Therapeutic efficacy observation on electroacupuncture for Alzheimer’s disease
2015-05-18PengJing彭静LuoLiang罗亮XuLi徐丽ChenXi陈曦
Peng Jing (彭静), Luo Liang (罗亮), Xu Li (徐丽), Chen Xi (陈曦)
1 Rehabilitation Office, Nursing Department, Leshan Vocational & Technical College, Sichuan 614000, China
2 Acupuncture & Rehabilitation Department, Leshan Hospital of Traditional Chinese Medicine, Sichuan 614000, China
3 Leshan Geriatric Hospital, Sichuan 614000, China
4 Leshan Shizhong District People’s Hospital, Sichuan 614000, China
Therapeutic efficacy observation on electroacupuncture for Alzheimer’s disease
Peng Jing (彭静)1, Luo Liang (罗亮)2, Xu Li (徐丽)3, Chen Xi (陈曦)4
1 Rehabilitation Office, Nursing Department, Leshan Vocational & Technical College, Sichuan 614000, China
2 Acupuncture & Rehabilitation Department, Leshan Hospital of Traditional Chinese Medicine, Sichuan 614000, China
3 Leshan Geriatric Hospital, Sichuan 614000, China
4 Leshan Shizhong District People’s Hospital, Sichuan 614000, China
Objective:To observe the effect of electroacupuncture (EA) for Alzheimer’s disease (AD).
Acupuncture Therapy; Electroacupuncture; Alzheimer Disease; Cognition Disorders; Activities of Daily Living; Neuropsychology
Alzheimer’s disease (AD) is the most common pattern of senile dementia. It is a chronic neurodegenerative disease[1]that usually starts slowly and gets worse over time. Common symptoms include decline in progressive learning and memory, cognitive impairment and personality change. Along with the aging population, the incidence of AD increases year by year. Studies have indicated that AD affects over 20% of people aged over 80 years. The early stage pathological process of AD may take decades. At present, there are no treatments that can stop or reverse its progression upon the presence of clinical symptoms[2-3]. There are no specific drugs yet for AD. As a result, it’s of great significance to come up with effective intervention protocol for AD. We treated 30 AD cases with electroacupuncture (EA) and evaluated their efficacies using mini-mental state examination (MMSE), revised Hasegawa dementia scale (HDS-R), activities of daily living (ADL) and neurological function defect scale (NFDS). The results are now summarized as follows.
1 Clinical Data
1.1 Diagnostic criteria
This was based on the diagnostic criteria for AD in theDiagnostic and Statistical Manual of Mental Disorders-IV-Text Revision (DSM-IV-TR) by the American Psychiatric Association (APA)[4]. Presence of multiple cognitive defects, manifesting as memory decline (difficulty in learning new knowledge or unable to recall the previous knowledge) and at least one of the following cognitive defects: aphasia, apraxia, agnosia or disturbed executive function (planning, organizing, sequencing or abstracting); social or occupational impairment that declined from previous level; insidious onset with slow continuing deterioration; absence of other central nervous disorders that can affect memory and cognition (such as cerebrovascular diseases, Parkinson’s disease, Huntington’s disease, subdural haematoma, normal pressure hydrocephalus, and brain tumor, etc.); absence of clinical evidence to suggest that the mental state may be due to other systemic or brain disease which can induce a dementia (such as hypothyroidism, vitamin B1or B12deficiency, niacin deficiency, hypocalcemia, neurosyphilis, and HIV infection, etc.).
1.2 Inclusion criteria
Those who met the above diagnostic criteria; aged over 60 years; the legal guardian agreed to accept the intervention protocol and comply with the follow-up; willingly signed the informed consent.
1.3 Exclusion criteria
Those who didn’t meet the above diagnostic or inclusion criteria; having complications of severe liver, kidney or heart insufficiency; having complications of severe neurological deficit symptoms; having a family history; having cognitive impairment due to delirium or other mental disorders (such as major depression and schizophrenia); and individuals whose condition was too severe for safety and efficacy evaluation of EA.
1.4 Statistical management
The SPSS 19.0 version software was used for statistical analysis. Thet-test was used for measurement data, which was expressed in the form ofAPvalue of less than 0.05 indicates a statistical significance.
