不同Wagner分级糖尿病足患者肾损害的临床研究
2015-04-21王佳佳陆祖谦
丁 维,王佳佳,陆祖谦,2*
不同Wagner分级糖尿病足患者肾损害的临床研究
丁 维1,王佳佳1,陆祖谦1,2*
(1安徽医科大学306医院临床学院内分泌科,合肥 230032;2解放军第306医院内分泌科及全军糖尿病诊治中心,北京 100101)
探讨不同严重程度的糖尿病足(Wagner 1~5级)患者的肾损害情况,了解糖尿病足与肾病之间的临床关系,提高临床实践中对糖尿病足的诊治。对解放军第306医院内分泌科2009年6月至2014年6月收治的622例2型糖尿病合并糖尿病足的患者及215例2型糖尿病非足病的患者作回顾性分析,将足病与非足病各分为一组,收集相关临床资料并检测相关生化指标分析糖尿病足的影响因素。将非足病、Wagner 1级、2级、3级各分为一组,Wagner 4级和5级分为一组,以尿白蛋白肌酐比值(UACR)、估算的肾小球滤过率(eGFR)为指标分析不同程度足病的肾损害情况。应用SPSS19.0统计软件进行统计学分析。糖尿病足病组与非足病组相比UACR明显升高,(78.0010.60mg/g,<0.05),eGFR明显下降[(100.91±44.98)(114.27±35.88)ml/(min·1.73m2),<0.05];多元逐步回归分析结果显示性别、糖尿病视网膜病变、血清白蛋白、尿酸、餐后2h血糖、UACR与2型糖尿病足发生、发展相关(β=0.707、0.850、-0.183、-0.006、0.104、0.003,均<0.05);Wagner 3级组与Wagner 2级组相比微量白蛋白尿(UACR 30~300mg/g)发生率明显升高 [49.7%(87/175)39.2%(67/171),2=3.885],Wagner 4~5级组与Wagner 3级组相比肾功能不全[eGFR<60ml/(min·1.73m2)]的发生率明显升高 [23.5%(43/183)11.0%(24/220),2=11.421],差异均有统计学意义(均<0.05);大量白蛋白尿(UACR≥300mg/g)、肾功能不全在Wagner 3级组的发生率低于2级组,但在Wagner 4~5级组重新升高。糖尿病足Wagner分级越高,肾损害越严重,微量白蛋白尿较肾小球滤过率能更早提示糖尿病肾损害,Wagner 3级是肾病进展及临床治疗的转折点,当患者处于Wagner 3级时应加强足部护理及肾脏保护的力度。
糖尿病,2型;糖尿病足;肾损害;尿白蛋白肌酐比值;估算的肾小球滤过率
糖尿病足(diabetic foot,DF)为2型糖尿病(type 2 diabetes mellitus,T2DM)患者较严重的慢性并发症,是导致非创伤性截肢及死亡的主要原因,已报道糖尿病患者截肢的风险要比非糖尿病患者高15~20倍[1],约25%的糖尿病患者会发生足病溃疡[2],15%糖尿病患者需截肢[3]。在合并慢性肾脏疾病(chronic kidney disease,CKD)的糖尿病患者中,DF的发病率更高,截肢率和死亡率也更高[4]。资料显示,肾脏透析是独立于糖尿病周围神经病变、血管病变及感染外的足部溃疡预测因子[5],Wolf等[6]的研究资料显示,DF与肾脏功能关系密切,但是尚不清楚不同Wagner分级的DF患者的肾损害情况。因此,该研究应用估算的肾小球滤过率(estimated glomerular filtration rate,eGFR)和尿白蛋白肌酐比值(urinary albumin to creatinine ratio,UACR)对不同Wagner分级的DF患者的肾损害情况进行回顾性分析,了解DF发展过程中肾脏损害的变化情况,以指导DF的临床诊治。
