腹腔镜胃癌根治术后患者炎症因子及凝血功能变化的研究
2015-08-23鲁力谢敏熊治国
鲁力,谢敏,熊治国
腹腔镜胃癌根治术后患者炎症因子及凝血功能变化的研究
鲁力,谢敏,熊治国△
目的探讨腹腔镜胃癌根治术后患者炎症因子及凝血功能的变化。方法回顾性分析2012年6月—2014年6月在我院行胃癌治疗的77例患者,其中38例予以腹腔镜治疗(腹腔镜组),39例予以常规开腹治疗(开腹组)。分析比较2组患者术前、术后6 h、术后24 h的白介素(IL)-6、IL-8、肿瘤坏死因子-α(TNF-α)、血清活化部分凝血活酶时间(APTT)、凝血酶原时间(PT)、国际标准化比值(INR)、纤维蛋白原(FIB)、D二聚体(D-D)的水平变化情况;统计并比较2组患者术后血栓发生例数及肿瘤复发情况。结果2组患者在性别、年龄、肿瘤大小、分化程度及TNM分期上的差异均无统计学意义,具有可比性。术后2组患者血清IL-6、IL-8、TNF-α水平与术前相比均明显升高(P<0.01),且开腹组高于腹腔镜组(P<0.01)。术后2组患者APTT、PT、INR水平较术前明显降低,且腹腔镜组低于开腹组(P<0.05);2组患者术后FIB、D-D水平较术前明显升高(P<0.05),且腹腔镜组高于开腹组(P<0.05);腹腔镜组患者术后肿瘤复发例数少于开腹组,但术后血栓性疾病发生例数则多于开腹组。结论腹腔镜胃癌根治术后患者炎症介质释放减少,对机体的免疫功能影响较小,但其对患者的凝血功能影响较大,临床治疗时应加以注意。
胃肿瘤;腹腔镜检查;开腹手术;胃癌根治术;炎症因子;凝血功能
近年来,随着腹腔镜技术越来越多地应用于临床,有关腹腔镜术后患者下肢深静脉血栓以及肺栓塞的报道也相继增加,而血栓性疾病又是手术后较为严重的并发症之一,如发现和处理不及时,可能会危及患者的生命[1]。同时手术创伤对机体免疫功能也会产生一定的影响,而术后肿瘤的复发、扩散与机体的免疫功能有着紧密的联系[2]。本研究着重观察腹腔镜胃癌根治术对患者免疫功能以及凝血功能的影响,现报告如下。
1 资料与方法
1.1一般资料回顾性分析2012年6月—2014年6月在我院行胃癌根治术的77例患者,其中38例行腹腔镜治疗(腹腔镜组),39例行常规开腹治疗(开腹组),所有患者经胃镜检查和病理学诊断均为原发性胃癌。2组患者在性别、年龄、肿瘤大小、分化程度及TNM分期方面差异均无统计学意义,见表1。
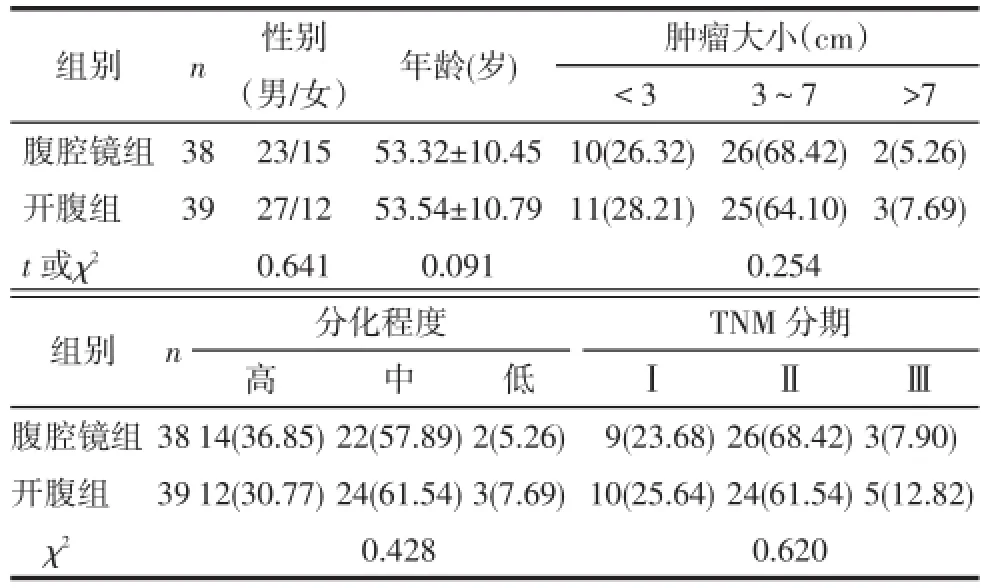
Tab.1 Comparison of the general data between two groups of patients表1 2组患者一般资料比较
