术中目标引导液体治疗对高危老年患者术后预后的影响
2015-04-21张丹凤朱赛楠王东信
徐 婧,张丹凤,朱赛楠,王东信*
术中目标引导液体治疗对高危老年患者术后预后的影响
徐 婧1,张丹凤1,朱赛楠2,王东信1*
(北京大学第一医院:1麻醉科,2医学统计室,北京 100034)
观察基于动脉压波形变化参数分析(FloTrac)的术中液体治疗对老年高危手术患者术后预后的影响。这是一项前瞻性、标签开放的随机对照研究。将2013年10月至2014年11月138例≥65岁在北京大学第一医院拟行腹部大手术的患者随机分为两组(每组69例)。对照组术中进行常规监测、按临床现有常规进行术中液体管理;目标引导液体治疗(GDT)组术中使用FloTrac/Vigileo系统监测动脉压波形分析参数,通过输液和血管活性药的使用维持每博量变异度(SVV)<13%、心脏指数(CI)≥2.5L/(min·m2)且平均动脉压(MAP)≥65mmHg。GDT组术后心血管并发症发生率明显少于对照组[2.9%(2/69)11.6%(8/69),=0.049];GDT组术后感染并发症发生率略少于对照组,但差异无统计学意义[13.0%(9/69)26.1%(18/69),=0.053]。术后总的并发症发生率两组间差异无统计学意义(>0.05)。基于Flotrac的GDT能减少高危老年患者术后心血管并发症的发生,并有可能减少感染并发症的发生,但对整体预后的影响尚需更大样本量的研究证实。
液体治疗;血流动力学;监测,术中;手术后并发症;随机对照试验
高危患者术中如何做到恰当补液一直是个令人困扰的问题。补液过多易导致心肺负担过重和组织水肿,增加术后并发症甚至死亡风险[1];而简单地限制液体输注有可能影响组织灌注,给患者造成危害[2]。研究显示目标引导液体治疗(goal-directed therapy,GDT)可以减少术后并发症的发生[3−6]和死亡率[7]。对机械通气期间动脉压波形变化参数分析(FloTrac)是GDT的监测目标之一,研究证实其监测结果每搏量变异度(stroke volume variation,SVV)与容量反应性有很好的相关性[8−10]。但目前有关FloTrac监测参数SVV指导术中液体治疗能否改善高危患者预后的资料有限而且有争议。Benes等[11]发现基于SVV监测的容量优化措施能改善术中血流动力学状态、减少术后并发症的发生;但另一项研究[12]并未发现SVV监测的益处。本研究的目的是观察基于机械通气期间进行FloTrac监测的术中液体治疗对老年高危手术患者预后的影响。
1 对象与方法
这是一项前瞻性、标签开放的随机对照试验。研究方案得到北京大学第一医院伦理委员会审核批准(2013[662]),已在chictr.org注册(ChiCTR-TRC-13003890)。所有受试者均签署了知情同意书。本研究于2013年10月到2014年11月在北京大学第一医院进行。
1.1 研究对象及分组
