成人非酒精性脂肪肝与2型糖尿病发病关系的前瞻性队列研究
2015-09-24李卫东傅坤发连燕舒陈允菊夏金荣
李卫东,傅坤发,连燕舒,陈允菊,夏金荣
·论著·
成人非酒精性脂肪肝与2型糖尿病发病关系的前瞻性队列研究
李卫东,傅坤发,连燕舒,陈允菊,夏金荣
目的探讨成人非酒精性脂肪肝(NAFLD)与2型糖尿病(T2DM)发病的关系。方法以南京市三所医院(东南大学附属中大医院、江苏省老年医院、南京市职业病防治院)体检职工人群为前瞻性研究随访队列,2008年基线调查其一般资料、既往病史、吸烟、饮酒、身体活动情况及体检资料等,2009—2012年连续随访4年,以首次诊断为T2DM为观察终点。将资料完整并符合要求的2 464例体检职工纳入分析,其中男1 445例,女1 019例。根据基线B超检查和饮酒情况将体检职工分为NAFLD组(n=365例)和对照组(n=2 099例)。采用COX比例风险回归模型分析NAFLD与T2DM发病风险的关系。结果经过平均3.8年的随访(9 695人年,其中NAFLD组1 397人年,对照组8 298人年),共有32例发生T2DM,累积发病率为3.30/1 000人年。其中NAFLD组中有12例发生T2DM,累积发病率为8.59/1 000人年;对照组中有20例发生T2DM,累积发病率为2.41/1 000人年。Kaplan-Meier分析显示,两组累积发病率间差异有统计学意义(χ2=21.374,P<0.001)。调整年龄、性别、教育程度、家庭收入、吸烟、饮酒、糖尿病家族史、手术史、每日身体活动量、空腹血糖(FBG)、总胆固醇(TC)、丙氨酸氨基转移酶(ALT)、血尿酸(BUA)及体质指数(BMI)后,与对照组相比,NAFLD组发生T2DM的HR(95%CI)为2.936(1.380,6.247)。结论NAFLD会增加T2DM的发病风险,是T2DM的独立危险因素。为减少糖尿病发生,成年人应重视和积极治疗NAFLD。
脂肪肝;糖尿病,2型;发病率;队列研究
李卫东,傅坤发,连燕舒,等.成人非酒精性脂肪肝与2型糖尿病发病关系的前瞻性队列研究[J].中国全科医学,2015,18(28):3426-3429.[www.chinagp.net]
Li WD,Fu KF,Lian YS,et al.Relationship between non-alcoholic fatty liver disease and the incidence of type 2 diabetes mellitus:a prospective cohort study[J].Chinese General Practice,2015,18(28):3426-3429.Cohort Study
我国近年2型糖尿病(type 2 diabetes mellitus,T2DM)流行情况严重,20岁以上的成人T2DM患病率为9.7%。据WHO估计,2005—2013年我国由糖尿病及相关心血管疾病导致的经济损失达5 577亿美元,给社会和家庭带来严重的负担[1]。T2DM复杂的发病过程使人们至今尚未找到根治方法。T2DM的很多危险因素,如年龄、种族/民族、家族史、遗传背景以及性别等,并不能完全解释近年T2DM发病率飙升的原因,需要进一步研究已知的、可改变的危险因素,如肥胖、饮食习惯的改变、吸烟和运动减少等,甚至还应探索其他未知的危险因素,如非酒精性脂肪肝(non-alcoholic fatty liver disease,NAFLD)。国外研究显示NAFLD会增加T2DM发病危险[2-4],而近年国内NAFLD发病率呈现流行趋势[5],NAFLD是否会增加T2DM发病危险,相关证据还很缺乏,需要引起重视和研究。本研究旨在通过前瞻性队列随访,观察和分析我国成人NAFLD病史对T2DM发病的影响,现报道如下。
1 对象与方法
1.1研究对象选取2008年南京市三所医院(东南大学附属中大医院、江苏省老年医院、南京市职业病防治院)的3 616例体检职工。纳入标准:(1)年龄≥18周岁;(2)南京市居住年满5年;(3)签署知情同意书,并自愿参与研究。排除标准:(1)已诊断为T2DM者; (2)糖耐量异常者;(3)高血压患者;(4)随访时T2DM是否发病不明者。符合纳入、排除标准的职工2 475例,根据是否患有NAFLD分为NAFLD组(n=370例)和对照组(n=2 105例)。NAFLD诊断符合2010年《非酒精性脂肪性肝病诊疗指南》[6]标准定义,并排除饮酒折合乙醇量男性>140 g/周、女性>70 g/周者及肝硬化、原发性肝癌、病毒性肝炎、药物性肝病、全胃肠外营养、肝豆状核变性、自身免疫性肝病等可导致脂肪肝的特定疾病患者。本研究通过该院伦理委员会的审批。
