低舒张压的单纯收缩期高血压研究新进展
2015-04-21李春辉孟威宏
李春辉,孟威宏
低舒张压的单纯收缩期高血压研究新进展
李春辉,孟威宏*
(沈阳军区总医院干部病房一科,沈阳 110016)
在有些高龄患者中,会出现舒张压(DBP)<60mmHg高血压患者,即低DBP的单纯收缩期高血压(ISH)。越来越多的证据表明DBP<70mmHg对机体是不利的,而低DBP的ISH患者常具有更多的心血管危险因素和更多的心血管事件风险,成为老年高血压降压治疗的难点,使用硝酸酯类药物进行治疗可能是一个有益的选择。
低舒张压;高血压;老年人;J形曲线
单纯收缩期高血压(isolated systolic hypertension,ISH)是老年高血压的最常见类型,>70岁的高血压人群中ISH患病率>90%[1],在高龄老年高血压患者中甚至会出现舒张压(diastolic blood pressure,DBP)<60mmHg(1mmHg=0.133kpa)的ISH。我们对这种特殊类型的高血压往往认识不足,本文拟对近年来这种特殊类型的高血压的新进展做一综述。
1 低DBP的产生机制及病理生理意义
血压的变化与年龄存在一定相关性,一般在50~60岁以后,DBP开始呈现下降趋势[2,3],收缩压(systolic blood pressure,SBP)继续随着年龄的增大而升高,脉压逐渐增大,所以老年高血压以ISH为常见,由于常常合并主动脉关闭不全,血压测量时大多采用柯氏音的第Ⅴ时相记录DBP。其DBP低的原因与动脉硬化弹性降低及心室舒张期、血管收缩功能下降等因素有关。老年人由于大动脉的硬化以及大血管弹力纤维被胶原纤维取代,使大血管弹性回缩力下降,同时小动脉血管阻力没有相应地增加[4],在心脏收缩时血管弹性扩张不足,使血管内压力迅速上升,表现为较高的SBP;而在心脏舒张期,由于大动脉与小动脉之间压力差的增大,使血液迅速流入小动脉,血管内压力快速下降,表现为较低的DBP。Mancusi等[5]发现,ISH患者左室心肌质量明显高于其他类型高血压患者,提示心肌重构也参与了这一过程的变化。而Franklin等[6]发现DBP<70mmHg的ISH患者年龄更高,且糖尿病和冠心病患病率是70mmHg≤DBP<90mmHg患者的2倍。上述情况说明年龄越高,DBP越低,脉压差越大,动脉硬化越重,更易发生心血管事件。
DBP降低可对机体产生相应危害,心脏收缩期冠状动脉血流量只有舒张期的20%~30%,DBP决定了冠脉的血流灌注,过低的DBP可能导致冠脉灌注不足。Franklin等[7]通过对1 924名年龄在50~79岁的无冠心病的高血压患者平均随访14.3年,发现>60岁的高血压患者DBP与冠心病的发病呈负相关。Fujishima等[8]观察无陈旧性心肌梗死的老年高血压患者发现DBP低于74.5mmHg是心电图呈现心肌缺血样改变的独立预测因子。Lagro等[9]还发现,老年高血压患者当出现低DBP的时候,23个月内死亡风险高达19%。Ungar等[10]发现脉压为78mmHg的ISH患者其死亡风险是平均脉压差为46mmHg组患者的5倍。而低DBP的ISH高血压患者脉压差将>90mmHg,其心脑血管事件和死亡风险将更高。因此,低的DBP不仅增加冠脉事件的风险,还与死亡风险的增加有关。
2 ISH患者降压治疗DBP最低耐受值的界定
研究者们对于降压治疗的J型曲线已争论了30多年,最早认为J点应>90mmHg,这一观点是1979年由Stewart等[11]提出的,通过对无并发症的原发性高血压患者随访6.5年发现,DBP<90mmHg与DBP在100~109mmHg相比,前者心肌梗死的风险增加了5倍。但后来的一些临床研究提示,最佳的DBP值应在80~90mmHg之间。1988年,Cruickshank[12]通过对6个临床试验共14 536名高血压患者的数据分析发现,对于有冠心病和周围动脉疾病的患者DBP J点是85mmHg。普伐他汀或阿托伐他汀评估和感染治疗−心肌梗死溶栓(PROVE IT-TIMI)22[13]研究数据也显示,对于心肌梗死患者,最佳DBP为80~90mmHg。国际缓释维拉帕米−群多普利研究[14](International Verapamil SR-Trandolapril Study,INVEST)表明DBP J点在84mmHg。若DBP达到此点后进一步降低,则致死或非致死性心脑血管事件发生率增加。当DBP降至70~60mmHg时,主要终点发生率增高了近1倍;当DBP<60mmHg时,主要终点发生率增高了2倍。Dorresteijn等[15]的研究也证明,有血管疾病的患者,最佳DBP为82mmHg,过低或过高都会导致心血管疾病及全因死亡率的增加。HOT研究[16]将DBP降至82.6mmHg,没有出现J形曲线。但近年来较多的证据表明,人体所能耐受的DBP应约在70mmHg。Arima等[17]通过对预防卒中复发(PROGRESS)研究数据分析发现,将DBP降至72mmHg时仍是安全的。日本一项针对>80岁的高龄老年高血压患者的随访发现[18],DBP<70mmHg死亡风险明显增高(RR值2.47)。