入选标准为年龄≥65岁、美国麻醉医师协会(American Society of Anesthesiologists,ASA)≥Ⅱ级、拟行择期大手术(预计手术时间≥2h或失血量≥800ml)的患者。存在以下情况之一者排除:(1)术前有心律失常;(2)因先天性心脏病存在心内分流;(3)因肺部疾病不能耐受8ml/kg潮气量的机械通气;(4)肾功能衰竭需要透析治疗;(5)手术需开胸;(6)未取得知情同意。
由统计专业人员采用SAS9.2软件按照区组随机的方法生成随机数字表,符合入选标准的患者,按照入组的先后顺序根据随机数字表的分组信息,按1∶1比例随机分入对照组或GDT组。
1.2 麻醉和术中液体管理
术前常规禁食水和进行肠道准备。对照组术中监测心电图、有创动脉压、中心静脉压(central venous pressure,CVP)、脉搏氧饱和度、呼气末二氧化碳、体温和尿量;GDT组除上述常规项目外,还利用FloTrac(Adwards,美国)监测SVV和心脏指数(cardiac index,CI)变化。所有患者均采用静、吸复合麻醉,麻醉期间持续脑电双频指数(bispectral index,BIS)值40~60水平。气管插管后行间歇正压通气,潮气量8ml/kg,根据呼气末二氧化碳调节呼吸频率使动脉血二氧化碳分压维持在35~45mmHg(1mmHg=0.133kPa)。
对照组按照现有临床常规管理术中输液,目标是维持平均动脉压(mean arterial pressure,MAP)≥65mmHg、CVP 8~12mmHg(腹腔镜手术气腹建立稳定后根据CVP波动水平判断)、尿量≥0.5ml/(kg·h)。医师判断容量足够但MAP仍不能维持预计水平,则静脉输注去甲肾上腺素(noradrenaline)或多巴酚丁胺(dobutamine)维持血压。
GDT组根据SVV和CI管理术中输液:如SVV≥13%持续>5min或对前一次液体治疗出现阳性反应(表现为CI增加>10%),则快速输注乳酸林格液(lactated Ringer’s solution)250ml;5min后如SVV仍≥13%或者输液后CI增加仍>10%,则重复上述步骤。目标是维持SVV<13%、CI≥2.5L/(min·m2)且MAP≥65mmHg。如医师判断容量足够但MAP和(或)CI仍不能维持预计水平,则输注去甲肾上腺素维持血压和(或)输注多巴酚丁胺维持CI。
1.3 观察终点
主要观察终点是术后住院期间(截至术后30d)的并发症发生率。急性肾损伤(acute kidney injury,AKI)的诊断依据对血肌酐(serum creatinine,SCr)和尿量的监测,参照改善全球肾脏病预后组织(Kidney Disease:Improving Global Outcomes,KDIGO)诊断标准(2012年版)[13]做出;其他并发症由1名临床经验丰富且对分组不知情的研究者进行最终判断,定义为术后30d内新发的对患者有不良影响且需要医疗干预的情况。
1.4 统计学处理