1.2手术方法腹腔镜组:患者仰卧取人字位,常规气管插管全麻后脐下置入10 mm Troca作为观察孔,左侧肋缘下置入12 mm Troca作为主操作孔,左、右腹中部及右肋缘下各放置5 mm Troca作为辅助操作孔,建立CO2气腹并维持压力为12 mmHg(1 mmHg=0.133 kPa)。游离胃结肠韧带,依次离断胃网膜左动静脉、胃短血管;处理胃大弯侧至远侧切断线处,游离胃胰粘连,依次离断胃网膜右动静脉、胃右动脉、胃左动静脉;游离完肝胃韧带后于上腹部近脐处做一5 cm左右切口后常规行空肠食管吻合,观察腹腔无活动性出血,放置引流管后关腹。开腹组:依据常规手术方法进行。
1.3观察指标炎症因子指标方面采用ELISA试剂盒(上海酶联生物科技有限公司)检测2组患者术前、术后6 h、术后24 h的血清白细胞介素(IL)-6、IL-8、肿瘤坏死因子(TNF)-α及D二聚体(D-D)。凝血指标方面采用BECKMAN全自动血凝仪(美国贝克曼库尔特公司)测定2组患者术前、术后6 h、术后24 h血清活化部分凝血活酶时间(APTT)、凝血酶原时间(PT)及纤维蛋白原(FIB)水平,并采取国际标准化比值(INR)法进行计算INR,并统计2组患者术后血栓发生例数及肿瘤复发情况。
1.4统计学方法采用SPSS 17.0软件进行数据分析,2组计量资料用均数±标准差(±s)表示,组间比较采用t检验,组内不同时点比较采用重复测量数据的方差分析,计数资料比较采用卡方检验,P<0.05为差异有统计学意义。
2 结果
2.12组患者术前及术后炎症因子指标变化比较2组患者术前血清IL-6、IL-8、TNF-α水平无明显差异(P>0.05)。术后2组患者血清IL-6、IL-8、TNF-α水平均较术前明显升高(P<0.01),且开腹组高于腹腔镜组(均P<0.01),见表2。
Tab.2 Comparison of the inflammatory factor index before and after operation between two groups of patients表2 2组患者术前及术后炎症因子指标变化情况比较(ng/L,±s)
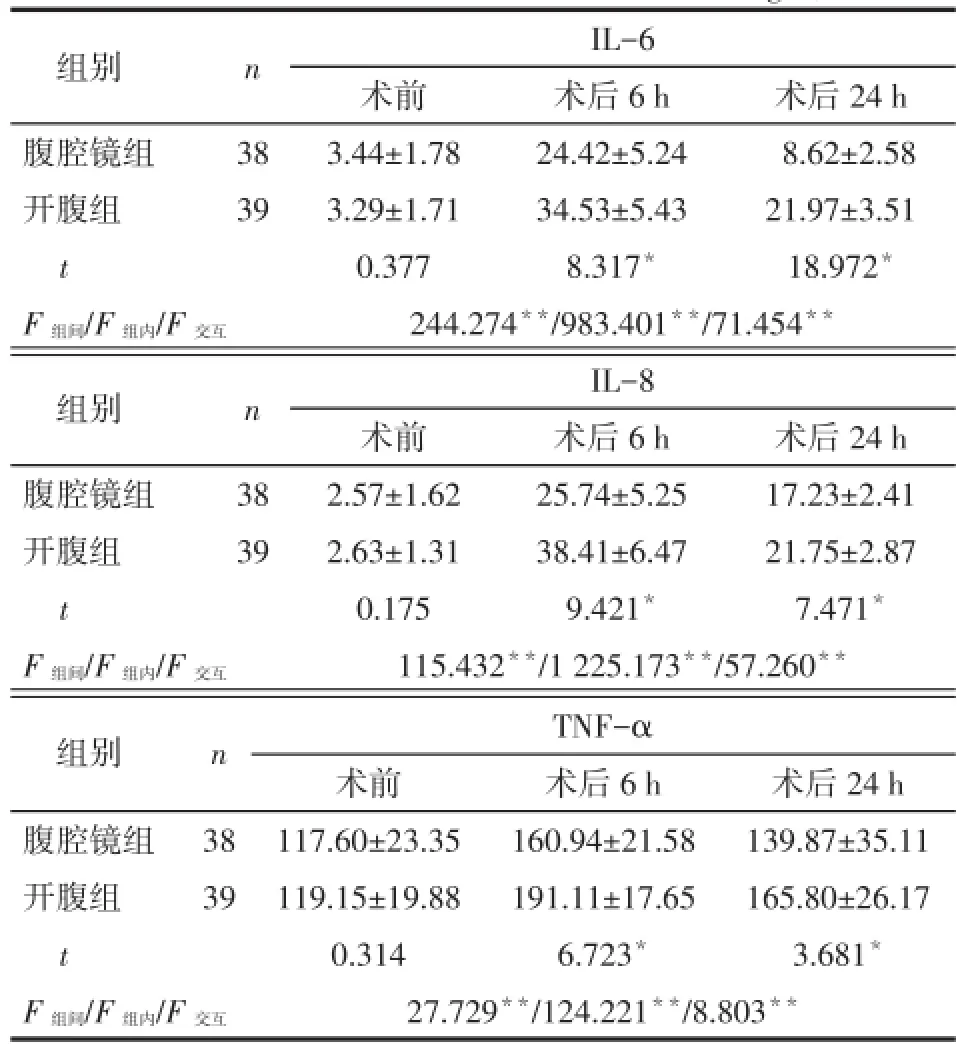
Tab.2 Comparison of the inflammatory factor index before and after operation between two groups of patients表2 2组患者术前及术后炎症因子指标变化情况比较(ng/L,±s)
*P<0.05,**P<0.01;表3同
