Therapeutic efficacy observation on bloodletting and cupping for cervical radiculopathy
2015-05-18MouMingyuan牟明园PiaoShengai朴盛爱MengXiangwen孟向文GuoYi郭义ChenZelin陈泽林ZhuChenghui朱成慧ZhaoQiang赵强ZhangYaowei张耀巍Fuquan吕福全XingJunbiao邢俊标DiaoDianjun刁殿军GengLianqi耿连奇LiDandan李丹丹LiuHuapeng刘华朋LokeshKumarKarna乐天
Mou Ming-yuan (牟明园), Piao Sheng-ai (朴盛爱), Meng Xiang-wen (孟向文), Guo Yi (郭义), Chen Ze-lin (陈泽林), Zhu Cheng-hui (朱成慧), Zhao Qiang (赵强), Zhang Yao-wei (张耀巍), Lü Fu-quan (吕福全), Xing Jun-biao (邢俊标), Diao Dian-jun (刁殿军), Geng Lian-qi (耿连奇), Li Dan-dan (李丹丹), Liu Hua-peng (刘华朋), Lokesh Kumar Karna (乐天)
1 Acupuncture and Tuina School, Tianjin University of Traditional Chinese Medicine, Tianjin 300193, China
2 Hospital Affiliated to Tianjin Research Academy of Traditional Chinese Medicine, Tianjin 300120, China
3 Tianjin Heping Hospital of Traditional Chinese Medicine, Tianjin 300050, China
4 Tianjin Nankai Hospital, Tianjin 300120, China
5 Tianjin Wuqing Hospital of Traditional Chinese Medicine, Tianjin 301700, China
6 Tianjin Tanggu Hospital of Traditional Chinese Medicine in Binhai New District, Tianjin 300000, China
Therapeutic efficacy observation on bloodletting and cupping for cervical radiculopathy
Mou Ming-yuan (牟明园)1, Piao Sheng-ai (朴盛爱)1, Meng Xiang-wen (孟向文)1, Guo Yi (郭义)1, Chen Ze-lin (陈泽林)1, Zhu Cheng-hui (朱成慧)1, Zhao Qiang (赵强)2, Zhang Yao-wei (张耀巍)3, Lü Fu-quan (吕福全)4, Xing Jun-biao (邢俊标)5, Diao Dian-jun (刁殿军)5, Geng Lian-qi (耿连奇)6, Li Dan-dan (李丹丹)1, Liu Hua-peng (刘华朋)1, Lokesh Kumar Karna (乐天)1
1 Acupuncture and Tuina School, Tianjin University of Traditional Chinese Medicine, Tianjin 300193, China
2 Hospital Affiliated to Tianjin Research Academy of Traditional Chinese Medicine, Tianjin 300120, China
3 Tianjin Heping Hospital of Traditional Chinese Medicine, Tianjin 300050, China
4 Tianjin Nankai Hospital, Tianjin 300120, China
5 Tianjin Wuqing Hospital of Traditional Chinese Medicine, Tianjin 301700, China
6 Tianjin Tanggu Hospital of Traditional Chinese Medicine in Binhai New District, Tianjin 300000, China
Objective:To observe the efficacy and safety of bloodletting and cupping for cervical radiculopathy.
Acupuncture Therapy; Blood-letting Puncturing and Cupping; Neck Pain; Spondylosis; Cervical Spondylosis; Randomized Controlled Trials
Cervical radiculopathy refers to signs and symptoms resulting from cervical stenosis, degenerated cervical spine and herniated cervical intervertebral discs compressing the nerve root[1]. The male/female incidence ratio is 1:7[2]. This condition affects 3.3% of the population, especially in their 4th or 5th decade[3]. Cervical radiculopathy is clinically characterized by pain and numbness in the neck that radiate towards the shoulder and arms, coupled with weakness and heaviness of the upper limbs. Patients with cervical radiculopathy often turn to conservative therapy. Surgery is an option only when their symptoms persist or progress[4]. Conservative therapies include nonsteroidal anti-inflammatory drugs (NSAIDs), exercise, manipulation therapy[5], cervical collar (neck brace)[6], muscle relaxants[7], pain killers, physical therapy apparatus[8], Chinese medicine[9-10], acupuncture[11], electroacupuncture[12], bee venom acupuncture[13], tuina[14]and bloodletting[15], etc. Of these therapies, acupuncture has exact effect for cervical spondylosis[16]and bloodletting is another popular external therapy for neck problems[17]. However, the literature references have low levels of evidence and there are no clinical reports regarding the effect of bloodletting therapy on cervical radiculopathy. This clinical trial aimed to evaluate and compare its effect with acupuncture in this regard.