1 对象与方法
1.1 研究对象
选择2009年6月至2014年6月在解放军第306医院内分泌科住院的T2DM合并DF的患者662例,其中男性432例(65.3%),女性230例(34.7%),年龄(63.11±12.02)岁,病程(12.96±7.77)年;随机选取T2DM非足病(non-diabetic foot,NDF)患者215例,其中男性118例(54.9%),女性97例(45.1%),年龄(60.85±12.81)岁,病程(11.15±7.20)年。纳入标准:(1)按照1999年世界卫生组织(World Health Organization,WHO)糖尿病标准诊断T2DM;(2)DF的诊断标准参照1999年国际DF工作组(International Diabetic Foot,IDF)的定义,按Wagner诊断进行分级;(3)按照美国糖尿病协会(American Diabetic Association,ADA;2007)关于微量白蛋白尿(microalbuminuria,MAU)诊断,采用测定即时尿标本的UACR,UACR<30mg/g、30~299mg/g、≥300mg/g分别为正常、微量白蛋白尿和大量白蛋白尿;(4)根据2001年肾脏病预后质量指南(Kidney Disease Outcome Quality Initiative,K/DOQⅠ)将CKD进行分期,以GFR为标准,分为肾功能正常(GFR>90ml/min)、肾功能下降(60ml/min<GFR<90ml/min)和肾功能不全(GFR<60ml/min)。内生肌酐清除率(creatinine clearance rate,Ccr)是反映GFR的重要指标,Ccr计算法采用肾脏病膳食改良(Modification of Diet in Renal Disease,MDRD)公式,即eGFR[ml/(min·1.73m2)]=0.742(女性)×186×SCr(mg/dl)-1.154×年龄(岁)-0.203。排除标准:排除1型糖尿病和其他继发性糖尿病,紫癜性肾炎、风湿性疾病的肾脏损害、慢性肾小球肾炎合并慢性肾功能不全、用利福平(rifampicin)后发生急性肾衰竭、甘露醇(mannitol)致渗透性肾病合并急性肾衰竭者。
1.2 研究方法
1.2.1 临床资料采集 按标准方法测量血压、身高、体质量,计算体质量指数(body mass index,BMI),并记录糖尿病肾病(diabetic nephropathy,DN)和糖尿病视网膜病变(diabetic retinopathy,DR)病史。
1.2.2 实验室检查 空腹血糖(fasting plasma glucose,FPG)及餐后2h血糖(2-hour postprandial plasma glucose,2hPPG)采用美国强生血糖仪测定。自动生化仪酶法检测血清总蛋白(total protein,TP)、白蛋白(albumin,Alb)、糖化血红蛋白(glycosylated hemoglobin A1c,HbA1c)、尿素氮(blood urea nitrogen,BUN)、血肌酐(serum creatinine,SCr)、尿酸(uric acid,UA)、总胆固醇(total cholesterol,TC)、甘油三酯(triglycerides,TG)和高密度脂蛋白胆固醇(high-density lipoprotein cholesterol,HDL-C)、低密度脂蛋白胆固醇(low-density lipoprotein cholesterol,LDL-C),UACR采用放射免疫法测定。