1.2方法采用前瞻性队列研究方法,于2009—2012年对该人群进行连续4年随访,随访期间因死亡、移民、迁居失访11例,共2 464例完成队列研究(其中NAFLD组365例,对照组2 099例),随访率为99.56%。两组人群2008年基线调查内容包括:(1)一般资料:年龄、性别、文化程度、家庭人均月收入等; (2)既往病史、吸烟、饮酒、糖尿病家族史、手术史和身体活动情况等;(3)体检资料:身高、体质量、收缩压(SBP)、舒张压(DBP)、空腹血糖(FBG)、总胆固醇(TC)、三酰甘油(TG)、低密度脂蛋白(LDL)、丙氨酸氨基转移酶(ALT)、血尿酸(BUA)、血肌酐(SCr);(4)B超检查并结合饮酒情况诊断NAFLD患病情况,其中B超检查由两名医师共同诊断完成,符合2010年《非酒精性脂肪性肝病诊疗指南》[6]中关于B超诊断脂肪肝的定义。
1.3指标计算体质指数(BMI,kg/m2)=体质量(kg)/身高2(m2)。根据Ainsworth等[7]提出的身体活动代谢当量(MET)能量值概要,将睡眠、静坐活动及轻、中和重度身体活动的MET值分别定义为0.9、1.0、2.0、4.0和8.0,计算每日身体活动量=∑METn×hn,其METn为特定身体活动的代谢当量,hn为相应的平均每日活动时间。对于随访中FBG>6.1 mmol/L的职工,增加口服葡萄糖耐量试验(oral glucose tolerance test,OGTT)检查,新发T2DM的诊断均采用1999年WHO的糖尿病诊断标准[8]。所有资料由培训合格的调查人员进行面对面调查,填写问卷,血标本统一处理和生化检测。随访时间以2008年基线调查时间为随访起点,以随访期间医生初次诊断T2DM、死亡或失访,三者中先发生的事件为随访终点。
1.4统计学方法采用EpiData 3.02软件双轨录入纠错,建立数据库,采用SPSS 17.0统计软件进行统计学分析。计量资料进行正态性检验,经检验本研究中计量资料均呈正态分布,组间比较采用t检验;计数资料组间比较采用χ2检验;采用Kaplan-Meier分析累积发病率,组间比较采用Log-rank检验。为控制潜在的混杂变量,采用COX比例风险回归模型分析NAFLD与T2DM发病的关系,以对照组为参照,计算NAFLD组发生T2DM的HR(95%CI)。以P<0.05为差异有统计学意义。
2 结果
2.1两组基线资料比较两组年龄、BMI、FBG、TC、ALT、BUA水平及男性比例间差异均有统计学意义(P<0.05);而每日身体活动量、SBP、DBP、TG、LDL、SCr水平及高中以上文化程度、家庭人均月收入>1 000元、吸烟、饮酒、糖尿病家族史、手术史比例间差异均无统计学意义(P>0.05,见表1、2)。
表1 两组基线资料比较(计量资料,±s)Table 1Comparison of baseline data between the two groups

表1 两组基线资料比较(计量资料,±s)Table 1Comparison of baseline data between the two groups
注:BMI=体质指数,SBP=收缩压,DBP=舒张压,FBG=空腹血糖,TC=总胆固醇,TG=三酰甘油,LDL=低密度脂蛋白,ALT=丙氨酸氨基转移酶,BUA=血尿酸,SCr=血肌酐;1 mm Hg=0.133 kPa
组别例数年龄(岁)每日身体活动量(MET.h)BMI(kg/m2)SBP(mm Hg)DBP(mm Hg)FBG(mmol/L) ±0.5 NAFLD组36557.5±11.344±2624.5±3.3120±1177±75.2±0.5 t对照组2 09948.7±14.447±2923.1±2.8118±1176±85.1 13.1541.5277.4753.0881.8354.865 P值<0.0010.127<0.0010.0670.063<0.001组别TC(mmol/L)TG(mmol/L)LDL(mmol/L)ALT(U/L)BUA(μmol/L)SCr(μmol/L)值4±16 NAFLD组2.08±1.254.93±0.923.01±0.7228±16334±8575±15 t值对照组1.29±0.784.86±0.902.93±0.7324±15315±797<0.0010.1960.480<0.001<0.0010.506 11.6411.2941.5673.6954.1290.666 P值