1 Clinical Materials
1.1 Diagnostic criteria
This was based on the diagnostic basis for cervical radiculopathy in theGuidelines for Diagnosis, Treatment and Rehabilitation of Cervical Spondylosisby Chinese Association of Rehabilitation Medicine[18](2007, Beijing): signs and symptoms (numb, pain) along the nerve that is irritated travels; positive brachial plexus tension test or Spurling sign; imaging findings showed consistency with clinical manifestations; exclusion of pain due to other cervical conditions (thoracic outlet syndrome, tennis elbow, carpal-tunnel syndrome, cubital tunnel syndrome, frozen shoulder and tendosynovitis involving the long head of the biceps brachii muscle).
1.2 Inclusion criteria
Those who met the above diagnostic criteria; having no indications for surgery; aged between 18 and 70 years; and signed the informed consent.
1.3 Exclusion criteria
Having posterior longitudinal ligament calcification of the cervical spine and congenital cervical spine deformity (such as developmental cervical stenosis); a history of cervical trauma; those who failed to respond to nonsurgical therapies within 3-6 months or having recurrences; presence of progressive muscular atrophy or motor disorder; failure of nonsurgical therapies confirmed by imaging findings; having complications of severe heart, brain, lung and kidney diseases; having severe infection in other body parts (such as throat problems); having osteoporosis; pregnant and breast-feeding women; and those who had been taking more than 5 types of Western drugs for 3 successive years.
1.4 Rejection criteria
Having a poor compliance and an inability to cooperate during the trial; those who could not receive treatment and follow-up due to other reasons.
1.5 Statistical method
The data analysis was done using the SPSS 19.0 version software. The measurement data in normal distribution were expressed asThe intra-group comparison before and after treatment was conducted by repeated Measures analysis of variance, whereas the inter-group comparison by One-way ANOVA. The measurement in abnormal distribution were expressed as median (interquartile range) [M (Q)]. The intra-group comparison before and after treatment was conducted by Friedman test, whereas the inter-group comparison by H test. The enumeration data comparison was conducted by the Chi-square test. APvalue of less than 0.05 indicates a statistical significance.
1.6 General data
A total of 183 cases in this trial were from five centers: Hospital Affiliated to Tianjin Research Academy of Traditional Chinese Medicine, Tianjin Heping Hospital of Traditional Chinese Medicine, Tianjin Wuqing Hospital of Traditional Chinese Medicine, Tianjin Nankai Hospital and Tianjin Tanggu Hospital of Traditional Chinese Medicine in Binhai New District. According to the computer-generated random number, the random cards were placed into random envelops with sequential numbers. Then the above cases were allocated into a bloodletting group, an acupuncture group and a combined group. All cases signed the informed consent. This trial had been approved by the Medical Ethics Committee, Tianjin University of Traditional Chinese Medicine. There were no inter-group statistical significances in gender, age and duration (allP>0.05), indicating that the three groups were comparable (Table 1).
2 Treatment Methods
2.1 Bloodletting group
Points: Dazhui (GV 14) and Jianjing (GB 21)[19].
Device: BCI-101 lancing device (manufactured by (AME Corporation, Korea) and I-type disposable lancing needle (manufactured by Tianjin Huahong Technology Co., Ltd., China).
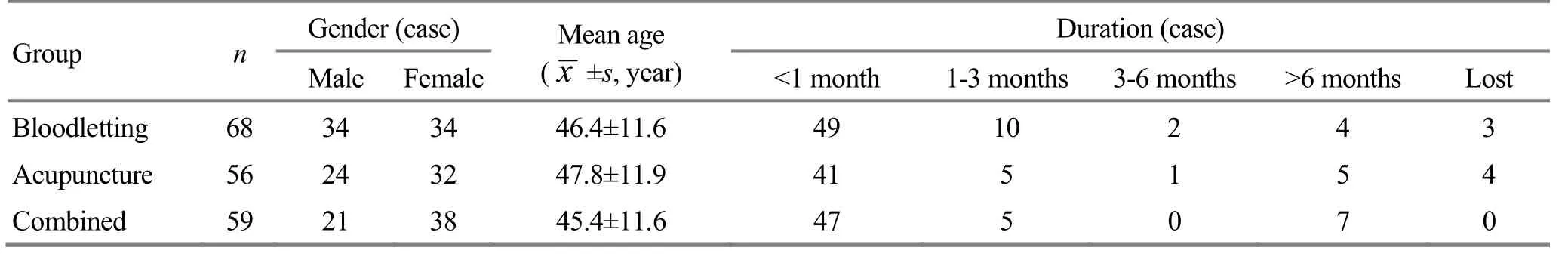
Table 1. Inter-group comparison of baseline data
Method: The patient was asked to take a prone lying position. The area within 2 cm around Dazhui (GV 14) and Jianjing (GB 21) were sterilized and let blood using a lancing device that contains a disposable needle, followed by 5-10 min of cupping (Figure 1), 5 mL blood for each cup, for a total of 2-3 cups.

