血清血脂及载脂蛋白水平与乳腺癌的相关性
2015-05-30蒋圣早陈东祥
蒋圣早 陈东祥


[摘要] 目的 探討血脂及载脂蛋白与乳腺癌的相关性。 方法 取2012年3月~2014年3月在我院确诊为乳腺浸润性导管癌的82例患者及健康体检对照者80例的血清,分析血清总胆固醇(TC)、甘油三酯(TG)、载脂蛋白A(Apo-A)、载脂蛋白B(Apo-B)、高密度脂蛋白胆固醇(HDL-C)和低密度脂蛋白胆固醇(LDL-C)水平,并根据肿瘤的大小、淋巴结转移、组织分化程度等情况进行分组,比较各组的测定值。 结果 乳腺癌组TC、TG、LDL-C、Apo-B分别为(6.20±0.24)mmol/L、(2.45±0.12)mmol/L,(4.58±0.20)mmol/L、(1.25±0.15)g/L,对照组为(4.00±0.20)mmol/L、(0.67±0.17)mmol/L、(2.14±0.22)mmol/L、(0.86±0.24)g/L,乳腺癌组明显高于对照组,两组比较差异有统计学意义(P<0.05);乳腺癌组HDL-C、Apo-A分别为(0.90±0.11)mmol/L、(1.20±0.22)g/L,对照组为(1.98±0.21)mmol/L、(1.36±0.20)g/L,乳腺癌组低于对照组,两组比较差异有统计学意义(P<0.05)。大小≥2 cm组TC显著高于<2 cm组(P<0.05)。淋巴结转移者TC、TG、HDL-C、LDL-C、Apo-A、Apo-B与无转移者比较差异无统计学意义。乳腺癌低分化组血清TG水平高于高分化组,而高分化组血清HDL-C、Apo-A水平低于低分化组,差异有统计学意义(P<0.05)。 结论 TC、TG、LDL-C、Apo-B异常升高,HDL-C、Apo-A的异常下降与乳腺癌的发生及恶变有相关性。
[关键词] 乳腺癌;血脂;载脂蛋白
[中图分类号] R737.9 [文献标识码] A [文章编号] 1673-9701(2015)14-0017-04
[Abstract] Objective To investigate the correlation between serum lipids, apolipoprotein and breast cancer. Methods A survey on the prevalence of breast cancer was conducted in out hospital from March 2012 to March 2014. The data of 82 subjects with histologically confirmed breast cancer and 80 healthy control subjects were analyzed. Serum TC, TG, Apo-A, Apo-B, HDL-C, LDL-C were tested at the same time. The grouped according to tumor size, lymph node metastasis, the degree of tissue differentiation, measured values were compared. Results The levels of serum TC,TG,LDL-C, Apo-B in the breast cancer group were (6.20±0.24) mmol/L, (2.45±0.12) mmol/L, (4.58±0.20) mmol/L, (1.25±0.15)g/L respectively, while those in the control group were (4.00±0.20) mmol/L, (0.67±0.17) mmol/L, (2.14±0.22) mmol/L, (0.86±0.24) g/L respectively.All above parameters of the breast cancer group were significantly higher than those in the control group (P<0.05). The levels of serum HDL-C, Apo-A in the breast cancer group were (0.90±0.11) mmol/L and (1.20±0.22) g/L, and those in the control group were (1.98±0.21) mmol/L and (1.36±0.20) g/L, which was significantly lower than that of the control group (P<0.05). The serum TC level were significantly higher in the lump≥2 cm group than that of < 2 cm group (P<0.05). There was not significant difference between patients with lymph node metastasis and non-metastasis for the levels of serum TC, TG, HDL-C, LDL-C, Apo-A and Apo-B. The levels of serum TG in the breast cancer poorly differentiated group were higher than those in the well differentiated group (P<0.05). And in the well differentiated group, but the serum HDL-C, Apo-A were significantly lower than in poorly differentiated group, the differences were statistically significant(P<0.05). Conclusion Abnormal elevated of the serum TC, TG, LDL-C, Apo B and HDL-C, Apo-A decline is related to the tumors accruing and development of breast cancer.