采用SPSS14.0统计软件进行统计分析。计量资料用均数±标准差或中位数(Q1,Q3)表示,计数资料用例数(百分率)表示。计量资料两组间比较采用检验或Mann-Whitney检验,计数资料组间比较采用2检验。以术后发生并发症为结局(其他情况为删失)的变量进行生存分析,采用Kaplan-Meier进行描述,组间比较采用log-rank检验。并采用Cox比例风险回归模型校正基线有统计学差异的变量后对两组间进行比较。所有检验均为双侧检验,以<0.05为差异有统计学意义。
2 结 果
2.1 患者入选及随访情况
共138例符合入选标准的患者进入随机分组,每组各69例,均完成了术中干预并随访至出院,其中GDT组有1例患者因家属要求在术后第3天转院治疗。
2.2 两组患者基线资料和围术期情况比较
基线资料中,GDT组患者年龄高于对照组(=0.049),其他指标两组间差异无统计学意义(>0.05;表1)。
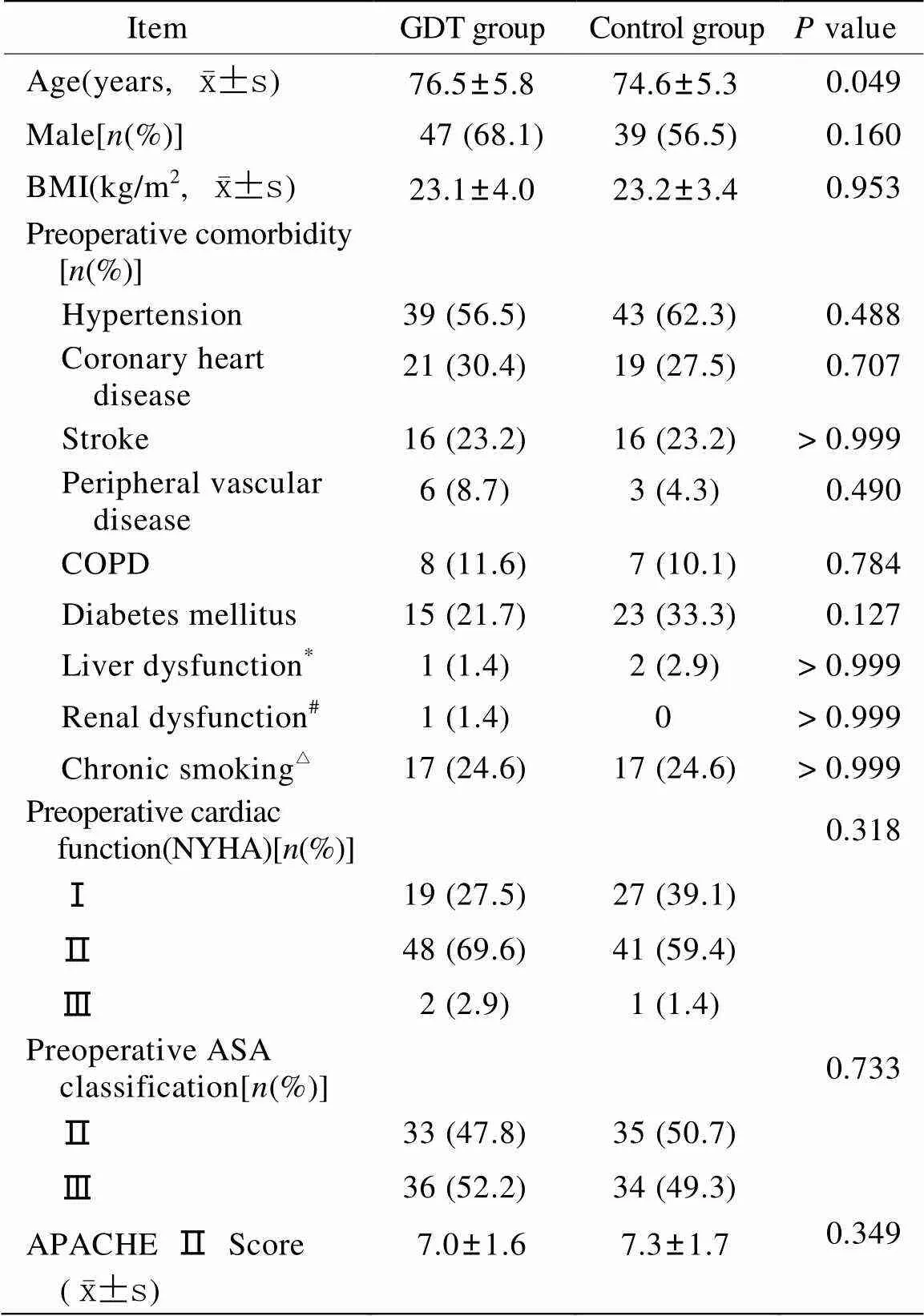
表1 所有患者的基线资料
BMI: body mass index; NYHA: New York Heart Association; COPD: chronic obstructive pulmonary disease; ASA: American Society of Anesthesiologists; APACHE: Acute Physiology and Chronic Health Evaluation.*Alanine transaminase (ALT) and/or aspartate transaminase (AST) more than five times of the upper limit of normal.#Serum creatinine (SCr) >177μmol/L.△Smoking half a pack of cigarettes per day for at least 2 years
围术期资料方面,GDT组麻醉时间和手术时间略短于对照组,但差异无统计学意义(分别为=0.051和0.061);GDT组术中多巴酚丁胺的使用比率明显高于对照组(=0.004),而麻黄碱的使用比率GDT组略低于对照组,但差异无统计学意义(=0.087)。其他指标两组间差异无统计学意义(>0.05;表2)。
2.3 两组患者术后情况比较
GDT组术后心血管并发症发生率明显低于对照组(=0.049);术后感染并发症发生率GDT组略低于对照组,但差异无统计学意义(=0.053)。其他术后并发症发生率及总的并发症发生率、并发症初发时间两组间差异均无统计学意义(>0.05;表3)。建立Cox比例风险回归模型校正年龄和手术时间后,术中动脉波形衍生参数监测并未显著延迟术后并发症初发时间(RR=1.209,95% CI 0.679~2.153,=0.518)。

表2 所有患者的术中资料
RBC: red blood cell; FFP: fresh frozen plasma.*Estimation of urine during surgery is impossible due to surgical practice, 8 and 3 patients in GDT group and control group respectively