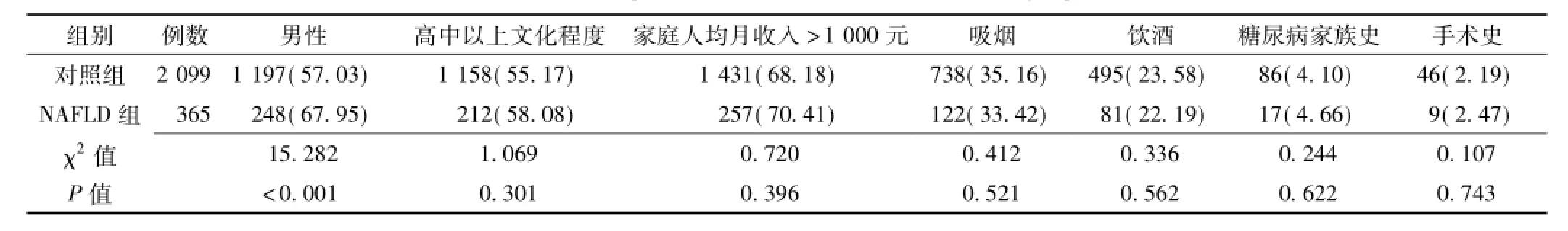
表2 两组基线资料比较〔计数资料,n(%)〕Table 2Comparison of baseline data between the two groups
2.2两组T2DM发病率及COX比例风险回归模型分析结果经过平均3.8年的随访(9 695人年,其中NAFLD组1 397人年,对照组8 298人年),共有32例发生T2DM,累积发病率为3.30/1 000人年。其中NAFLD组中有12例发生T2DM,累积发病率为8.59 /1 000人年;对照组中有20例发生T2DM,累积发病率为2.41/1 000人年。Kaplan-Meier分析显示,两组累积发病率间差异有统计学意义(χ2=21.374,P<0.001)。
与对照组相比,NAFLD组发生T2DM的HR为4.619〔95%CI(2.257,9.454),P<0.001〕(模型1);调整年龄、性别后,NAFLD组发生T2DM的HR为3.294〔95%CI(1.581,6.864),P=0.001〕(模型2);调整年龄、性别及教育程度、家庭收入、吸烟、饮酒、糖尿病家族史、手术史、每日身体活动量、FBG、TC、ALT、BUA后,NAFLD组发生T2DM的HR为3.275〔95%CI(1.545,6.942),P=0.002〕(模型3);调整年龄、性别、教育程度、家庭收入、吸烟、饮酒、糖尿病家族史、手术史、每日身体活动量、FBG、TC、ALT、BUA及BMI后,NAFLD组发生T2DM的HR为2.936〔95%CI(1.380,6.247),P=0.005〕(模型4)。
3 讨论
NAFLD是一种与胰岛素抵抗(insulin resistance,IR)和遗传易感密切相关的代谢应激性肝脏损伤,其病理学改变与酒精性肝病相似,但患者无过量饮酒史,包括单纯性脂肪肝(NAFL)、脂肪性肝炎(NASH)及其相关肝硬化和肝细胞癌[9-10]。NAFLD与T2DM的关系密切,IR是两者的共同发病机制,NAFLD与T2DM、脂代谢紊乱、动脉粥样硬化性疾病密切伴随[11],国外有研究显示NAFLD是前期糖尿病的预测因子[12],NAFLD有较高的T2DM发生率[13],也有用NAFLD的纤维化评分来预测T2DM[14]。国内对NAFLD患者T2DM的发病率研究较少。本研究多因素COX比例风险回归模型分析显示,调整年龄、性别、BMI、SBP、ALT等影响因素后,NAFLD与T2DM的发生仍呈现强关联,HR(95%CI)为2.936(1.380,6.247)。本研究初步显示NAFLD是T2DM独立危险因素,与国外研究结果一致[14-15]。
NAFLD几乎没有临床症状,加上国内对NAFLD与T2DM的关系研究不够深入,不被患者和临床医师重视,但NAFLD的某些病因去除后NAFLD可以治愈[16],但患T2DM后,特别是出现胰岛β细胞功能衰竭后,将会出现众多并发症,目前T2DM没有好的治愈方法。本队列研究初步显示NAFLD患者有较高的T2DM发病率,通过有效干预措施早期治疗NAFLD[17],使肝内堆积的脂肪降到参考范围,恢复肝脏对血糖的调节能力和激素的代谢能力,有可能降低T2DM的发病率。有研究显示T2DM是NAFLD的独立危险因素[18-19],NAFLD与T2DM的关系可能是互为因果的关系,患者可以同时身患NAFLD与T2DM两种疾病,NAFLD可以恶化糖代谢和加速T2DM提前出现并发症[20-22],T2DM又促进NAFLD进展到肝纤维化和肝硬化,增加肝病死亡风险[23-24],NAFLD与T2DM相互作用形成恶性循环,造成糖代谢紊乱和不良肝病结局,因此,需要重视和进行深入研究。
本研究的数据来源医院职工的体检数据,非随机抽样获得的样本,必然存在一定的选择偏倚,虽然B超检查筛检NAFLD是目前国内诊断NAFLD和健康体检的常用方法,但远不如CT和穿刺活检诊断NAFLD的灵敏度高,因此,本研究结论尚需大样本队列研究的进一步证实。
[1]中华医学会糖尿病学分会.中国2型糖尿病防治指南(2013年版)[J].中华糖尿病杂志,2014,6(7):447-495.