1.3 统计学处理
2 结 果
2.1 DF组患者与NDF组患者临床特征
DF组患者的年龄、男性所占比例、病程、收缩压、SCr、UACR均较NDF组显著升高,差异均有统计学意义(<0.05);在DF组患者中,DN和DR的发生率较NDF组患者明显升高,差异有统计学意义(<0.05);营养学指标:TP、Alb、UA、TC、TG、HDL-C、LDL-C,DF组均较NDF组降低,差异均有统计学意义(<0.05);在DF组中,2hPPG、eGFR较NDF组降低,差异有统计学意义(<0.05);两组患者的舒张压、FPG、HbAlc、BUN的差异无统计学意义(>0.05;表1)。
2.2 DF的影响因素
以糖尿病患者是否合并足病(0=无足病,1=有足病)为应变量,对表1所有指标行相关分析,结果显示,性别、年龄、糖尿病病程、BMI、收缩压、DN、DR、Alb、SCr、UA、TC、2hPPG、UACR、eGFR与2型糖尿病足相关,将所得相关项为自变量作多元逐步回归分析。结果显示,性别、DR、Alb、UA、2hPPG、UACR影响2型糖尿病足发生、发展(表2)。
2.3 DF组和NDF组患者不同UACR和eGFR发生率比较
校正年龄、收缩压等混杂因素,Wagner分级与UACR和eGFR密切相关。NDF和不同Wagner分级DF患者的正常白蛋白尿发生率分别为73.8%(144/195)、47.8%(22/46;Wagner 1)、34.5%(59/171;Wagner 2)、28.0%(49/175;Wagner 3)、23.0%(31/135;Wagner 4和5);微量白蛋白尿发生率分别为21.0%(41/195)、32.6%(15/46;Wagner 1)、39.2%(67/171;Wagner 2)、49.7%(87/175;Wagner 3)、45.2%(61/135;Wagner 4和5),Wagner 3级组与Wagner 2级组相比,微量白蛋白尿发生率明显升高[49.7%(87/175)39.2%(67/171),2=3.885,<0.05];大量白蛋白尿的发生率分别为5.2%(10/195)、19.6%(9/46;Wagner 1)、26.3%(45/171;Wagner 2)、22.3%(39/175;Wagner 3)、31.8%(43/135;Wagner 4和5),大量白蛋白尿在Wagner 3级组的发生率低于2级组,但在Wagner 4~5级组重新升高。
NDF组和不同Wagner分级DF组患者的肾功能正常的发生率分别为75.8%(150/198)、64.2%(34/53;Wagner 1)、55.1%(108/196;Wagner 2)、59.5%(131/220;Wagner 3)、54.1%(99/183;Wagner 4和5);肾功能下降的发生率分别为18.7%(37/198)、22.6%(12/53;Wagner 1)、32.1%(63/196;Wagner 2)、29.5%(65/220;Wagner 3)、22.4%(41/183;Wagner 