1.5 General materials
A total of 30 eligible (13 males and 17 females) AD cases from Leshan Hospital of Traditional Chinese Medicine, Leshan Geriatric Hospital and Leshan Shizhong District People’s Hospital were included between January 2014 and October 2014. These cases were aged between 60 and 85 years, with a mean age of (73.3±6.7) years. Their duration lasted between 2 and 9 years, with an average duration of (5.1 ±2.5) years.
2 Treatment Methods
2.1 Treatment devices
Disposable filiform needles (manufactured by Suzhou Medical Device Factory Ltd., China) of 0.25 mm in diameter and 25 mm or 40 mm in length; and Xinsheng Brand G6805-II electric stimulator (Qingdao, China).
2.2 Points
Shenting (GV 24), Baihui (GV 20), Dazhui (GV14), Fengfu (GV 16), Mingmen (GV 4) and bilateral Yongquan (KI 1).
2.3 Method
The patient took a sitting position. After routine sterilization using 75% medical alcohol, Shenting (GV 24), Baihui (GV 20), Dazhui (GV 14), Fengfu (GV 16) and Mingmen (GV 4) were punctured 0.5 cun obliquely towards the pathway of the Governor Vessel; and Yongquan (KI 1) on both sides were punctured 0.5-0.8 cun perpendicularly. An even reinforcing-reducing manipulation was applied to each point upon arrival of qi. Then the G6805-II electric stimulator was connected respectively to Shenting (GV 24) and Baihui (GV 20), to Dazhui (GV 14) and Fengfu (GV 16) and to bilateral Yongquan (KI 1), using continuous wave at the frequency of 2-100 Hz and the voltage of 2-4 V. With a tolerable intensity, each treatment lasted 25 min. The treatment was conducted once a day for 10 d as a course. There was a 3-day interval between two courses. The therapeutic efficacies were observed after three courses.
3 Therapeutic Efficacy Evaluation
3.1 Measurement items and methods
The intelligence and neurologic functions were graded and scored before and after treatment.
3.1.1 MMSE
The MMSE contains 30 items and has a maximum score of 30 points involving the patient’s orientation, recall, calculation and language.
Dementia criteria by MMSE score: MMSE ≤17 points for illiterate; MMSE ≤20 points for elementary school intelligence; MMSE ≤22 points for middle school (including secondary school) intelligence; and MMSE ≤23 points for college education (including junior college) intelligence.
Dementia severity by MMSE score: MMSE ≥21 points for mild; MMSE ≥10 points, but ≤20 points for moderate; and MMSE ≤9 points for severe.
3.1.2 HDS-R
The HDS-R was used to assess patients’ cognition changes before and after treatment. It has a maximum score of 30 points. Dementia is defined when the HDS-R is less than 21 points (above primary school education).
3.1.3 ADL
The ADL contains 14 items, 6 physical selfmaintenance scales (PSMS), 8 instrumental activities of daily living (IADL) and a maximum score of 64 points. A total score of <16 points indicates completely normal, whereas a score of >16 points indicates impaired ADL. For single item, 1 point indicates normal, 2-4 points indicate functional decline. A score of ≥3 points for two or more items or a total score of ≥22 points indicates marked impairment in ADL.
3.1.4 NFDS
The NFDS score ranged from 0 to 45 points. 0-15 points for mild neurological deficit; 16-30 points for moderate neurological deficit; and 31-45 points for severe neurological deficit.
3.2 Results
3.2.1 Changes in MMSE and HDS-R scores
After treatment, both MMSE and HDS-R scores were significantly increased (P<0.01), indicating that EA can increase patients’ MMSE and HDS-R scores and alleviate their cognitive impairment (Table 1).
Table 1. Changes in MMSE and HDS-R scores before and after EA treatment
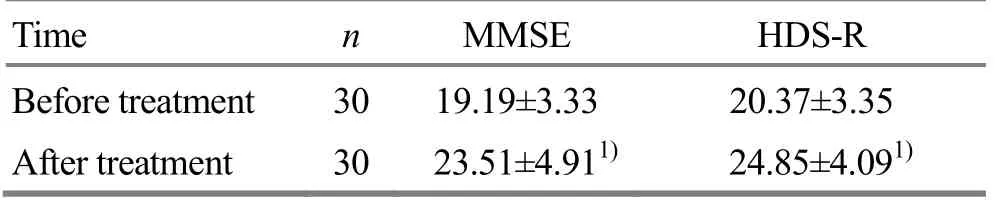
Table 1. Changes in MMSE and HDS-R scores before and after EA treatment
Note: Compared with the result of before treatment, 1) P<0.01
Time n MMSE HDS-R Before treatment 30 19.19±3.33 20.37±3.35 After treatment 30 23.51±4.911) 24.85±4.091)
3.2.2 Changes in ADL and NFDS scores
After treatment, both ADL and NFDS scores were significantly decreased (P<0.01), indicating that EA can improve patients’ ADL and alleviate their symptoms of neurological deficits (Table 2).