组别腹腔镜组开腹组t F组间/F组内/F交互n 38 39 IL-6术前3.44±1.78 3.29±1.71 0.377 244.274**/983.401**/71.454**术后6 h 24.42±5.24 34.53±5.43 8.317*术后24 h 8.62±2.58 21.97±3.51 18.972*组别腹腔镜组开腹组t F组间/F组内/F交互n 38 39 IL-8术前2.57±1.62 2.63±1.31 0.175 115.432**/1 225.173**/57.260**术后6 h 25.74±5.25 38.41±6.47 9.421*术后24 h 17.23±2.41 21.75±2.87 7.471*组别腹腔镜组开腹组t F组间/F组内/F交互n 38 39 TNF-α术前117.60±23.35 119.15±19.88 0.314 27.729**/124.221**/8.803**术后6 h 160.94±21.58 191.11±17.65 6.723*术后24 h 139.87±35.11 165.80±26.17 3.681*
2.22组患者术前及术后凝血纤溶指标的变化比较2组患者术前APTT、PT、INR、FIB、D-D水平无明显差异(P>0.05)。术后2组患者APTT、PT、INR水平较术前明显降低,且腹腔镜组低于开腹组(均P<0.05);2组患者术后FIB、D-D水平则较术前明显升高(P<0.05),且腹腔镜组高于开腹组(均P<0.05),见表3。
2.32组患者术后血栓性疾病及肿瘤复发情况比较开腹组1例出现术后下肢深静脉血栓,而腹腔镜组中术后发生下肢轻度深静脉血栓7例,2组之间差异有统计学意义(χ2=5.198,P<0.05);随访2组术后1年肿瘤复发情况,腹腔镜组随访35例,失访3例,开腹组随访33例,失访6例,腹腔镜组3例患者出现肿瘤复发,而开腹组中则有10例患者出现肿瘤复发,2组之间差异有统计学意义(χ2=4.320,P<0.05)。
Tab.3 Comparison of blood coagulation and fibrinolysis indexes before and after operation between two groups of patients表3 2组患者术前及术后凝血纤溶指标的变化情况比较(±s)
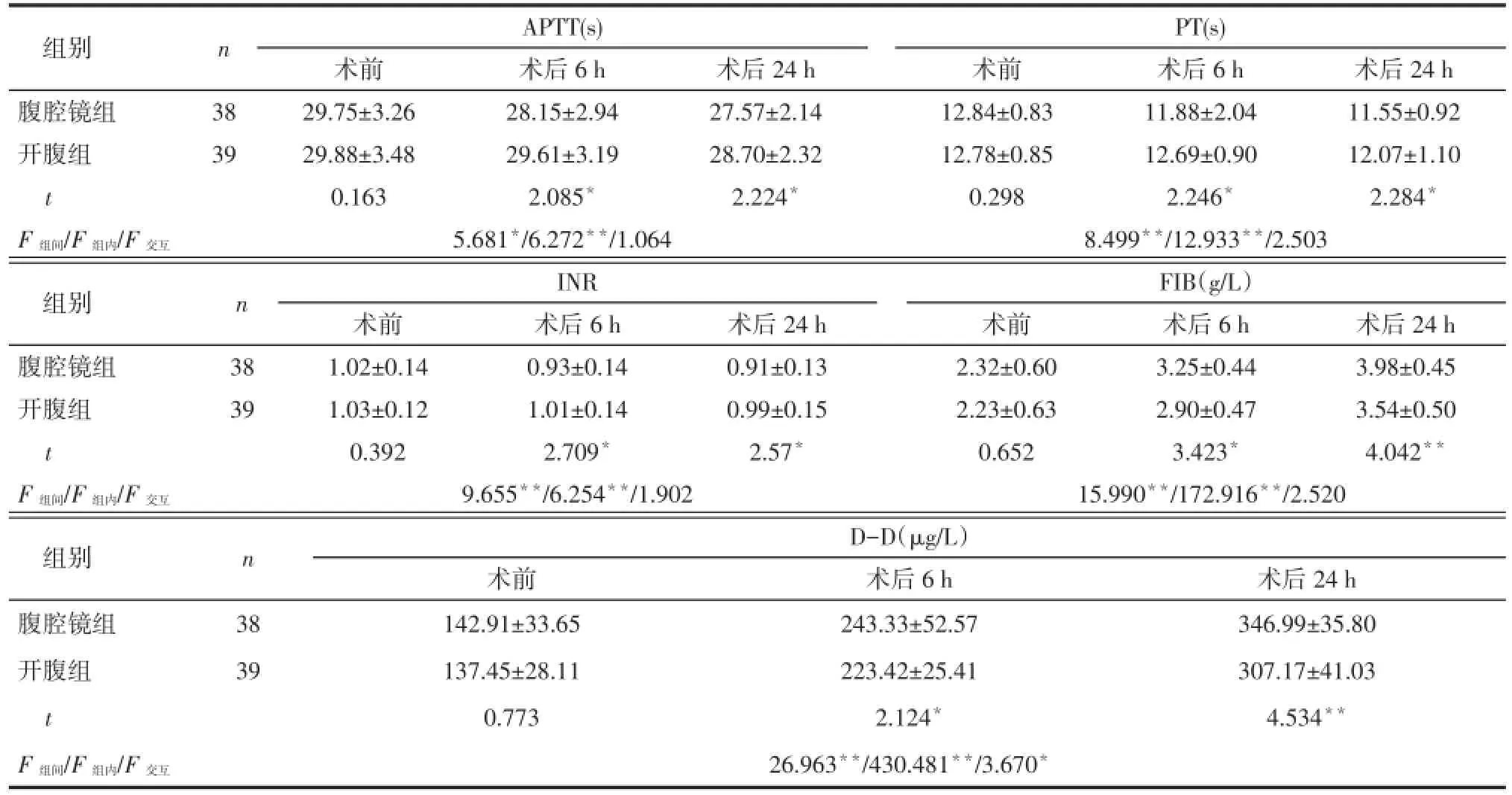
Tab.3 Comparison of blood coagulation and fibrinolysis indexes before and after operation between two groups of patients表3 2组患者术前及术后凝血纤溶指标的变化情况比较(±s)