Tringali等[19]对14270名高血压患者进行了为期2年的横断面调查,结果表明,DBP<70mmHg与高血压患者的全因死亡风险增加有关。而Framingham心脏研究(FHS)[20]最新数据也表明,DBP<70mmHg的ISH患者,与DBP在70~89mmHg的ISH患者相比,不仅冠状动脉风险增加,心力衰竭和缺血性卒中的风险也明显增加。不同的临床研究得出的最低DBP值存在很大的差异,INVEST研究[21,22]给我们新的提示,不同年龄,不同血运重建方式对DBP的耐受是不一样的,冠状动脉旁路移植术术后低DBP耐受值高于经皮冠状动脉介入治疗术后患者。这就提示我们患者对低灌注的耐受情况是受多方面因素影响的,不仅与DBP值有关,还可能与血液黏滞度、血小板黏附聚集能力、是否应用他汀类药及血管自身狭窄情况等多种因素有关。不同患者所能耐受DBP的最低值是不同的,但目前多数证据显示,ISH患者DBP<70mmHg对机体是不利的。
3 老年ISH患者如何从降压治疗中获益
早期研究认为,人体理想血压为115/75mmHg[23],血压每增加20/10mmHg,心血管死亡风险增加1倍。长期有效地控制血压可使心脑血管病发病率和死亡率大幅度下降。但新近临床研究显示,很少能直接将患者血压降至理想血压水平,老年高血压患者降压目标值为150/90mmHg[24−26],而这一目标值对ISH患者的降压治疗缺乏指导意义。
目前已经完成的有关老年高血压降压治疗的大型临床试验有9项(表1),其中老年人收缩期高血压项目(Systolic Hypertension in the Elderly Program,SHEP)、欧洲收缩期高血压临床试验(Systolic Hypertension-Europe,Syst-Eur)和中国收缩期高血压临床试验(Systolic Hypertension in China,Syst-China)等3项研究是专门针对ISH。Syst-Eur和Syst-China两项研究终点血压分别为152/79mmHg和150/81mmHg,试验结果表明,无论是在心脑血管事件还是全因死亡率上,患者都是获益的。SHEP研究入组患者平均DBP为75mmHg,治疗组终点DBP为68mmHg,对照组为73mmHg。治疗组在脑卒中发病率明显降低,但在心肌梗死和全因死亡率方面并没有明显获益。提示随着DBP的进一步下降,患者净获益在降低。目前还没有将ISH患者DBP降至<68mmHg获益的循证医学证据,因此就现有的循证医学证据而言,68~70mmHg应为ISH降压治疗的极限,更低的DBP能否从降压治疗中获益尚不确定。
4 老年低DBP的ISH治疗探讨
如何处理低DBP的ISH患者是一个非常棘手的问题。虽然指南指出老年人降压至150/90mmHg这一目标值,但因其没有体现出不同类型高血压在降压治疗方面的差异性,无法成为低DBP的ISH参照标准。对于DBP<68mmHg甚至<60mmHg的ISH的降压治疗尚无循证医学证据可循。2011年美国老年高血压专家共识[27]建议要尽量避免DBP<65mmHg的情况出现。尽管低DBP可能导致心肌灌注不足,但如果患者SBP过高仍可能导致心脑血管事件的发生,也就是说SBP高危害更大,应尽量把SBP降低到<140mmHg(<80岁)或<150mmHg(>80岁),如果血管狭窄严重,有缺血症状,应进行血管重建术,故SBP的升高程度是选择用药的基本标准。一些经验性的治疗提出[26],当DBP<60mmHg时,如SBP<150mmHg,不宜降压治疗;如SBP 150~179mmHg,可谨慎给予小剂量降压药;如SBP≥180mmHg,应给予小剂量降压药治疗。具体到患者时还应结合其年龄、临床症状、体征、血管狭窄程度及靶器官损害情况等综合判定,进行个体化用药。
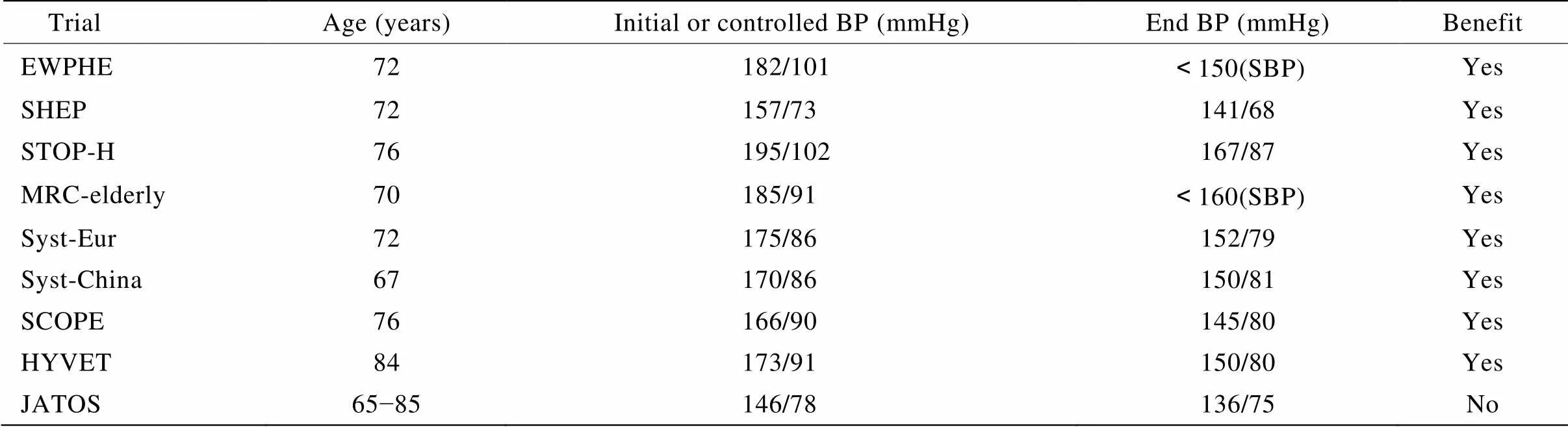
表1 老年高血压的临床试验
EWPHE: European Working Party on High Blood Pressure in the Elderly; SHEP: Systolic Hypertension in the Elderly Program; STOP-H: Swedish Trial in Old Patients with Hypertension; MRC-elderly: Medical Research Council Trial of Treatment of Hypertension in Older Adults; Syst-Eur: Systolic Hypertension-Europe; Syst-China: Systolic Hypertension in China; SCOPE: The Study on Cognition and Prognosis in the Elderly; HYVET: Hypertension in the Very Elderly Trial; JATOS: Japanese Trial to Assess Optimal Systolic Blood Pressure in Elderly Hypertensive Patients; BP: blood pressure; SBP: systolic blood pressure. 1mmHg=0.133kPa