[2]Bae JC,Rhee EJ,Lee WY,et al.Combined effect of nonalcoholic fatty liver disease and impaired fasting glucose on the development of type 2 diabetes:a 4-year retrospective longitudinal study[J].Diabetes Care,2011,34(3):727-729.
[3]Shibata M,Kihara Y,Taguchi M,et al.Nonalcoholic fatty liver disease is a risk factor for type 2 diabetes in middle-aged Japanese men[J].Diabetes Care,2007,30(1):2940-2944.
[4]Musso G,Gambino R,Cassader M,et al.Meta-analysis:natural history of non-alcoholic fatty liver disease(NAFLD)and diagnostic accuracy of non-invasive tests for liver disease severity[J].Ann Med,2011,43(8):617-649.
[5]Fan JG,Farrell GC.Epidemiology of non-alcoholic fatty liver disease in China[J].J Hepatol,2009,50(1):204-210.
[6]The Chinese National Workshop on Fatty Liver and Alcoholic Liver Disease for the Chinese Liver Disease Association.Guidelines for management of nonalcoholic fatty liver disease:an updated and revised edition[J].Chin J Hepatol,2010,18(3):163-166.(in Chinese)中华医学会肝脏病学分会脂肪肝和酒精性肝病学组.非酒精性脂肪性肝病诊疗指南(2010更新版)[J].中华肝胆病杂志,2010,18(3):163-166.
[7]Ainsworth BE,Haskell WL,Leon AS,et al.Compendium of physical activities:classification of energy costs of human physical activities[J].Med Sci Sports Exerc,1993,25(1):71-80.
[8]Alberti KG,Zimmet PZ.Definition,diagnosis and classification of diabetesmellitusanditscomplications.Part1:diagnosisand classification ofdiabetesmellitusprovisionalreportofaWHO consultation[J].Diabet Med,1998,15(7):539-553.
[9]Farrell GC,Larter CZ.Nonalcoholic fatty liver disease:from steatosis to cirrhosis[J].Hepatology,2006,43(2 Suppl 1):S99-S112.
[10]Onnerhag K,Nilsson PM,Lindgren S.Increased risk of cirrhosis and hepatocellular cancer during long-term follow-up of patients with biopsy-proven NAFLD[J].Scand J Gastroenterol,2014,49 (9):1111-1118.
[11]Schild BZ,Santos LN,Alves MK.Nonalcoholic fatty liver disease and its association with metabolic syndrome in the preoperative period in patients undergoing bariatric surgery[J].Rev Assoc Med Bras,2013,59(2):155-160.
[12]Ryoo JH,Choi JM,Moon SY,et al.The clinical availability of non alcoholic fatty liver disease as an early predictor of the metabolic syndrome in Korean men:5-year's prospective cohort study[J].Atherosclerosis,2013,227(2):398-403.
[13]Zelber-Sagi S,Lotan R,Shibolet O,et al.Non-alcoholic fatty liver disease independently predicts prediabetes during a 7-year prospective follow-up[J].Liver Int,2013,33(9):1406-1412.
[14]Kasturiratne A,Weerasinghe S,Dassanayake AS,et al.Influence of non-alcoholic fatty liver disease on the development of diabetes mellitus[J].J Gastroenterol Hepatol,2013,28(1):142-147.
[15]Chang Y,Jung HS,Yun KE,et al.Cohort study of non-alcoholic fatty liver disease,NAFLD fibrosis score,and the risk of incident diabetes in a Korean population[J].Am J Gastroenterol,2013,108(12):1861-1868.
[16]Weiβ J,Rau M,Geier A.Non-alcoholic fatty liver disease: epidemiology,clinical course,investigation,and treatment[J].Dtsch Arztebl Int,2014,111(26):447-452.