4和5);肾功能不全的发生率分别为5.5%(11/198)、13.2%(7/53;Wagner 1)、12.8%(25/196;Wagner 2)、11.0%(24/220;Wagner 3)、23.5%(43/183;Wagner 4和5),Wagner 4和5级组与Wagner 3级组相比,肾功能不全的发生率明显升高[23.5%(43/183)11.0%(24/220),2=11.421,<0.05],肾功能不全在Wagner 3级组的发生率低于2级组,但在Wagner 4~5级组重新升高。
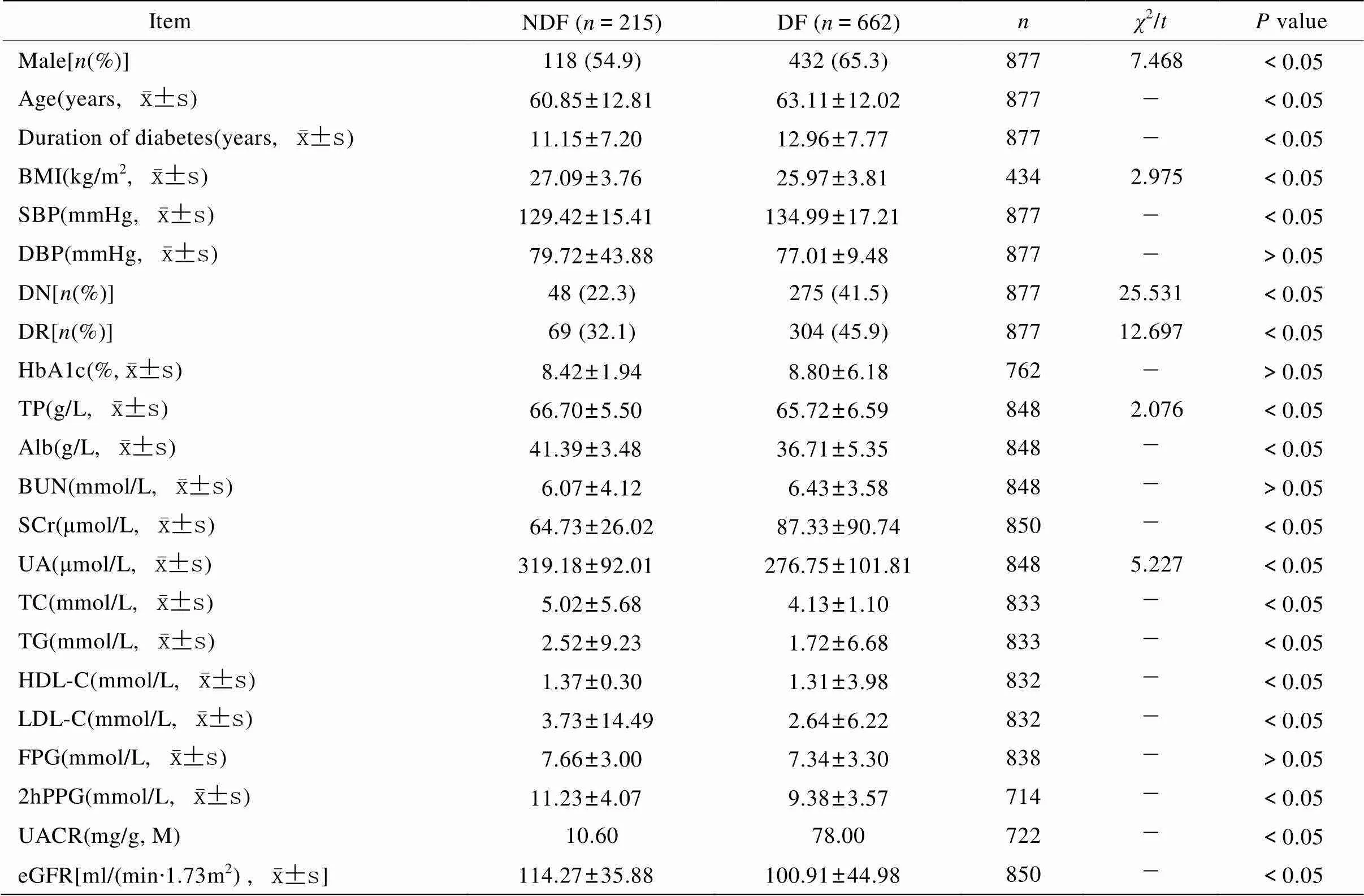
表1 NDF组与DF组一般临床资料比较
NDF: non-diabetic foot; DF: diabetic foot; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; DN: diabetic nephropathy; DR: diabetic retinopathy;HbA1c: glycosylated hemoglobin A1c; TP: total protein; Alb: albumin; BUN: blood urea nitrogen; SCr: serum creatinine; UA: uric acid; TC: total cholesterol; TG: triglycerides; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; FPG: fasting plasma glucose; 2hPPG: 2-hour postprandial plasma glucose; UACR: urinary albumin to creatinine ratio; eGFR: estimated glomerular filtration rate. 1mmHg=0.133kPa
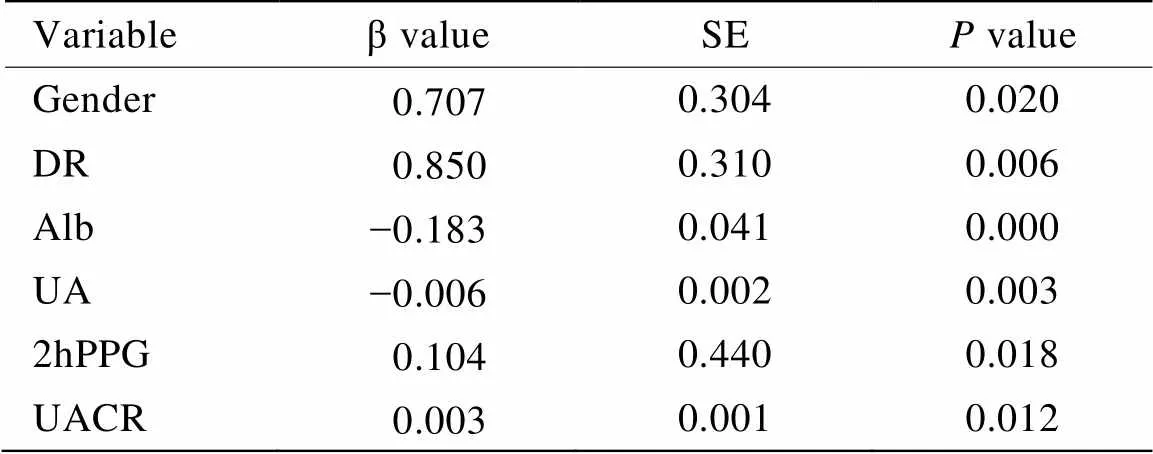
表2 多元逐步回归分析结果
DR: diabetic retinopathy; Alb: albumin; UA: uric acid; 2hPPG: 2-hour postprandial plasma glucose; UACR: urinary albumin to creatinine ratio
3 讨 论
DF占非外伤性下肢截肢的70%~85%[7],已成为全球性医疗护理难题。研究显示,CKD是DF发展的独立危险因素[8]。而慢性DF可以通过增加循环中炎症细胞因子如白细胞介素−6、肿瘤坏死因子−α[9],或反复发作败血症引起急性肾损伤(acute kidney injury,AKI)[10],或两者兼有对肾脏造成损害,故两者关系密切,互相影响[11]。目前尚不清楚在DF患者中,基于Wagner分级不同的DF患者肾损害的程度及其发生率。
蛋白尿的程度与肾小球硬化和肾小管间质纤维化进展密切相关[12]。然而MAU不能提示早期肾病的肾小球功能[13],GFR可提示肾小球滤过和肾小管重吸收功能。研究资料显示,GFR每10ml/min变化是DF的独立预测因子。故在探讨DF肾损害情况时对MAU和GFR均需要进行分析。UACR与尿白蛋白排泄率(urinary albumin excretion rate,UAER)有较好的相关性、一致性和较小的误差,并且较UAER检测简单、快捷,故本研究以UACR作为MAU的诊断指标[14]。本研究采用MDRD校正公式计算得出的eGFR来评估GFR。