Figure 1. Bloodletting and cupping
2.2 Acupuncture group
Points: Bilateral cervical (C3-7) Jiaji (EX-B 2) points and Jianjing (GB 21) on the affected side[19].
Device: Disposable filiform needles of 0.3 mm in diameter and 40 mm in length.
Method: The patient was asked to take a prone lying position. After routine sterilization, the above points were punctured at a depth between 25 mm and 38 mm, followed by 30-second sparrow-pecking manipulation upon arrival of qi until the presence of local soreness and distension. The needles were retained for 30 min and manipulated once during the needle retention.
2.3 Combined group
Patients in this group first received same bloodletting and cupping as the bloodletting group and then the same acupuncture therapy as the acupuncture group.
The treatments in all three groups were done once every three days, twice a week. Four times made up a course of treatment, and patients were treated for 1-3 courses. Drugs and other therapies were discontinued during this clinical trial.
2.4 Quality control
The quality control of this clinical trial consisted of three stages.
First, physicians from all centers were trained before the clinical trial to minimize errors. The training contents included case selection criteria, grouping, different treatment methods and management of unexpected events.
Second, regular inspection was conducted to each center to make sure the results more objective.
Third, experimental data were recorded and analyzed by different personnel.
3 Treatment Results
3.1 Observation measurements
3.1.1 Pain intensity
As for neck pain, the visual analogue scale (VAS) was used to evaluate the pain intensity[20]. A higher VAS score indicates a more intense pain.
3.1.2 Quality of life
The neck disability index (NDI) was used to evaluate the patients’ functional status[21], which involves two aspects: neck pain and associated symptom; and activities of daily living (ADL)[22]. A higher NDI score indicates a more severe condition.
3.1.3 Associated clinical symptoms
The symptoms, functional status and clinical signs were graded according to the clinical assessment scale (CAS) for cervical spondylosis[23]. A higher CAS score indicates a more severe condition.
3.2 Treatment outcomes
After 1 course of treatment, due to wrong or incomplete information or personal reasons, 33 cases in the bloodletting group, 27 cases in acupuncture group and 32 cases in the combined group were rejected from the trial. After 2 courses of treatment, 6 cases in the bloodletting group, 8 cases in acupuncture group and 7 cases in the combined group dropped out.
Considering the dropouts in all three groups, before the 2nd and 3rd course of treatment, an inter-group comparison on baseline data was conducted. There were no inter-group statistical differences in baseline data (P>0.05), (Table 2 and Table 3).
3.2.1 Inter-group comparison in scores of VAS, NDI and CAS after 1 course of treatment
Before treatment, there were no inter-group statistical significances in comparing the scores of VAS,NDI and CAS (P>0.05), indicating that the three groups were comparable. After 1 course of treatment, there were intra-group statistical significances in VAS, NDI and CAS (P<0.001), indicating that all three therapies can significantly alleviate pain, cervical dysfunction and symptoms due to cervical radiculopathy. However, there were no inter-group statistical significances in comparing scores of VAS, NDI and CAS after 1 course of treatment (P>0.05), indicating that the three therapies have similar effect for cervical radiculopathy-related pain, cervical dysfunction and symptoms after 1 course of treatment (Table 4).
3.2.2 Inter-group comparison in scores of VAS, NDI and CAS after 2 courses of treatment
After 2 courses of treatment, the scores of VAS, NDI and CAS in all three groups showed statistical significances in comparison with the results before treatment and after 1 course of treatment (P<0.001), indicating that the efficacies in all three groups increased with the time of treatment. However, there were no inter-group statistical significances in comparing scores of VAS, NDI and CAS after 2 courses of treatment (P>0.05), indicating that the three therapies had no statistical differences in alleviating pain, cervical dysfunction and symptoms in patients with cervical radiculopathy (Table 5).