3 讨 论
本研究的结果显示对于接受大手术的高危老年患者,术中根据机械通气期间进行FloTrac/Vigileo监测的GDT可降低术后心血管并发症发生率,并有减少术后感染并发症的趋势。
综合现有文献结果,术后各系统的并发症发生率分别为心脏15.4%[6]、胃肠道15.9%[3]、AKI 8.3%[5]、感染25.5%[4]。本研究中对照组术后各系统并发症发生率分别为心血管11.6%、胃肠道11.6%、AKI 8.7%、感染26.1%。说明本研究所观察患者的人群特征与以往研究基本一致。
Arulkumaran等[6]的荟萃分析发现GDT能减少高危手术患者术后心血管并发症的发生,认为这与在心输出量监测下、通过补液和正性肌力药物改善组织氧输送有关[14,15]。但在该荟萃分析所纳入的22项研究中仅有2项研究采用了FloTrac监测,且结果并不一致[11,16]。本研究显示根据FloTrac监测结果指导的术中液体管理减少了老年患者术后心血管并发症的发生。本研究资料显示GDT组和对照组的术中输液量无明显差异,但GDT组使用了更多的多巴酚丁胺,这可能是GDT组术后心血管并发症发生率降低的主要原因。
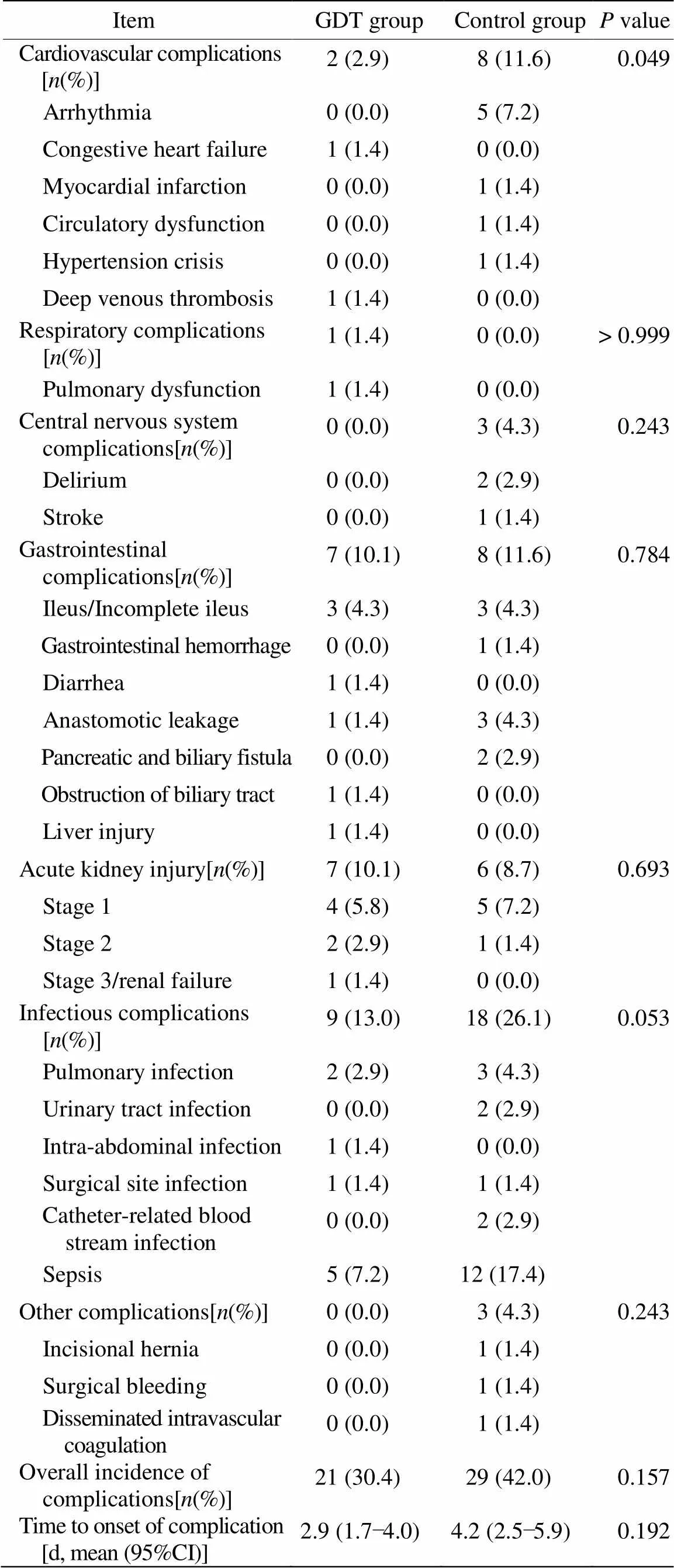
表3 所有患者的主要观察结果
Dalfino等[4]的荟萃分析发现GDT能减少术后感染并发症的风险,认为这与其改善患者的组织氧供有关[17]。但该荟萃分析所纳入的26项研究中仅3项小规模研究采用了FloTrac监测技术,结果也不一致[11,18,19]。本研究结果中虽然两组患者间术后感染并发症发生率的差异无统计学意义,但GDT组亦呈减少趋势(=0.053)。说明根据FloTrac监测指导术中容量管理可能降低术后感染风险,但仍需更进一步的研究证实。
与以往的荟萃分析结果不同[3,5,20],本研究并未发现GDT能减少术后胃肠道并发症和AKI的发生,也未能减少总的术后并发症发生率。但事实上在这些荟萃分析所纳入的研究中仅有少数研究术中采用FloTrac监测,而且这些研究均没有发现FloTrac监测组与对照组间有明显差异。本研究结果中虽然术后总并发症发生率两组间差异无统计学意义,但GDT组确实低于对照组[30.4%(21/69)42.0%(29/69),=0.157]。考虑到本研究样本量较小,术中以FloTrac动脉压波形分析参数为目标的GDT对老年高危患者预后的影响仍然值得进一步研究。
4 结 论
基于机械通气期间FloTrac监测的术中GDT能降低高危老年患者术后心血管并发症的风险,并有可能减少感染并发症的发生,但对总体并发症发生率的影响尚需更大样本量的研究证实。
[1] Moller AM, Pederson T, Svendsen PE,. Perioperative risk factors in elective pneumonectomy: the impact of excess fluid balance[J]. Eur J Anaesthesiol, 2002, 19(1): 57−62.