本研究结果显示,随Wagner分级越高,正常UACR和正常eGFR的发生率大体趋势逐渐下降,提示随Wagner分级越高,肾损害越严重;Wagner 3级组MAU的发生率较Wagner 2级组明显升高,Wagner 3级组肾功能不全发生率较Wagner 2级组无升高直到Wagner 4~5级组才明显升高,提示MAU出现明显异常的病程阶段较GFR早,MAU较GFR更早提示糖尿病引起的肾损害;大量白蛋白尿、肾功能不全在Wagner 3级组的发生率低于2级组,分析原因一方面可能为Wagner 2级溃疡伤口较轻,机体有更好的组织储备(即神经体液反应、营养物质代谢、内脏功能等),Wagner 3级伤口已深及骨髓,局部组织存在大量坏死,血液循环严重不良,在这种恶劣的环境下,肾损害的影响不那么突出,Wagner 3级及以上患者多伴有不同程度的营养不良,蛋白及肌酐较低,故相应的UACR会偏低,由肌酐估算出的eGFR会偏高。另一方面Wagner 3级已引起临床医师对糖尿病肾损害的重视,往往在这一级会使用多学科联合治疗并且较为有效,但随足病发展至Wagner 4~5级肾功能还是不可避免明显下降,最终可能进展为终末期肾病或需要透析治疗。
多元逐步回归分析显示DF除与肾损害相关外还与多个因素相关。男性、合并DR、Alb降低、UA升高、2hPPG异常都与DF的发生、发展显著相关,在临床工作中对这些人群需更加严格的检查和治疗。
本研究采用单中心研究,其优点是在诊断、治疗和录入电子档案都按照统一标准。但本研究也有不足,MDRD公式由SCr计算得出eGFR,虽已校正SCr测定中影响GFR评价的因素,但仍有研究提出此公式有缺陷包括可能低估GFR值[15],若要进一步准确测定GFR,可能需要采用同位素法或测定血清胱抑素C[16]。
综上所述,DF与CKD关系密切,两者在彼此病程发展中都有促进的作用。在临床工作中建议对DF患者常规筛查是否存在肾损害,包括MAU和GFR。Wagner 3级是肾病进展及临床治疗的转折点,在该阶段鼓励多学科联合护理足部溃疡和保护肾功能,可以有效地延缓足病及肾病的发展,提高患者生活质量,但随足病发展到Wagner 4~5级时,肾功能还是会不可挽救地进一步恶化。
[1] Jeffcoate WJ, Harding KG. Diabetic foot ulcers[J]. Lancet, 2003, 361(9368): 1545−1551.
[2] van Houtum WH, Lavery LA, Harkless LB. The impact of diabetes-related lower-extremity amputations in the Netherlands[J]. J Diabetes Complications, 1996, 10(6): 325−330.
[3] Akha O, Kashi Z, Makhlough A. Correlation between amputation of diabetic foot and nephropathy[J]. Iran J Kidney Dis, 2010, 4(1): 27−31.
[4] Ndip A, Lavery LA, Boulton AJ. Diabetic foot disease in people with advanced nephropathy and those on renal dialysis[J]. Curr Diab Rep, 2010, 10(4): 283−290.