3.2.3 Inter-group comparison in scores of VAS, NDI and CAS after 3 courses of treatment
After 3 courses of treatment, the scores of VAS, NDI and CAS in all three groups showed statistical differences compared with the results before treatment, after 1 course of treatment and after 2 courses of treatment (all P<0.001), indicating that all three therapies can significantly alleviate pain, cervical dysfunction and symptoms in patients with cervical radiculopathy, and their efficacies still increase with the time of treatment. However, there were no inter-group statistical significances in comparing scores of VAS, NDI and CAS after 3 courses of treatment (P>0.05), indicating that the three therapies had no statistical differences in alleviating pain, cervical dysfunction and symptoms in patients with cervical radiculopathy (Table 6).
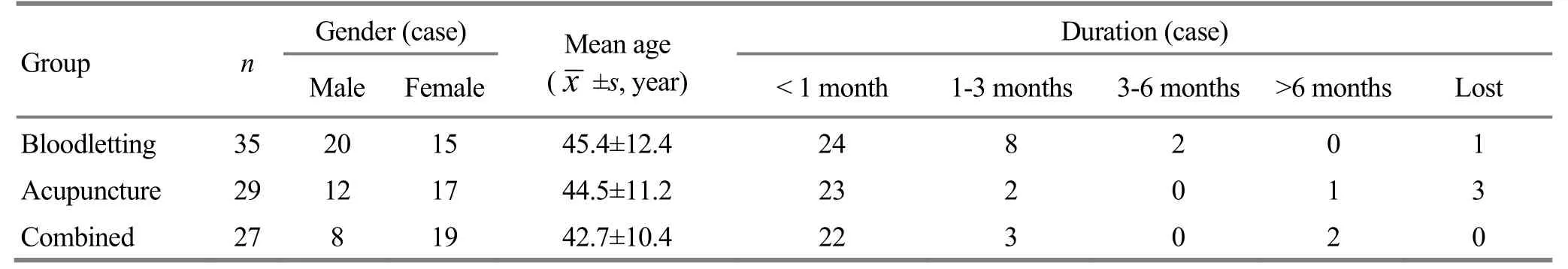
Table 2. Inter-group comparison of baseline data before the second course of treatment
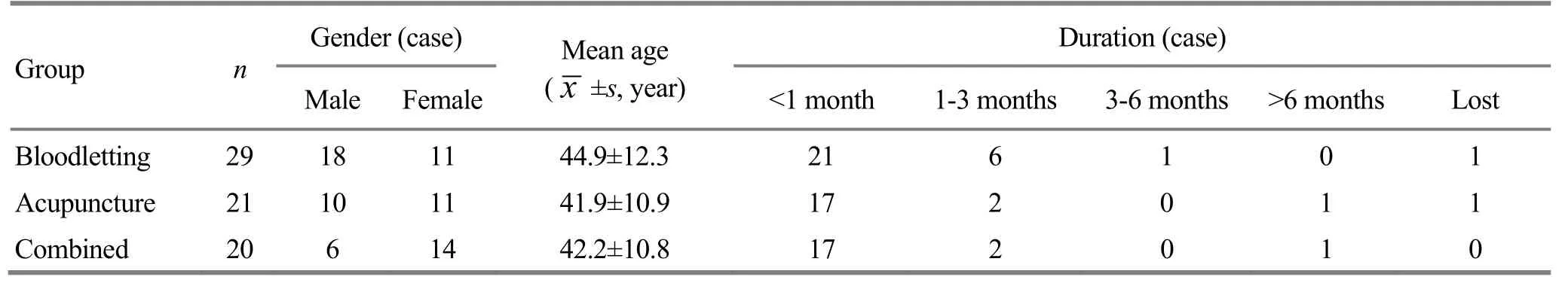
Table 3. Inter-group comparison of baseline data before the third course of treatment
Table 4. Inter-group comparison in scores of VAS, NDI and CAS
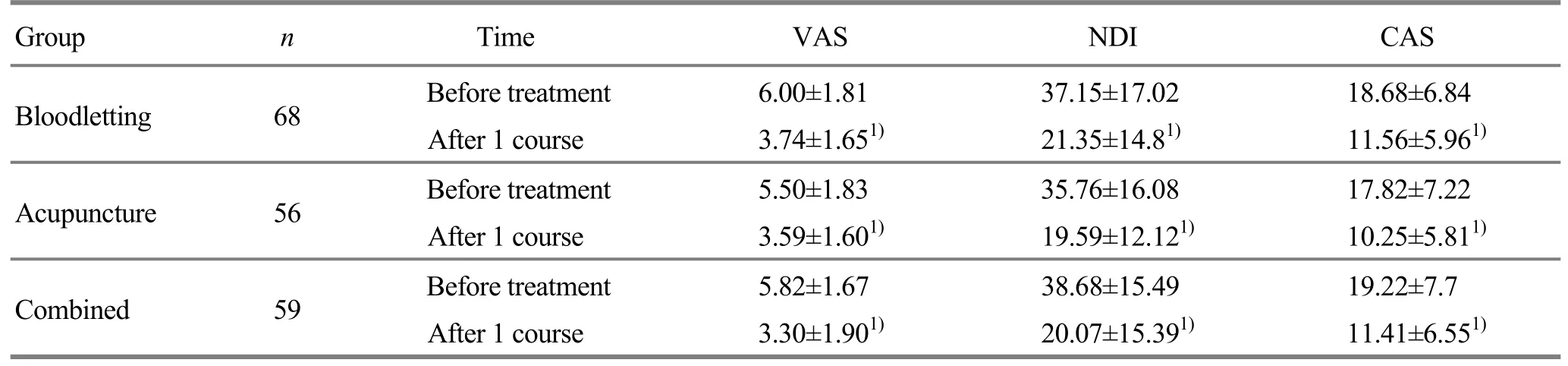
Table 4. Inter-group comparison in scores of VAS, NDI and CAS
Note: Intra-group comparison before and after treatment, 1) P<0.001
Group n Time VAS NDI CAS Bloodletting 68 Before treatment 6.00±1.81 37.15±17.02 18.68±6.84 After 1 course 3.74±1.651) 21.35±14.81) 11.56±5.961)Acupuncture 56 Before treatment 5.50±1.83 35.76±16.08 17.82±7.22 After 1 course 3.59±1.601) 19.59±12.121) 10.25±5.811)Combined 59 Before treatment 5.82±1.67 38.68±15.49 19.22±7.7 After 1 course 3.30±1.901) 20.07±15.391) 11.41±6.551)
Table 5. Inter-group comparison in scores of VAS, NDI and CAS after 2 courses of treatment
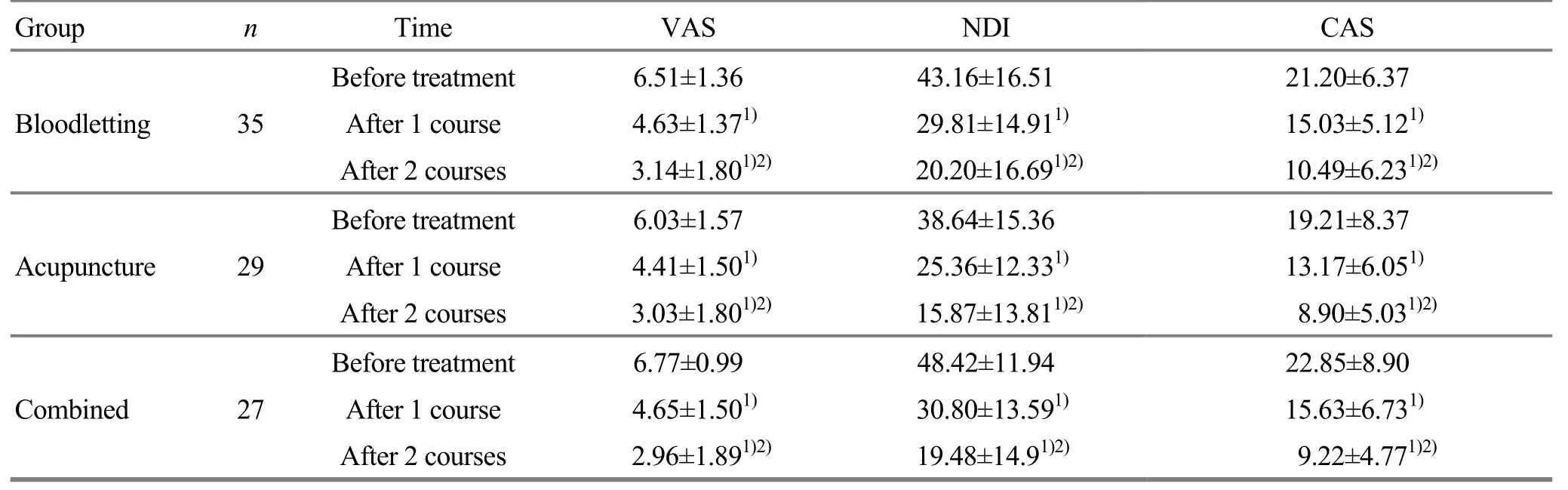
Table 5. Inter-group comparison in scores of VAS, NDI and CAS after 2 courses of treatment