当需要降压治疗时,选取哪种药物也是值得探讨的问题。由于ISH与动脉硬化明显相关,因此理论上具有抗动脉硬化的药物如血管紧张素转换酶抑制剂(angiotensin-converting enzyme inhibitor,ACEI)、血管紧张素受体拮抗剂(angiotensin receptor blockers,ARB)、钙通道阻滞剂(calcium channel blocker,CCB)等[28]都适用于老年ISH的治疗。SHEP、Syst-Eur、Syst-China 3个ISH的临床试验证明,噻嗪类利尿剂(thiazine diuretics)或二氢吡啶类CCB可减少患者心、脑血管病的复合终点,尤其是显著减少脑卒中发生率,为ISH患者降压治疗提供了有效性和安全性证据。氯沙坦治疗伴有左室肥厚的ISH患者的心血管事件发生率和死亡率[29][氯沙坦干预终点缩小(Losartan Intervention for Endpoint Reduction,LIFE)-ISH研究]的结果表明,在血压下降幅度相似的情况下,氯沙坦组的主要复合终点事件更低,且减少了新发糖尿病风险,降低了心血管死亡、全因死亡以及脑卒中的风险。LIFE-ISH研究提示,ARB类药物成为继利尿剂和CCB之后又一个有循证医学证据的治疗ISH的药物。但这些药物在降低SBP的同时也不同程度地降低了DBP,这对于低DBP的ISH患者来说就会存在降低冠脉灌注增加心血管事件的风险。
从理论上讲,适用于低DBP的ISH药物应最大限度地降低SBP,同时最低限度减少冠状动脉灌注。硝酸酯类药物通过释放一氧化氮改善大动脉顺应性,其对动脉的扩张主要体现在对大动脉而非终末阻力动脉血管。通过扩张大动脉的直径、增强动脉壁的舒张功能和改善动脉顺应性,从而达到降低SBP的目的,而此方法对DBP的影响非常有限;由于它具有扩张冠状动脉的作用,因此不会降低冠状动脉血流灌注。一些小型的临床观察[30−32],已显示出其在治疗ISH方面的可行性,前景看好,但尚缺乏大型临床试验的证据。
总之,低DBP的ISH是老年高血压处理的难点,要重视DBP过低所带来的潜在风险,尤其对于高龄老人,必须平衡其获益和风险,在充分遵循循证医学证据的前提下,做到选药个体化,尽量选择对DBP和冠状动脉灌注影响小的药物。随着经验的积累和不断地探索总结,优化针对这一特殊类型的高血压的治疗方法,必将进一步改善老年高血压患者的预后。
[1] Franklin SS, Jacobs MJ, Wong ND,. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES)Ⅲ[J]. Hypertension, 2001, 37(3): 869−874.
[2] Wright JD, Hughes JP, Ostchega Y,. Mean systolic and diastolic blood pressure in adults aged 18 and over in the United States, 2001−2008[J]. Natl Health Stat Report, 2011, (35): 1−22, 24.
[3] Franklin SS, Gustin W 4th, Wong ND,. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study[J]. Circulation, 1997, 96(1): 308−315.
[4] Franklin SS, Pio JR, Wong ND,. Predictors of new-onset diastolic and systolic hypertension: the Framingham Heart Study[J]. Circulation, 2005, 111(9): 1121−1127.
[5] Mancusi C, Gerdts E, De Simone G,. Impact of isolated systolic hypertension on normalization of left ventricular structure during antihypertensive treatment (the LIFE study)[J]. Blood Press, 2014, 23(4): 206−212.
[6] Franklin SS, Chow VH, Mori AD,. The significance of low DBP in US adults with isolated systolic hypertension[J]. J Hypertens, 2011, 29(6): 1101−1108.