[17]Da Silva HE,Arendt BM,Noureldin SA,et al.A cross-sectional study assessing dietary intake and physical activity in Canadian patients with nonalcoholic fatty liver disease vs healthy controls[J].J Acad Nutr Diet,2014,114(8):1181-1194.
[18]Williamson RM,Price JF,Glancy S,et al.Prevalence of and risk factors for hepatic steatosis and nonalcoholic fatty liver disease in people with type 2 diabetes:the Edinburgh Type 2 Diabetes Study[J].Diabetes Care,201l,34(5):1139-1144.
[19]Jimba S,Nakagami T,Takahashi M,et al.Prevalence of nonalcoholic fatty liver disease and its association with impaired glucose metabolism in Japanese adults[J].Diabet Med,2005,22(9): 1141-1145.
[20]TargherG,BertoliniL,PadovaniR,et al.Prevalenceof nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients[J].Diabetes Care,2007,30(5):1212-1218.
[21]Anstee QM,Targher G,Day CP.Progression of NAFLD to diabetes mellitus,cardiovasculardiseaseorcirrhosis[J].NatRev Gastroenterol Hepatol,2013,10(6):330-344.
[22]Targher G,Bertolini L,Rodella S,et al.Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular events in type 2 diabetic patients[J].Diabetes Care,2007,30(8):2119-2121.
[23]LeiteNC,Villela-NogueiraCA,PannainVL,et al. Histopathological stages of nonalcoholic fatty liver disease in type 2 diabetes:prevalences and correlated factors[J].Liver Int,2011,31(5):700-706.
[24]刘泽洪.丹参冻干粉治疗糖尿病非酒精性脂肪肝的疗效观察[J].实用心脑肺血管病杂志,2011,19(7):1223.
Relationship Between Non-alcoholic Fatty Liver Disease and the Incidence of Type 2 Diabetes Mellitus:A Prospective Cohort Study
LI Wei-dong,FU Kun-fa,LIAN Yan-shu,et al.Department of Gastroenterology,Zhongda Hospital Affiliated to Southeast University,Nanjing 210009,China
Objective To investigate the relation between non-alcoholic fatty liver disease(NAFLD)and the incidence of type 2 diabetes mellitus(T2DM).MethodsA prospective follow-up cohort study was conducted with employees who received physical examination in three hospitals(Zhongda Hospital Affiliated to Southeast University,Jiangsu Geriatrics Hospital and Nanjing Occupational Disease Precaution Clinic)in Nanjing.At baseline in 2008,general data,medical history,smoking,alcohol use,physical activities and physical examination data were investigated.Follow-up was undertaken from 2009 to 2012 consecutively for 4 years,and observation ended at the first diagnosis of T2DM.We included 2 464 subjects who had complete data and accorded with inclusion criteria,among which 1 445 were males and 1 019 were females.According to baseline B ultrasound examination and alcohol use,the subjects were divided into NAFLD group(n=365)and control group(n =2 099).Cox proportion risk regression model was employed to analyze the relationship between NAFLD and T2DM.Results After an average follow-up of 3.8 years(9 695 person-years;1 397 person-years for NAFLD group;8 298 person-years for control group),T2DM occurred in 32 patients,with an accumulated morbidity of 3.30/1 000 person-years.In NAFLD group,T2DM occurred in 12 patients,with an accumulated morbidity of 8.59/1 000 person-years;in control group,T2DM occurred in 20 patients,with an accumulated morbidity of 2.41/1 000 person-years.Kaplan-Meier analysis showed that the two groupswere significantly different in accumulated morbidity(χ2=21.374,P<0.001).After adjusting for age,sex,educational level,family income,smoking,alcohol use,family history of diabetes,previous surgeries,daily physical activities,FBG,TC,ALT,BUA and BMI,the HR(95%CI)of T2DM in NAFLD group was 2.936(1.380,6.247),compared with control group.ConclusionNAFLD may increase the incidence of T2DM and is an independent risk factor for T2DM.In order to reduce the occurrence of diabetes,adults should pay more attention to NAFLD and take an active manner in its treatment.
Fatty liver;Diabetes mellitus,type 2;Incidence;Cohort studies
R 575 R 587.1
A
10.3969/j.issn.1007-9572.2015.28.011
2015-06-10;
2015-08-20)
(本文编辑:崔沙沙)
210009江苏省南京市,东南大学附属中大医院消化科(李卫东,夏金荣);江苏省老年医院干部科(傅坤发);江苏建康职业学院公共卫生教研室(连燕舒);南京市职业病防治院职业健康管理中心(陈允菊)
连燕舒,210036江苏省南京市,江苏建康职业学院公共卫生教研室;E-mail:yanshuL99@163.com