Note: Intra-group comparison before and after treatment, 1) P<0.001; intra-group comparison after 1 course of treatment, 2) P<0.001
Group n Time VAS NDI Before treatment 6.51±1.36 43.16±16.51 Bloodletting 35After 1 course 4.63±1.371) 29.81±14.911)After 2 courses 3.14±1.801)2) 20.20±16.691)2)Before treatment 6.03±1.57 38.64±15.36 Acupuncture 29After 1 course 4.41±1.501) 25.36±12.331)After 2 courses 3.03±1.801)2) 15.87±13.811)2)Before treatment 6.77±0.99 48.42±11.94 Combined 27After 1 course 4.65±1.501) 30.80±13.591)After 2 courses 2.96±1.891)2) 19.48±14.91)2)CAS 21.20±6.37 15.03±5.121)10.49±6.231)2)19.21±8.37 13.17±6.051)8.90±5.031)2)22.85±8.90 15.63±6.731)9.22±4.771)2)

Table 6. Inter-group comparison in scores of VAS, NDI and CAS after 3 courses of treatment [(M (Q), point]
4 Discussion
Cervical radiculopathy accounts for 60%-70% of cervical spondylosis[24]. It often results from degenerated cervical intervertebral disc, hyperplasia of cervical vertebrae and unstable or subluxated cervical joints or ligament irritating or compressing the cervical nerve root[25]. The treatment purpose of this condition is to alleviate symptoms and relieve pain.
Numerous clinical studies have confirmed the exact efficacy of acupuncture for cervical radiculopathy. However, there are fewer reports and only low-level evidence regarding bloodletting therapy for this condition. That’s why we conducted this multi-center, large sample and randomized controlled clinical trial to investigate the effect of bloodletting on pain, cervical dysfunction and clinical symptoms in patients with cervical radiculopathy. In addition, we compared its therapeutic efficacy with that of conventional acupuncture and bloodletting combined with acupuncture. Results of this clinical trial have suggested that bloodletting can alleviate the patients’ pain, cervical dysfunction and other clinical symptoms in a fast and effective way and had no statistical significance compared with acupuncture. What’s more, its efficacy increases with the course of treatment (after 3 courses). However, combining bloodletting and acupuncture did not improve the clinical efficacy.
