现小的点状缺血灶,缺血灶位置发生在皮层下内侧分水岭区;当病情进展烟雾状血管退化时,PCA向前循环的供血减少,此时大脑皮层还可由颅外向颅内的侧支循环代偿供血,而皮层下深部组织缺血病灶的范围会增大;当进展至疾病后期,侧枝循环进一步退化,大脑皮层缺血也会加重而发生梗死。另外一方面,当大脑后动脉受累或由于向前循环代偿过多而造成后循环供血不足时,后循环供血区发生缺血性卒中的风险也会增加[10-11]。

图2 A:Ⅰ期烟雾病患者,双额叶皮层下点状缺血灶,CVA评分1分;B:Ⅱ期烟雾病患者,左额叶皮层下缺血性梗死灶,CVA评分2分;C:Ⅲ期烟雾病患者,左顶叶皮层下缺血性梗死灶,CVA评分3分;D:Ⅳ期烟雾病患者,左额叶皮层缺血性梗死,CVA评分3分;E:Ⅴ期烟雾病患者,左枕叶皮层缺血性梗死,CVA评分3分;F:Ⅵ期烟雾病患者,左枕叶皮层缺血性梗死,CVA评分3分Fig. 2 A: A stage Ⅰ MMD patient with punctuate ischemic lesions in sub-cortical structure of bilateral front lobe, the CVA score was 1; B: A Stage Ⅱ MMD patient with ischemic infarction lesion in sub-cortical white matter of left front lobe, the CVA score was 2; C: A Stage Ⅲ MMD patient with ischemic infarction lesion in sub-cortical area of left parietal lobe, the CVA score was 3; D: A Stage Ⅳ MMD patient with ischemic infarction lesion in the cortex of left front lobe, the CVA score was 3; E: A Stage Ⅴ MMD patient with ischemic infarction lesions in occipital cortex, the CVA score was 3; F: A Stage Ⅵ MMD patient with ischemic infarction lesion in occipital cortex, the CVA score was 3.
3.3烟雾病脑内缺血病灶的发生机制
过去普遍认为,烟雾病患者缺血病变的发生是由于大血管的狭窄造成的严重的低灌注所致[12]。而在缺血性烟雾病疾病进展过程中,除了大血管的狭窄造成血流动力学的损害而引起缺血性卒中外,也会增加血管栓塞性卒中的风险[13-15]。Takagi Y等[16]发现狭窄的ICA、MCA管壁及扩张的烟雾血管内可见血栓,成分为血小板和纤维蛋白,为动脉栓子的来源。烟雾病脑梗死的发生部位以内侧分水岭区和大脑前循环供血区的皮层多见,也支持其发病机制中有动脉栓塞及低灌注/栓子清除障碍共同参与[9]。J-M Kim等[12]认为,当脑内缺血病灶发生部位与血流动力学损害部位不一致时,应考虑到血栓形成的可能并选择合理的治疗方案(如抗血栓治疗)。
另外,还应注意到,虽然随着烟雾病的病程进展脑内缺血病灶的范围会由皮层下区域和大脑前循环供血区逐渐累及皮层和大脑后循环供血区,但铃木分期Ⅳ期以上的患者仍有相当一部分患者缺血灶仅累及皮层下组织、CVA评分仅为1分甚至无脑实质的损害发生。可见,作为金标准的铃木分期在评估脑缺血状态时仍有不足之处,临床工作中还需结合多种检查共同评估患者病情。
综上所述,烟雾病脑内缺血性病灶由于其侧枝循环的独特性及多态性有一定的特点,病灶位置随着疾病进展而变化,最早发生在皮层下内侧分水岭区和大脑前循环供血区,逐渐累及皮层和大脑后循环供血区,了解该特点对烟雾病的早期诊断及病情评估有一定的临床价值。
[References]
[1] Suzuki J, Takaku A. Cerebrovasular “moyamoya” disease: diseaseshowing abnormal net-like vessels in bease of brain. Arch Neurol, 1969, 20(3): 288-299.
[2] Gao S, Ni J, Huang JX, et al. Clinical characteristics of moyamoya disease. Chin J Neurol, 2006, 39(3): 176-179.
高山, 倪俊, 黄家星, 等. 烟雾病临床特点分析. 中华神经科杂志, 2006, 39(3): 176-179.
[3] Hart RG. Immediate anticoagulation of embolic stroke: a randomized trial. Stroke, 1983, 14(5): 668-676.
[4] Bai M, Guo Q, Wu L, et al. The diagnostic value of 3.0 T MRI in detecting childhood arterial ischaemic stroke. Chin J Magn Reson Imaging, 2013, 4(3): 192-195.
白敏, 郭茜, 吴林, 等. 3.0 T MRI对儿童动脉性缺血性脑卒中的诊断价值. 磁共振成像, 2013, 4(3): 192-195.
[5] Li ML. Advance of cerebral magnetic resonance angiography at 3.0 T. Chin J Magn Reson Imaging, 2013, 4(4): 309-313.
李明利. 3.0 T MR脑血管成像的临床应用进展. 磁共振成像, 2013, 4(4): 309-313.