[7] Franklin SS, Khan SA, Wong ND,. Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham Heart Study[J]. Circulation, 1999, 100(4): 354−360.
[8] Fujishima S, Murakami N, Haga Y,. Low diastolic blood pressure was one of the independent predictors of ischemia-like findings of electrocardiogram in patients who underwent coronary angiography[J]. J Cardiol, 2013, 62(4): 230−235.
[9] Lagro J, Laurenssen NC, Schalk BW,. Diastolic blood pressure drop after standing as a clinical sign for increased mortality in older falls clinic patients[J]. J Hypertens, 2012, 30(6): 1195−1202.
[10] Ungar A, Pepe G, Lambertucci L,. Low diastolic ambulatory blood pressure is associated with greater all-cause mortality in older patients with hypertension[J]. J Am Geriatr Soc, 2009, 57(2): 291−296.
[11] Stewart IM. Relation of reduction in pressure to first myocardial infarction in patients receiving treatment for severe hypertension[J]. Lancet, 1979, 1(8121): 861−865.
[12] Cruickshank JM. Coronary flow reserve and the J curve relation between diastolic blood pressure and myocardial infarction[J]. BMJ, 1988, 297(6658): 1227−1230.
[13] Bangalore S, Qin J, Sloan S,. What is the optimal blood pressure in patients after acute coronary syndromes? Relationship of blood pressure and cardiovascular events in the Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction (PROVE IT-TIMI) 22 trial[J]. Circulation, 2010, 122(21): 2142−2151.
[14] Messerli FH, Mancia G, Conti CR,. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous[J]? Ann Intern Med, 2006, 144(12): 884−893.
[15] Dorresteijn JA, van der Graaf Y, Spiering W,. Relation between blood pressure and vascular events and mortality in patients with manifest vascular disease: J-curve revisited[J]. Hypertension, 2012, 59(1): 14−21.
[16] Hansson L, Zanchetti A, Carruthers SG,. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group[J]. Lancet, 1998, 351(9118): 1755−1762.
[17] Arima H, Chalmers J, Woodward M,. Lower target blood pressures are safe and effective for the Prevention of Recurrent Stroke: the PROGRESS trial[J]. J Hypertens, 2006, 24(6): 1201−1208.