组别腹腔镜组开腹组t F组间/F组内/F交互n 38 39 APTT(s)术前29.75±3.26 29.88±3.48 0.163 5.681*/6.272**/1.064术后6 h 28.15±2.94 29.61±3.19 2.085*术后24 h 27.57±2.14 28.70±2.32 2.224*PT(s)术前12.84±0.83 12.78±0.85 0.298 8.499**/12.933**/2.503术后6 h 11.88±2.04 12.69±0.90 2.246*术后24 h 11.55±0.92 12.07±1.10 2.284*组别腹腔镜组开腹组t F组间/F组内/F交互n 38 39 INR术前1.02±0.14 1.03±0.12 0.392 9.655**/6.254**/1.902术后6 h 0.93±0.14 1.01±0.14 2.709*术后24 h 0.91±0.13 0.99±0.15 2.57*FIB(g/L)术前2.32±0.60 2.23±0.63 0.652 15.990**/172.916**/2.520术后6 h 3.25±0.44 2.90±0.47 3.423*术后24 h 3.98±0.45 3.54±0.50 4.042**组别腹腔镜组开腹组t F组间/F组内/F交互n D-D(μg/L)38 39术前142.91±33.65 137.45±28.11 0.773术后6 h 243.33±52.57 223.42±25.41 2.124*26.963**/430.481**/3.670*术后24 h 346.99±35.80 307.17±41.03 4.534**
3 讨论
外科手术是治疗胃癌的主要方法,但手术创伤在一定程度上会导致术后机体的免疫抑制,其抑制程度与创伤的严重程度相关。有研究显示[3],由手术创伤而介导的免疫抑制可能会增加术后感染和肿瘤扩散的概率,且手术创伤对机体的凝血功能也有着一定的影响[4],因此研究不同的手术方式对于胃癌患者免疫和凝血功能的影响有着重要的意义。
IL-6在手术创伤早期即可表达,是组织损伤的敏感指标之一,与手术的创伤程度相关,其浓度的升高可以直接反映出创伤对机体造成的损害。IL-8可促进中性粒细胞脱颗粒,释放弹性蛋白酶,损伤内皮细胞,使微循环血流淤滞,组织坏死,造成器官功能损伤,进而增加患者术后感染的概率。