[6] Jung MY, Kim YO, Yoon W, et al. Characteristics of brain magnetic resonance images at symptom onset in children with moyamoya disease. Brain Dev, 2015, 37(3): 299-306.
[7] You SJ, Cao YJ, Zhang CY, et al. Analysis of clinical manifestations and angiographic stage and compensatory mechanisms in patients with moyamoya disease. Chin J Cerebrovasc Dis (Electronic Edition), 2011, 5(2): 89-95.
尤寿江, 曹勇军, 章春园, 等. 成人烟雾病的临床特点、分期及代偿机制分析. 中华脑血管病杂志(电子版), 2011, 5(2): 89-95.
[8] Liu W, Zhu S, Wang X, et al. Evaluation of angiographic changes of the anterior choroidal and posterior communicating arteries for predicting cerebrovascular lesions in adult moyamoya disease. J Clin Neurosci, 2011, 18(3): 374-378.
[9] Gao HH, Gao LB, Wen JM. The distribution patterns of cerebral infarction and the features of collateral circulation in adult patients with ischemic moyamoya disease. J Intervent Radiol, 2013, 22(8): 621-624.
高红华, 高连波, 文佳媚. 成年缺血性烟雾病脑梗死的分布模式及侧支循环特点. 介入放射学杂志, 2013, 22(8): 621-624.
[10] Mugikura S, Takahashi S, Higano S, et al. The relationship between cerebral infarction and angiographic characteristics in childhood moyamoya disease. Am J Neuroradiol, 1999, 20(2): 336-343.
[11] Yamada I, Himeno Y, Suzuki S, et al. Posterior circulation in moyamoya disease: angiographic study. Radiology, 1995, 197(1): 239-246.
[12] Kim JM, Lee SH, Roh JK. Changing ischaemic lesion patterns in adult moyamoya disease.J Neurol Neurosurg Psychiatry, 2009, 80(1): 36-40.
[13] Momjian-Mayor I, Baron JC. The pathophysiology of watershed infarction in internalcarotid artery disease: review of cerebral perfusion studies. Stroke, 2005, 36(3): 567-577.
[14] Horn P, Bueltmann E, Buch CV, et al. Arterio-embolic ischemic stroke in children with moyamoya disease. Childs Nerv Syst, 2005, 21(2): 104-107.
[15] Iguchi Y, Kimura K, Tateishi Y, et al. Microembolic signals are associated with progression of arterial lesion in Moyamoya disease: a case report. J Neurol Sci, 2007, 260(1-2): 253-255.
[16] Takagi Y, Kikuta K, Nozaki K, et al. Histological features of middle cerebral arteries from patients treated for Moyamoya disease. Neurol Med Chir(Tokyo), 2007, 47(1): 1-4.
The MRI features of ischemic lesions of adult moyamoya disease patients in different stage
QIAO Peng-gang1, HAN Cong2, ZUO Zhi-wei1, WANG Yi-tuo1, XING Xu-dong1, QIAN Tian-yi3, LI Gong-jie1*
14 Sep 2015, Accepted 22 Oct 2015
Objective: To analyze the MRI features of adult moyamoya patients in different stage and possible pathogenesis. Materials and Methods: We retrospectively reviewed the topography of ischemic lesions in 174 cerebral hemispheres of 94 adult patients with moyamoya disease, CVA score were calculated and its correlation with DSA findings were compared. Results: Using the results of DSA as reference, there were 6, 26, 23, 50, 49, 20 cerebral hemispheres in stages I to VI respectively among all 174 cerebral hemispheres. Ischemic lesions were detected in 156 hemispheres: 114 hemispheres only effect sub-cortical structure and 42 hemispheres has cortical areas been involved. There are 145 hemispheres that have lesions located in anterior circulation and 11 hemispheres has lesions in posterior circulation areas. The number of hemispheres whose CVA score is 0-3 are 18, 74, 40, 42 respectively. Along with the increase of stages diagnosed by DSA, the lesions growth from sub-cortical area to cortical area(r=0.32859, P<0.0001), while the CVA score increased as well(r=0.30375, P<0.0001). Conclusion: The location and size of ischemic lesions in patients with moyamoya disease changes along with the progress of DSA grade, which would behelpful to early diagnosis and condition evaluation.
Moyamoya disease; Brain ischemia; Magnetic resonance imaging; Hemodynamics; Cerebrovascular accident; Angiography, Digital subtraction; Adult
1.军事医学科学院附属医院放射科,北京 100071
2.军事医学科学院附属医院神经外科,北京 100071
3.西门子(中国)有限公司磁共振事业部,深圳 518057
李功杰,E-mail:ligj307@163.com
2015-09-14
R445.2;R725.4
A
10.3969/j.issn.1674-8034.2015.12.003乔鹏岗, 韩聪, 左智炜, 等. 成人烟雾病患者不同分期脑内缺血性病变MRI特点. 磁共振成像, 2015, 6(12): 893-897.
北京市自然科学基金青年项目(编号:7144231);首都临床特色应用研究项目(编号:Z141107002514171)
接受日期:2015-10-22
ACKNOWLEDGMENTS This work was part of youth project Beijing municipal natural science foundation (No. 7144231); Capital characteristic clinic project(No. Z141107002514171).