This trial has confirmed the similar efficacy of bloodletting therapy as acupuncture for cervical radiculopathy. Thanks to its shorter treatment time and fast pain-relief effect, bloodletting can be conveniently done.
Because of errors in data collection in one center (incomplete/absent data, dropout of cases), there might be problems in sample size despite the statistical process. This indicates that quality control is essential to multi-center clinical trials.
In terms of modern medicine, the underlying action mechanism of bloodletting for cervical radiculopathy lies in its role in remarkable improvement in blood perfusion[26]. Studies have suggested that bloodletting therapy can reduce intercellular adhesion molecule 1 (ICAM-1), increase local blood supply, improve inflammatory injury, alleviate pain and benefit deficiency or excess type of cervical spondylosis[27].Further studies on bloodletting need to focus on multiple perspectives of clinical assessment and mechanism study.
Conflict of Interest
There was no conflict of interest in this article.
Acknowledgments
This work was supported by Scientific Research Project of Integrative Chinese and Western Medicine by Tianjin Municipal Health Bureau (天津市卫生局中西医结合科研课题, No.11027).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 21 January 2015/Accepted: 25 February 2015
[1] Ellenberg MR, Honet JC, Treanor WJ. Cervical radiculopathy. Arch Phys Med Rehabil, 1994, 75(3): 342-352.
[2] Corey DL, Comeau D. Cervical radiculopathy. Med Clin North Am, 2014, 98(4): 791-799.
[3] Wainner RS, Gill H. Diagnosis and nonoperative management of cervical radiculopathy. J Orthop Sports Phys Ther, 2010, 30(12): 728-744.
[4] Leonardi M, Boos N. Degenerative disorders of the cervical spine. Spinal Disorders, 2008, (17): 429-479.