TNF-α是炎症反应过程中出现最早、最重要的炎性介质,能激活中性粒细胞和淋巴细胞,使血管内皮细胞通透性增加,调节其他组织代谢活性并促使其他细胞因子的合成和释放,对机体的免疫反应起到抑制作用。综上,外周血中IL-6、IL-8、TNF-α水平在术后早期即可增高,且与创伤的严重程度呈正性相关,在一定程度上反映手术创伤对机体免疫功能的抑制程度[5-6]。所以,减少术后IL-6、IL-8、TNF-α的释放,对胃癌患者术后的恢复具有积极的作用。本研究结果显示术后两组患者血清IL-6、IL-8、TNF-α水平与术前相比均明显升高,但腹腔镜组明显低于开腹组,可见2种手术方式均会引起机体的炎症反应,在一定程度上抑制患者的免疫功能,但腹腔镜手术对机体的创伤更小,术后机体应激反应程度更轻,对机体免疫功能抑制更小,本研究术后2组患者肿瘤复发情况亦进一步说明这一点。
虽然腹腔镜手术对机体的创伤更小,术后机体的炎症反应更轻,但其对患者的凝血功能影响却较大。APTT主要反映内源性凝血系统状况,降低见于高凝状态,如促凝物质进入血液及凝血因子的活性增高等情况。PT主要反映外源性凝血系统状况,缩短见于血液高凝状态和血栓性疾病等。FIB主要反映纤维蛋白原的含量,D-D主要反映纤维蛋白溶解功能,增高或阳性见于继发性纤维蛋白溶解功能亢进,它们均能较为准确地反映机体凝血功能的变化[7]。本研究结果显示腹腔镜术后6 h及术后24 h 的APTT、PT及INR水平较开腹组降低,FIB、D-D水平较开腹组升高,这反映出腹腔镜组患者术后血液凝固性高于开腹组,本研究结果部分2组患者术后血栓性疾病的发生例数与此结论相符合。腹腔镜组血液凝固性较高的原因可能为腹腔镜手术时CO2气腹对腹腔血管的影响,手术操作中长时间的头高脚低位,以及因腹腔镜下分离血管、清扫淋巴结等操作困难导致手术时间延长造成静脉血液瘀滞,增加了激活的血小板和凝血因子与静脉壁接触的时间,容易引起血栓形成,是下肢深静脉血栓形成的首要因素[8]。因此,在腹腔镜手术治疗时应对患者血液高凝状态予以注意。
综上,腹腔镜胃癌根治术具有创伤小、恢复快、术后机体应激反应程度轻及对机体的免疫功能影响小等优点,但其对患者凝血系统的影响较大。因此,在胃癌患者腹腔镜手术治疗时,应做好全面的评估,并采取相应的措施,预防高凝状态的出现,努力避免患者术后深静脉血栓的形成。
[1]De Martino RR,Goodney PP,Spangler EL,et al.Variation in thromboembolic complications among patients undergoing commonly performed cancer operations[J].J Vasc Surg,2012,55(4):1035-1040.