[18] Kagiyama S, Takata Y, Ansai T,. Does decreased diastolic blood pressure associate with increased mortality in 80-year-old Japanese[J]. Clin Exp Hypertens, 2009, 31(8): 639−647.
[19] Tringali S, Oberer CW, Huang J. Low diastolic blood pressure as a risk for all-cause mortality in VA patients[J]. Int J Hypertens, 2013, 2013: 178780.
[20] Franklin SS, Gokhale SS, Chow VH,. Does low diastolic blood pressure contribute to the risk of recurrent hypertensive cardiovascular disease events? The Framingham Heart Study[J]. Hypertension, 2015, 65(2): 299−305.
[21] Denardo SJ, Gong Y, Nichols WW,. Blood pressure and outcomes in very old hypertensive coronary artery disease patients: an INVEST substudy[J]. Am J Med, 2010, 123(8): 719−726.
[22] Denardo SJ, Messerli FH, Gaxiola E,. Coronary revascularization strategy and outcomes according to blood pressure (from the International Verapamil SR-Trandolapril Study [INVEST])[J]. Am J Cardiol, 2010, 106(4): 498−503.
[23] Lewington S, Clarke R, Qizilbash N,. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies[J]. Lancet, 2002, 360(9349): 1903−1913.
[24] Düsing R. The US-American Hypertension Guideline 2014: JNC 8[J]. Dtsch Med Wochenschr, 2014, 139(19): 1016−1018.
[25] Taylor J. 2013 ESH/ESC guidelines for the management of arterial hypertension[J]. Eur Heart J, 2013, 34(28): 2108−2109.
[26] Cardiology Society of Chinese Medical Association, Cerebrovascular Diseases Committee of Chinese Gerontology Association. Diagnosis of hypertension in the elderly and the treatment of Chinese expert consensus (2011 Edition)[J]. Chin Med J Front (electron version), 2012, 4(2): 31−39. [中华医学会心血管病学分会, 中国老年学学会心脑血管病专业委员会. 老年高血压的诊断与治疗中国专家共识(2011版)[J]. 中国医学前沿杂志(电子版), 2012, 4(2): 31−39.]
[27] Huang J, Wildman RP, Gu D,. Prevalence of isolated systolic and isolated diastolic hypertension subtypes in China[J]. Am J Hypertens, 2004, 17(10): 955−962.
[28] Franklin SS. Is there a preferred antihypertensive therapy for isolated systolic hypertension and reduced arterial compliance[J]? Curr Hypertens Rep, 2000, 2(3): 253−259.
[29] Ruwald AC, Westergaard B, Sehestedt T,. Losartanatenolol-based antihypertensive treatment reduces cardiovascular events especially well in elderly patients: the Losartan Intervention for Endpoint reduction in hypertension (LIFE) study[J]. J Hypertens, 2012, 30(6): 1252−1259.
[30] Tamborini G, Maltagliati A, Trupiano L,. Lowering of blood pressure and coronary blood flow in isolated systolic hypertension[J]. Coron Artery Dis, 2001, 12(4): 259−265.
[31] Stokes GS. Nitrates as adjunct hypertensive treatment[J]. Curr Hypertens Rep, 2006, 8(1): 60−68.
[32] Abad-Pérez D, Novella-Arribas B, Rodríguez-Salvanés FJ,. Effect of oral nitrates on pulse pressure and arterial elasticity in patients aged over 65 years with refractory isolated systolic hypertension: study protocol for a randomized controlled trial[J]. Trials, 2013, 14: 388.
(编辑: 李菁竹)
New research progress in isolated systolic hypertension with low diastolic pressure
LI Chun-Hui, MENG Wei-Hong*
(First Department of Cadre’s Wards, General Hospital of Shenyang Military Command, Shenyang 110016, China)
Some elderly hypertensive patients may manifest as diastolic blood pressure (DBP) lower than 60mmHg, a phenomenon known as isolated systolic hypertension (ISH) with low diastolic pressure. More and more evidence shows that DBP <70mmHg is detrimental to the body. What’s more, the ISH patients with lower DBP often have more risk factors and are of higher risk for cardiovascular events, which become a difficulty for the treatment of the elderly hypertension. Nitrates may be a good option.
low diastolic blood pressure; hypertension; aged; J-shaped curve
(12BJZ02).
R544.1; R592
A
10.11915/j.issn.1671-5403.2015.08.129
2015−02−02;
2015−03−17
保健专项科研课题(12BJZ02)
孟威宏, E-mail: shuitianlianbi@sina.com