[Key words] Breast cancer; Serum lipid; Apolipoprotein
乳腺癌是女性最常见的恶性肿瘤之一。目前,发病呈上升趋势,但其病因尚不清楚。近年来研究显示:生活方式、饮食因素与乳腺癌的发病有一定关系。本研究拟通过检测乳腺癌患者血清总胆固醇(TC)、甘油三酯(TG)、载脂蛋白A(Apo-A)、载脂蛋白B(Apo-B)、高密度脂蛋白胆固醇(HDL-C)和低密度脂蛋白胆固醇(LDL-C)水平,探讨乳腺癌发生的危险因素,为乳腺癌的预防和治疗提供科学依据,现报道如下。
1 对象与方法
1.1 研究对象
选择2012年3月~2014年3月在我院经病理学确诊的乳腺癌患者82例为研究对象,均为女性;年龄25~81岁,平均(53.7±12.3)岁。根据乳腺肿块的大小分为<2 cm组(60例)和≥2 cm组(22例);另按淋巴结转移情况,将其分为转移组(50例)和无转移组(32例);根据组织分化程度分为低分化组(60例)、中分化组(14例)和高分化组(8例)。随机抽取同期行健康体检者为对照组,共80例,均为女性,年龄25~76岁,平均(55.2±14.6)岁。入组者均已排除乳腺癌手术史、原发性高血脂症及影响血脂代谢的相关疾病和药物。两组平均年龄差异无统计学意义(P>0.05),具有可比性。
1.2 方法
清晨收集受检者静脉血2 mL,将其置于枸椽酸钠抗凝液试管中,3000 r/min离心10 min。取血清,采用直接法测定HDL-C、LDL-C,全自动生化分析仪酶比色法测定TC、TG,免疫透射比浊法测定Apo-A、Apo-B。试剂及试剂盒均由上海复星长征医学科学有限公司提供。为了避免误差均采用双管测定后取其平均值。仪器为西门子advia-2400生化分析仪。
1.3 统计学方法
用SPSS 13.0统计学软件进行处理,计量资料以(x±s)表示,组间比较采用t检验,多组间比较采用单因素方差分析,相关分析采用Logistic回归等方法进行分析。P<0.05为差异有统计学意义。
2 结果
2.1 乳腺癌组及对照组、乳腺癌临床病理特征与血脂水平的比较
乳腺癌组TC、TG、LDL-C、Apo-B分别为(6.20±0.24)mmol/L、(2.45±0.12)mmol/L、(4.58±0.20)mmol/L、(1.25±0.15)g/L,对照组为(4.00±0.20)mmol/L、(0.67±0.17)mmol/L、(2.14±0.22)mmol/L、(0.86±0.24)g/L,乳腺癌组明显高于对照组,两组比较差异有统计学意义(P<0.05);乳腺癌组HDL-C、Apo-A分别为(0.90±0.11)mmol/L、(1.20±0.22)g/L,對照组为(1.98±0.21)mmol/L、(1.36±0.20)g/L,乳腺癌组低于对照组,两组比较差异有统计学意义(P<0.05)。肿块大小≥2 cm组TC[(6.50±0.15)mmol/L]显著高于<2 cm组[(4.65±0.21)mmol/L](P<0.05)。淋巴结转移者TC、TG、HDL-C、LDL-C、Apo-A、Apo-B与无转移者比较差异无统计学意义。乳腺癌低分化组血清TG水平高于高分化组,差异有统计学意义(P<0.05),而高分化组血清HDL-C、Apo-A水平低于低分化组,差异有统计学意义(P<0.05)。见表1。
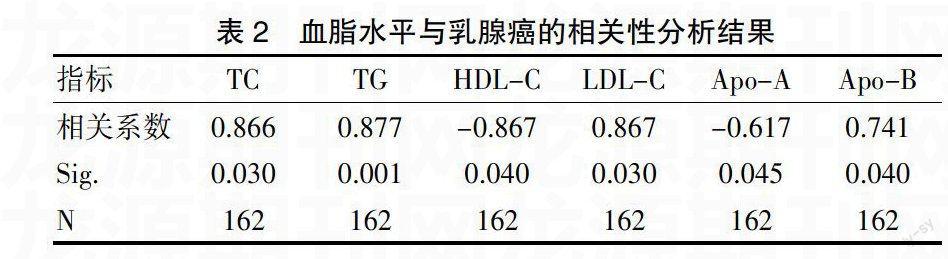
2.2 乳腺癌与血脂水平的相关性分析
乳腺癌与TC、TG、LDL-C、Apo-B的相关系数(r)分别为0.866(P<0.05)、0.877(P<0.01)、0.867(P<0.05)、0.741(P<0.05),呈正相关关系;乳腺癌与HDL-C、Apo-A相关系数为-0.867(P<0.05)、-0.617(P<0.05),呈负相关。见表2。
2.3 乳腺癌发生与相关因素的Logistic回归分析
以乳腺癌作为因变量,将TC、TG、HDL-C、LDL-C、Apo-A和Apo-B作为自变量,用Logistic回归分析,逐步剔除作用不显著的变量,结果显示TC、TG、HDL-C、Apo-A和Apo-B是乳腺癌发生的危险因素(P<0.05),见表3。