[5] van der Velde G, Hogg-Johnson S, Bayoumi AM, Cassidy JD, Côté P, Boyle E, Llewellyn-Thomas H, Chan S, Subrata P, Hoving JL, Hurwitz E, Bombardier C, Krahn M. Identifying the best treatment among common nonsurgical neck pain treatments: a decision analysis. Spine (Phila Pa 1976), 2008, 33(4 Suppl): S184-S191.
[6] Persson LC, Carlsson CA, Carlsson JY. Long-lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar. A prospective, randomized study. Spine (Phila Pa 1976), 1997, 22(7): 751-758.
[7] Borenstein DG. Chronic neck pain: how to approach treatment. Curr Pain Headache Rep, 2007, 11(6): 436-439.
[8] Sundberg T, Petzold M, Wändell P, Rydén A, Falkenberg T. Exploring integrative medicine for back and neck pain: a pragmatic randomised clinical pilot trial. BMC Complement Altern Med, 2009, 9: 33.
[9] Cui XJ, Sun YL, You SF, Mo W, Lu S, Shi Q, Wang YJ. Effects of Qishe Pill, a compound traditional Chinese herbal medicine, on cervical radiculopathy: study protocol for a randomized controlled trial. Trials, 2013, 14: 322.
[10]Liu ZY, Liu BG, Lin X. Kinematic effect of Chinese herbal fomentation on patients with chronic neck pain. Chin J Integr Med, 2014, 20(12): 917-922.
[11]Que QH, Ye XD, Su QG, Yan W, Chu JF, Mei LJ, Huang WW, Lu RH, Zheng GH. Effectiveness of acupuncture intervention for neck pain caused by cervical spondylosis: study protocol for a randomized controlled trial. Trials, 2013, (14): 186.
[12]Wu YC, Zhang JF, Sun YJ. Clinical study on electroacupuncture for cervical intervertebral disc herniation. J Acupunct Tuina Sci, 2013, 11(6): 371-374.
[13] Seo BK, Lee JH, Kim PK, Baek YH, Jo DJ, Lee S. Bee venom acupuncture, NSAIDs or combined treatment for chronic neck pain: study protocol for a randomized, assessor-blind trial. Trials, 2014, 15: 132.
[14]Wang SN, Sheng F, Pan YH. Clinical study on tuina combined with auricular point sticking for cervical radiculopathy. J Acupunct Tuina Sci, 2014, 12(4): 230-235.
[15]Cao HJ, Han M, Li X, Dong SJ, Shang YM, Wang Q, Xu S, Liu JP. Clinical research evidence of cupping therapy in China: a systematic literature review. BMC Complement Altern Med, 2010, 10: 70.
[16]Guo XR. Clinical study advance in acupuncture treatment for cervical radiculopathy. Yatai Chuantong Yiyao, 2015, 11(2): 60-61.
[17]Xu YL, Zhang K, Meng XW. Study on the security of collateral puncture in treating vertebrae disease. Tianjin Zhongyiyao Daxue Xuebao, 2012, 31(2): 114-115.
[18] Chinese Association of Rehabilitation Medicine. Guidelines for Diagnosis, Treatment and Rehabilitation of Cervical Spondylosis. Beijing: Chinese Association of Rehabilitation Medicine, 2010: 1-13.
[19]General Administration of Quality Supervision, Inspection and Quarantine of the People’s Republic of China, Standardization Administration of the People’s Republic of China. Nomenclature and Location of Acupuncture Points (GB/T 12346-2006). Standards Press of China, 2006.
[20] Yan TB. Modern Rehabilitative Therapeutics. Guangzhou: Guangdong Science &Technology Press, 2004: 493.
[21]Wu SL, Ma C, Wu SL, Yan TB. Validity and reliability of the neck disability index for cervical spondylopathy patients. Zhongguo Kangfu Yixue Zazhi, 2008, 23(7): 625-628.
[22]Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther, 1991, 14(7): 409-415.
[23]Zhang MS, Xu WC, Lin ZM, Chen Y. The reliability and validity of a clinical assessment scale for cervical spondylosis. Zhonghua Wuli Yixue Yu Kangfu Zazhi, 2003, 25(3): 151-154.
[24]Qiu XW. Clinical research on acupuncture at cervical Jiaji points for radicular type of cervical spondylosis. Doctor thesis of Guangzhou University of Traditional Chinese Medicine, 2011.