[2]Finn OJ.Immuno-oncology:understanding the function and dysfunction of the immune system in cancer[J].Ann Oncol,2012,23(Suppl 8):viii6-9.
[3]Chopra SS,Haacke N,Meisel C,et al.Postoperative immunosuppression after open and laparoscopic liver resection:assessment of cellular immune function andmonoc-Ytic HLA-DR expression[J]. JSLS,2013,17(4):615-621.
[4]Weinberg L,Scurrah N,Parker FC,et al.Markers of coagulation activation after hepatic resection for cancer:evidence of sustained upregulation of coagulation[J].Anaesth Intensive Care,2011,39(5): 847-853.
[5]Watanabe T,Takahashi A,Suzuki K,et al.Epithelial-mesenchymal transition in human gastric cancer cell lines induced by TNF-a-inducing protein of Helicobacter pylori[J].Int J Cancer,2014,134(10): 2373-2382.
[6]Ruzzo A,Catalano V,Canestrari E,et al.Genetic modulation of the interleukin 6(IL-6)system in patients with advanced gastric cancer:a background for an alternative target therapy[J].BMC Cancer,2014,14(1):357.
[7]Ma X,Li Y,Zhang J,et al.Prognostic role of D-dimer in patients with lung cancer:a meta-analysis[J].Tumour Biol,2014,35(3): 2103-2109.
[8]HuangZP,LiuXJ,ZouBX,etal.The complete recanalization of PICC-related ve-nous thrombosis in cancer patients:A series of case reports[J].Exp Ther Med,2013,6(2):411-412.
(2014-07-09收稿2014-08-29修回)
(本文编辑李国琪)
Researches on inflammatory factor and blood coagulation in patients with laparoscopic gastric cancer radical surgery
LU Li,XIE Min,XIONG Zhiguo△
Hubei Cancer Hospital,Wuhan 430071,China
△Corresponding AuthorE-mail:1790946193@qq.com
ObjectiveTo investigate the change of inflammatory factor and blood coagulation in patients with laparoscopic gastric cancer radical surgery.MethodsData of seventy-seven stomach cancer patients hospitalized in our hospital and received the surgical treatment from June 2012 to June 2014 were retrospectively analyzed.Thirty-eight of these patients underwent laparoscopic treatment(laparoscopic group)and 39 cases received laparotomy treatment(laparotomy group). The values of interleukin-6(IL-6),IL-8 and tumor necrosis factor alpha(TNF-α)were analyzed at the time points of preoperation and 6 h,24 h after the surgery in two groups.The levels of activated partial thromboplastin time(APTT),prothrombin time(PT),international standardization ration(INR),fibrinogen(FIB)and D dimer(D-D)were also analyzed at the same time points in two groups.The postoperative thrombosis and tumor recurrence rate were also analyzed in two groups of patients.ResultsThere were no significant differences in the gender,age,the size of tumor,differentiation degree and TNM staging between two groups of patients.The serum levels of IL-6,IL-8 and TNF-α were significantly increased after surgery in two groups(P<0.01),and which were significantly higher in laparotomy group than those of laparoscopic group(P<0.01).The levels of APTT,PT and INR were significantly lower after surgery in two groups of patients,and which were significantly lower in laparoscopic group than those of laparotomy group(P<0.05).The levels of FIB and D-D were significantly increased after operation in two groups of patients(P<0.05),which were significantly higher in laparoscopic group than those of laparotomy group(P<0.05).The postoperative recurrence of cancer was less in laparoscopic group than that of laparotomy group.But,the postoperative thrombosis was more in laparoscopic group than that of laparotomy group.Conclusion There was less release of inflammatory mediators and less effect on the body's immune function in patients with laparoscopic gastric cancer radical surgery.But,the surgery has a large influence in blood coagulation,we should pay attention to it in the clinical treatment.
stomach neoplasms;laparoscopy;laparotomy;gastric cancer radical gastrectomy;inflammatory factor;blood coagulation function
R735.2
ADOI:10.11958/j.issn.0253-9896.2015.03.014
湖北省自然科学基金资助项目(2013CFC023)
武汉,湖北省肿瘤医院胃肠外科(邮编430071)
鲁力(1978),男,博士,主要从事消化道肿瘤研究
△E-mail:1790946193@qq.com