[5] Valabhji J. Foot problems in patients with diabetes and chronic kidney disease[J]. Ren Care, 2012, 38 (Suppl 1): 99−108.
[6] Wolf G, Muller N, Busch M,. Diabetic foot syndrome and renal function in type 1 and 2 diabetes mellitus show close association[J]. Nephrol Dial Transplant, 2009, 24(6): 1896−1901.
[7] Zubair M, Malik A, Ahmad J. The impact of creatinine clearance on the outcome of diabetic foot ulcers in North Indian tertiary care hospital[J]. Diabetes Metab Syndr, 2011, 5(3): 120−125.
[8] Lewis S, Raj D, Guzman NJ. Renal failure: implications of chronic kidney disease in the management of the diabetic foot[J]. Semin Vasc Surg, 2012, 25(2): 82−88.
[9] Benes J, Chvojka J, Sykora R,. Searching for early septic acute kidney injury:an experimental study[J]. Crit Care, 2011, 15(5): R256.
[10] Bonventre JV, Zuk A. Ischemic acute renal failure: an inflammatory disease[J]? Kidney Int, 2004, 66(2): 480−485.
[11] Game FL, Selby NM, McIntyre CW. Chronic kidney disease and the foot in diabetes—is inflammation the missing link[J]? Nephron Clin Pract, 2013, 123(1−2): 36−40.
[12] Wolf G, Ziyadeh FN. Cellular and molecular mechanisms of proteinuria in diabetic nephropathy[J]. Nephron Physiol, 2007, 106(2): 26−31.
[13] Cabre A, Lazaro I, Girona J,. Plasma fatty acid-binding protein 4 increases with renal dysfunction in type 2 diabetic patients without microalbuminuria[J]. Clin Chem, 2008, 54(1): 181−187.