[25]Wang JR, Gong CM, Ma SJ, Xiu JJ, Liu LJ. Mechanism and component analysis of Bi Tong Ling medicated wine for cervical radiculopathy. Zhongguo Zhongyiyao Xiandai Yuancheng Jiaoyu, 2011, 9(2): 98.
[26] Piao SA, Meng XW, Zhu CH, Liu HP, Li DD. Effect of bloodletting therapy on local blood perfusion in patients with cervical radiculopathy. Tianjin Zhongyiyao, 2014, 31(11): 656-659.
[27]Chen XK, Li LP, Wu H, Li G, Cai WH. Study of the influence of pricking bloodletting method on intracellular adhesion molecule-1 in the treatment of cervical spondylosis. Shanghai Zhenjiu Zazhi, 2010, 29(1): 25-27.
Translator:Han Chou-ping (韩丑萍)
刺络疗法治疗神经根型颈椎病的疗效观察
目的:观察刺络疗法治疗神经根型颈椎病(cervical spondylotic radiculopathy, CSR)的有效性及安全性。方法:采用五个中心、随机、对照的方法, 将183名符合纳入标准的受试者按随机数字表分为刺络组(68例)、针刺组(56例)及刺络加针刺组(59例)。刺络组患者接受在大椎、患侧肩井刺络放血并拔火罐治疗, 留罐5-10 min, 出血量每罐5 mL, 共2-3罐。针刺组患者接受在双侧C3-7夹脊穴、患侧肩井针刺治疗, 留针30 min。刺络加针刺组患者接受与刺络组相同的刺络治疗和与针刺组相同的针刺治疗。三组均3日治疗1次,每星期治疗2次, 治疗4星期为1疗程, 治疗1-3疗程。采用视觉模拟量表(visual analogue scale, VAS)、颈部功能障碍指数(neck disability index, NDI)和临床评价量表(clinical assessment scale, CAS)评分于治疗前及治疗1、2、3疗程后, 对各组进行疗效评价。结果:三组治疗1、2、3个疗程后VAS、NDI、CAS评分均较本组治疗前有明显下降(均P<0.001), 三组组间VAS、NDI及CAS评分比较, 无统计学差异(均P>0.05)。结论:刺络疗法治疗CSR可有效缓解患者疼痛并改善其生活质量, 与针刺疗法具有同样治疗作用。
针刺疗法; 刺络拔罐疗法; 颈痛; 椎关节强硬; 颈椎病; 随机对照临床试验
R246.2 【
】A
Author: Mou Ming-yuan, master degree candidate
Meng Xiang-wen, associated professor.
E-mail: mengxiangwen@139.com
Methods:The randomized controlled clinical trial was conducted in five centers. A total of 183 eligible subjects were randomly allocated into a bloodletting group (n=68), an acupuncture group (n=56) and a combined group (n=59). Patients in the bloodletting group were treated with bloodletting at Dazhui (GV 14) and Jianjing (GB 21) on the affected side, coupled with 5-10 min of cupping, 5 mL blood for each cup, 2-3 cups for one treatment. Patients in the acupuncture group were treated with needling cervical Jiaji (EX-B 2) points and Jianjing (GB 21) on the affected side. The needles were retained for 30 min. Patients in the combined group were treated with both methods. The treatment in all three groups were done once every three days, twice a week, 4 weeks for a course of treatment, for a total of 1-3 courses. Then the therapeutic efficacy was evaluated using scores of visual analogue scale (VAS), neck disability index (NDL) and clinical assessment scale (CAS) before treatment and after 1, 2 and 3 courses of treatment.
Results:The scores of VAS, NDI and CAS in all three groups were significantly decreased after 1, 2 and 3 courses of treatment (allP<0.001), and there were no inter-group statistical significances in comparing scores of VAS, NDI and CAS (allP>0.05).
Conclusion:Bloodletting and cupping share the similar effect with acupuncture in pain relief and improvement of quality of life in patients with cervical radiculopathy.
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture at Chize (LU 5) versus Shangjuxu (ST 37) in rats with ulcerative colitis
- Professor Yan Jun-bai’s experience in treating rheumatic arthritis with suppurative moxibustion
- Clinical observation on Nie-pinching spine manipulation combined with point therapy for cerebral palsy in children with spleen deficiency
- Observation on clinical effect of auricular acupoint sticking plus music therapy for post-stroke insomnia
- Clinical observation on acupuncture plus tuina for insomnia
- Observation on clinical effects of herbal cake-partitioned moxibustion for knee osteoarthritis