Table 2.Changes in ADL and NFDS scores before and after EA treatment

Table 2.Changes in ADL and NFDS scores before and after EA treatment
Note: Compared with pre-treatment results, 1) P<0.01
Time n ADL NFDS Before treatment 30 41.19±3.68 17.65±3.86 After treatment 30 36.13±3.261) 13.39±3.021)
4 Discussion
Considering from AD symptoms such as decline in intelligence, learning, memory and ADL, social impairment and personality change, it falls under the category of ‘dementia’ or ‘forgetfulness’ in Chinese medicine. Physicians of different generations believe this condition is closely associated with the heart, brain and kidney[5]. Kidney yang deficiency can result in failure of clean yang qi to ascend to the brain. Obstruction of the Governor Vessel can result in failure of essential qi of Zang-fu organs to ascend to nourish the brain. As a result, kidney deficiency and obstruction of meridians are key factors contributing to AD[6]. The treatment strategy in this study was therefore to tonify kidney, unblock the Governor Vessel and refresh the mind.
Of points selected in this study, Baihui (GV 20) is a crossing point between the Governor Vessel with the Bladder, Small Intestine, Gallbladder and Liver Meridians; Shenting (GV 24) is a crossing point between the Governor Vessel with Bladder and Stomach Meridians. These are two essential points for mental problems. Dazhui (GV 14) is a crossing point between the Governor Vessel and six yang meridians. Dazhui (GV 14) and Mingmen (GV 4) are two essential points to strengthen the body. Fengfu (GV 16) is a crossing point between the Governor Vessel with Bladder Meridian and Yang Link Vessel. It is a key point to remove wind and refresh the mind. Yongquan (KI 1) is the Jing-Well point of Kidney Meridian. Needling this point can tonify kidney yang and benefit intelligence.
This study employed four neuropsychological scales including MMSE[7], HDS-R[8], ADL[9]and NFDS[10]for comprehensive objective efficacy evaluation from overall intelligence, orientation, memory, calculation, language, ADL and cognition.
Research results have suggested that EA can increase the MMSE and HDS-R scores and decrease the ADL and NFDS scores in AD patients, indicating that this treatment protocol can effectively improve patients’orientation, memory, calculation, language, ADL and neurological deficits, stop or delay AD progression. It’s therefore worthy of clinical application.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by the Scientific Research Project of Leshan Vocational & Technical College, Sichuan Province (四川省乐山职业技术学院科研项目, No. KY2014012).
Statement of Informed Consent
The informed consent was obtained from all individual participants included in this study.
Received: 15 December 2014/Accepted: 18 January 2015
[1] Ma HJ, Tang N, Li YY, Cao CD, Yi ZX, Zhang WN. Advance in acupuncture for senile dementia. Guangxi Zhongyi Xueyuan Xuebao, 2012, 15(2): 84-86.
[2] Deng HM, Xiao F, Yang L, Zhu MM, Huang F. Research overview on inflammation mechanism and related drugs for Alzheimer’s disease. Guangdong Yixue, 2010, 31(16): 2170-2172.
[3] Small GW, Rabins PV, Barry PP, Buckholtz NS, DeKosky ST, Ferris SH, Finkel SI, Gwyther LP, Khachaturian ZS, Lebowitz BD, McRae TD, Morris JC, Oakley F, Schneider LS, Streim JE, Sunderland T, Teri LA, Tune LE. Diagnosis and treatment of Alzheimer disease and related disorders. Consensus statement of the American Association for Geriatric Psychiatry, the Alzheimer's Association, and the American Geriatrics Society. JAMA, 1997, 278(16): 1363-1371.
[4] Division of Mental Health General. International Classification of Diseases. 10th Revision. World Health Organization, 1989: 60-68.