[14] Liu D, Tang JY, Liu SY,. Urinary albumin/creatinine ratio compared with the albumin excretion rate detection[J]. Chin J Clin Physicians, 2010, 4(8): 144−145. [刘 丹, 唐菊英, 刘珊英, 等. 尿白蛋白/肌酐比值与白蛋白排泄率检测的比较[J]. 中华临床医师杂志, 2010, 4(8): 144−145.]
[15] Rossing P, Rossing K, Gaede P,, Monitoring kidney function in type 2 diabetic patients with incipient and overt diabetic nephropathy[J]. Diabetes Care, 2006, 29(5): 1024−1030.
[16] Zhang PP, Liu ZH. Evaluation of renal function of patients with diabetic nephropathy[J]. Chin J Nephrol Dial Transplant, 2007, 16(6): 558−563. [张培培, 刘志红. 糖尿病肾病患者肾功能的评估[J]. 肾脏病与透析肾移植杂志, 2007, 16(6): 558−563.]
(编辑: 周宇红)
Clinical analysis on kidney damage in diabetic foot patients with different Wagner grades
DING Wei1, WANG Jia-Jia1, LU Zu-Qian1,2*
(1Department of Endocrinology, No. 306 Clinical College, Anhui Medical University, Hefei 230032, China;2Department of Endocrinology, Center for Diabetes Mellitus Diagnosis and Treatment, Chinese PLA Hospital No. 306, Beijing 100101, China)
To investigate the kidney damage of the patients who have different severity of diabetic foot (Wagner grades 1 to 5) and investigate the relationship of diabetic foot with kidney disease in order to improve the clinical practice for diagnosis and treatment for diabetic foot.A retrospective study was carried out on 622 type 2 diabetes mellitus (T2DM) patients with diabetic foot and 215 T2DM patients of non-foot disease admitted to the Department of Endocrinology of Chinese PLA Hospital No.306 from June 2009 to June 2014. Their clinical data were collected and biochemical indicators were measured. The patients with non-foot disease or Wagner grades l to 3 were assigned into a group, and those with Wagner grades 4 to 5 into another group. Urinary albumin/creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) were used to evaluate the kidney damage. The relationship of the renal function with varying degrees of diabetic foot was analyzed by SPSS19.0 software.The diabetic foot group had significantly higher UACR (78.0010.60mg/g,<0.05), but lower eGFR [(100.91±44.98)(114.27±35.88)ml/min·1.73m2,<0.05] when compared with the non-foot group. Multivariate stepwise regression analysis indicated that gender, diabetic retinopathy, serum albumin, uric acid, 2-hour postprandial plasma glucose (2hPPG), UACR were associated with the incidence and development of type 2 diabetic foot (β=0.707, 0.850,-0.183,-0.006, 0.104, 0.003, all<0.05). The incidence of microalbuminuria (UACR 30−300mg/g) were significantly higher in the patients with Wagner grade 3 than those with grade 2 [49.7% (87/175)39.2% (67/171),2=3.885]. The ratio of renal insufficiency [eGFR<60ml/(min·1.73m2)] was obviously higher in those with Wagner grades 4−5 compared with those with grade 3 [23.5% (43/183)11.0% (24/220),2=11.421, all<0.05]. Those with Wagner grade 3 had less incidences of macroalbuminuria (UACR≥300mg/g) and renal insufficiency than those with grade 2, but the incidences were increased again in those with Wagner grades 4−5.The higher the Wagner classification grade is for diabetic foot, the more severe the kidney damage is. Microalbuminuria is superior to GFR to suggest kidney damage in diabetic patients. Wagner grade 3 is a turning point of the deterioration of kidney damage and clinical treatment. Clinicians should strengthen foot care and kidney protection when the patient is in Wagner grade 3.
diabetes mellitus, type 2; diabetic foot; kidney damage; urinary albumin to creatinine ratio; estimated glomerular filtration rate
R587.2
A
10.11915/j.issn.1671-5403.2015.05.082
2015−02−02;
2015−04−03
陆祖谦,E-mail: Luzuqian@vip.sina.com