3 讨论
乳腺癌是女性最常见的恶性肿瘤之一,在我国占全身各种恶性肿瘤的7%~10%,并呈逐年上升趋势,其病因尚不清楚。但营养过剩、肥胖、脂肪饮食,可加强或延长雌激素对乳腺上皮细胞的刺激,从而增加发病机会[1]。有关血脂与乳腺癌发生的关系,国内外文献报道较少,且结论不一。Psaltopoulou等[2]2011年系统回顾分析了13800例患者和23340例对照的橄榄油摄入量结果认为其与乳腺癌呈负相关。Smith-Warner等[3]认为膳食脂肪摄取量与乳腺癌无相关性,而Boyd等[4]认为高脂肪摄入量与乳腺癌密切相关。国内的相关报道多与高脂血症相关,认为血脂与乳腺癌的发生有密切关系[5]。本研究显示,乳腺癌组血清TC、TG、LDL-C、Apo-B高于对照组,而血清HDL-C、Apo-A则低于对照组,差异有统计学意义(P<0.05),与李国静等[5]的研究一致。肿瘤细胞的生长需要胆固醇,这就会导致内源性胆固醇合成增加。有研究表明,恶性肿瘤细胞的LDL-C受体常呈下调状态,这导致羟甲基戊二酞辅酶A(HMG-CoA)还原酶的活性增高,而HMG-CoA还原酶通路重新合成的内源性胆固醇可以激活肿瘤细胞的增殖[6]。抑制内源性胆固醇合成的药物如洛伐他汀或辛伐他汀在体内和体外实验中也证实,它们可以显著降低肿瘤细胞的穿血管内皮细胞移行能力[7],Ahern等[8]对18769例丹麦Ⅰ~Ⅲ期浸润性乳腺癌女性患者进行的前瞻性队列研究也同样证实亲脂类他汀药物的使用能明显降低乳腺癌患者的复发率。同时通过HDL-C受体信号通路活性提高来调节细胞内胆固醇的积累,从而导致血清HDL-C水平降低[9]。提示脂质代谢水平在乳腺癌的发生及发展过程中可能发挥着重要作用。
李国静等[5]认为乳腺癌患者血清TC水平升高,高脂血症与乳腺癌密切相关。而潘巨龙等[10]研究认为乳腺癌患者血清TC水平降低,在伴有骨转移的患者中更加明显。刘煦禾等[11]的研究发现乳腺癌晚期患者TC水平较早期明显增加。Bahl等[12]认为高水平的TC患者复发率增加。本研究结果显示,肿块≥2 cm组的TC较肿块<2 cm组明显升高,提示TC与乳腺癌生长有一定关系。其机制可能是高浓度的TC及其前体物质导致肿瘤细胞异常过度增殖,羟甲基戊二酰辅酶 A(HMG-CoA)还原酶的活性增高,其作为是乳腺癌患者TC合成的限速酶会加速合成TC以满足癌细胞合成细胞膜的需要。
在对脂类水平和乳腺癌的相关性的研究中发现,TG水平与乳腺癌的发病风险呈正相关。研究证实高TG比率乳腺癌患者易远处转移。Lipscombe等[13]发现,乳腺癌组织中TG的代谢明显比周围组织快,Han等[14]也发现,乳腺癌患者血清TG水平升高。本研究显示乳腺癌低分化组血清TG高于高分化组,与上述研究结果一致。其原因可能是乳腺癌细胞的过度增殖需消耗大量的能量,脂质代谢异常活跃,大量脂肪动员,血清 TG 水平升高。而高分化组血清HDL-C、Apo-A低于低分化组,差异有统计学意义(P<0.05)。提示TG、HDL-C、Apo-A可能与乳腺癌的恶性程度有关。
本研究结果发现,淋巴结转移组与淋巴结无转移组TC、TG、HDL-C、LDL-C、Apo-A、Apo-B水平无统计学差异,考虑可能与病例数少有关。目前,血脂与乳癌关系的研究机制尚不明确,可能与乳腺组织的发育受雌激素的控制有关[15],研究表明,膳食脂肪增加内源性雌激素的生产可能会导致乳腺癌[16,17]。当脂肪代谢紊乱时,高浓度游离脂肪酸可导致血液游离雌激素增加,刺激乳腺上皮细胞增生及分化。血液中高浓度不饱合脂肪酸容易被氧化,生成脂质过氧化物,产生过多自由基,从而导致细胞突变[18],而减少脂肪摄入量有可能降低患乳腺癌的风险[19]。
综上,乳腺癌患者存在一定程度的血脂代谢改变,TC、TG、Apo-B升高及HDL-C、Apo-A下降与乳腺癌具有相关性,应引起临床重视,能否可以作为预测乳腺癌发生的有效指标,尚需进一步的研究。
[参考文献]
[1] 陈孝平. 外科学[M]. 第2版. 北京:人民卫生出版社,2012:399.