[5] Zhou CX, Hu YS, Cui X, Ni HH, Wu J, Shi JC. Observation on therapeutic effect of acupuncture combined with herbal medicine and cognitive training on mild cognitive impairment in patients with post-stroke. Zhenjiu Linchuang Zazhi, 2012, 28(8): 1-4.
[6] Zhao L, Zhang FW, Zhang H, Luo C, Zhu MJ, Xiao XQ, Yu X, Li H, Zheng LQ. Therapeutic efficacy observation on electroacupuncture of dredging the Governor Vessel and regulating brain for cognitive function in patients with mild cognitive impairment. Zhongguo Laonian Yixue Zazhi, 2010, 30(10): 1321-1323.
[7] Zhang MY. Psychiatry Assessment Scale Manual. Changsha: Hunan Science & Technology Press, 2003: 154-159.
[8] Tang CM. Neuropsychology. Beijing: People’s Military Medical Press, 2001: 343-344.
[9] Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist, 1969, 9(3): 179-186.
[10]Sukoff MH. Effects of hyperbaric oxygenation. J Neurosurg, 2001, 95 (3): 544-546.
Translator:Han Chou-ping (韩丑萍)
电针治疗阿尔茨海默病疗效观察
目的: 观察电针治疗阿尔茨海默病(Alzheimer’s disease, AD)的疗效。方法: 共纳入30例患者, 予以针刺神庭、百会、大椎、风府、命门和涌泉治疗。得气后, 神庭、百会为一组, 大椎、风府为一组, 双侧涌泉为一组,连接 G6805-Ⅱ型电针治疗仪, 施以连续波, 频率 2-100 Hz, 电压 2-4 V, 刺激量以患者能够耐受为度, 每次刺激25 min, 每日1次, 连续10次为1疗程, 疗程间间隔3天, 治疗3个疗程后用简易精神状态检查量表(mini-mental state examination, MMSE)、修订后的长谷川智能量表(revised Hasegawa dementia scale, HDS-R)、日常生活能力(activities of daily living, ADL)量表、临床神经功能缺损量表(neurological function defect scale, NFDS)评价疗效。结果:电针治疗后MMSE和HDS-R评分较治疗前有显著升高(P<0.01); ADL和NFDS评分较治疗前有显著下降(P<0.01)。结论: 电针是治疗AD的有效方法, 能有效提高AD患者总体智能和修复神经功能缺损。
针刺疗法; 电针; 阿尔茨海默病; 认知障碍; 日常生活活动; 神经心理学
R246.6 【
】A
Author: Peng Jing, lecturer, attending physician.
E-mail: pengjing1983@sina.com
Methods:A total of 30 eligible cases were treated by needling Shenting (GV 24), Baihui (GV 20), Dazhui (GV 14), Fengfu (GV 16), Mingmen (GV 1) and Yongquan (KI 1). Upon arrival of qi, the G6805-II electric stimulator was connected to Shenting (GV 24) and Baihui (GV 20) (one pair), to Dazhui (GV 14) and Fengfu (GV 16) (one pair) and to bilateral Yongquan (KI 1) (one pair) for 25 min, using continuous wave at the frequency of 2-100 Hz and voltage of 2-4 V. With a tolerable intensity, the EA was conducted once a day for 10 d (one treatment course). There was a 3-day interval between two courses. After three courses, the therapeutic efficacies were evaluated using the mini-mental state examination (MMSE), revised Hasegawa dementia scale (HDS-R), activities of daily living (ADL) and neurological function defect scale (NFDS).
Results:After EA treatment, the MMSE and HDS-R scores were significantly increased (P<0.01) and the ADL and NFDS scores were significantly decreased (P<0.01).
Conclusion:EA is effective for AD and can improve the overall intelligence and repair neurologic deficits in AD patients.
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Efficacy observation on acupuncture-moxibustion for urinary retention after surgery for cervical cancer
- Therapeutic observation of acupuncture plus heat-sensitive moxibustion for chronic pelvic inflammatory disease
- A controlled study on treatment of acute lumbar sprain by acupuncture at Yaotongdian (EX-UE 7) plus tuina manipulation
- Effect of complex reinforcing-reducing manipulation on lower limb motion and balance disorder in patients with subacute combined degeneration of the spinal cord
- Clinical study on skin needling plus heat-sensitive moxibustion for chronic facial paralysis
- Effect of tuina manipulations on blood pressure and its variability in hypertension patients