[2] Psaltopoulou T,Kosti RI,Haidopoulos D,et al. Olive oil intake is inversely related to cancer prevalence: A systematic review and a meta-analysis of 13800 patients and 23340 controls in 19 observational studies[J]. Lipids Health Dis,2011,30(10):127.
[3] Smith-Warner SA,Spiegelman D,Adami HO,et al. Types of dietary fat and breast cancer: A pooled analysis of cohort studies[J]. Int J Cancer,2001,92(5):767-774.
[4] Boyd NF,Stone J,Vogt KN,et al. Dietary fat and breast cancer risk revisited: A meta-analysis of the published literature[J]. Br J Cancer,2003,89(9):1672-1685.
[5] 李國静,罗春华,易虹,等. 52例乳腺癌患者血脂检测结果分析[J]. 中国妇幼保健,2004, 19(14):83-84.
[6] Mehta N,Hordines J,Solpe C,et al. Cellular effects of hypercholesterolemia in modulation of cancer growth and metastasis:a review of the evidence[J]. Surg Oncol,1997,6(3):179-185.
[7] Kusama T,Mukai M,Iwasaki T,et al. 3-hydroxy-3-methylglutaryl-coenzyme a reductase inhibitors reduce human pancreatic cancer cell invasion and metastasis[J]. Gastroenterology,2002,122(2):308-317.
[8] Ahern TP,Pedersen L,Tarp M,et al. Statin prescriptions and breast cancer recurrence risk:A Danish nationwide prospective cohort study[J]. Journal of the National Cancer Institute,2011,103(19):1461-1468.
[9] Guo EQ,Chen LR,Xie QP,et al. Serum HDL-C as a potential biomarker for nodal stages in gastric cancer[J]. Ann Surg Onco1,2009,14(9):2528-2534.
[10] 潘巨龙,严佳斌,郑玉萍. 乳腺癌骨转移患者血脂和血浆 CA153 联检对早期诊断的临床价值[J]. 放射免疫学杂志,2012,25(4):463-465 .
[11] 劉煦禾,唐来. 乳腺癌患者血浆总胆固醇及高密度脂蛋白与乳腺癌临床分期的相关性研究[J]. 海南医学院学报,2011,17(6):806-808.
[12] Bahl M,Ennis M,Tannock IF,et al. The prognostic effect of lipids on early-stage breast cancer outcome[J]. J Clin Oncol,2005,23(16):710.
[13] Lipscombe LL,Goodwin PJ,Zinman B,et al. Diabetes mellitus and breast cancer:a retrospective population-based cohort study[J]. Breast Cancer Res Treat,2006,98(3):349-356.
[14] Han C,Zhang HT,Du L,et al. Serum levels of leptin,insulin,and lipids in relation to breast cancer in China[J]. Endocrine,2005,26(1):19-24.
[15] Wu AH,Stram DO,Pike MC. RESPONSE: Re: Meta-analysis: Dietary fat intake,serum estrogen levels,and the risk of breast cance[J]. J Natl Cancer Inst,1999,92(1):1512.
[16] Parry BM,Milne JM,Yadegarfar G,et al. Dramatic dietary fat reduction is feasible for breast cancer patients: Results of the randomised study,WINS(UK)-stage 1[J]. Eur J Surg Oncol,2011,37:848-855.
[17] Holmes MD,Hunter DJ,Colditz GA,et al. Association of dietary intake of fat and fatty acids with risk of breast cancer[J]. JAMA,1999,28(10):914-920.
[18] Rock CL,Flatt SW,Thomson CA,et al. Effects of a high-fiber,low-fat diet intervention on serum concentrations of reproductive steroid hormones in women with a history of breast cancer[J]. J Clin Oncol,2004,22(12):2379-2387.
[19] Khodarahmi M,Azadbakht L. The association between different kinds of fat intake and breast cancer risk in women[J]. Int J Prev Med,2014,5(1):6-15.
(收稿日期:2014-12-25)