[2] Holte, K, Foss NB, Andersen J,. Liberal or restrictive fluid administration in fast-track colonic surgery: a randomized, double-blind study[J]. Br J Anaesth, 2007, 99(4): 500−508.
[3] Giglio MT, Marucci M, Testini M,. Goal-directed haemodynamic therapy and gastrointestinal complications in major surgery: a meta-analysis of randomized controlled trials[J]. Br J Anaesth, 2009, 103(5): 637−646.
[4] Dalfino L, Giglio MT, Puntillo F,. Haemodynamic goal-directed therapy and postoperative infections: earlier is better. A systematic review and meta-analysis[J]. Crit Care, 2011, 15(3): R154.
[5] Brienza N, Giglio MT, Marucci M,. Does perioperative hemodynamic optimization protect renal function in surgical patients? A meta-analytic study[J]. Crit Care Med, 2009, 37(6): 2079−2090.
[6] Arulkumaran N, Corredor C, Hamilton MA,. Cardiac complications associated with goal-directed therapy in high-risk surgical patients: a meta-analysis[J]. Br J Anaesth, 2014, 112(4): 648−659.
[7] Aya HD, Cecconi M, Hamilton M,. Goal-directed therapy in cardiac surgery: a systematic review and meta-analysis[J]. Br J Anaesth, 2013, 110(4): 510−517.
[8] Hofer CK, Senn A, Weibel L,. Assessment of stroke volume variation for prediction of fluid responsiveness using the modified FloTrac and PiCCOplus system[J]. Crit Care, 2008, 12(3): R82.
[9] Button D, Weibel L, Reuthebuch O,. Clinical evaluation of the FloTrac/Vigileo system and two established continuous cardiac output monitoring devices in patients undergoing cardiac surgery[J]. Br J Anaesth, 2007, 99(3): 329−336.
[10] Mayer J, Boldt J, Wolf MW,. Cardiac output derived from arterial pressure waveform analysis in patients undergoing cardiac surgery: validity of a second generation device[J]. Anesth Analg, 2008, 106(3): 867−872.
[11] Benes J, Chytra I, Altmann P,. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study[J]. Crit Care, 2010, 14(3): R118.
[12] Scheeren TW, Wiesenack C, Gerlach H,. Goal-directed intraoperative fluid therapy guided by stroke volume and its variation in high-risk surgical patients: a prospective randomized multicentre study[J]. J Clin Monit Comput, 2013, 27(3): 225−233.
[13] Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury[J].Off J Int Soc Nephrol, 2012, 2(Suppl 1): 1−138.
[14] Jhanji S, Vivian-Smith A, Lucena-Amaro S,. Haemodynamic optimisation improves tissue microvascular flow and oxygenation after major surgery: a randomised controlled trial[J]. Crit Care, 2010, 14(4): R151.
[15] Lobo SM, de Oliveira NE. Clinical review: what are the best hemodynamic targets for noncardiac surgical patients[J]? Crit Care, 2013, 17(2): 210.
[16] Cecconi M, Fasano N, Langiano N,. Goal-directed haemodynamic therapy during elective total hip arthroplasty under regional anaesthesia[J]. Crit care, 2011, 15(3): R132.
[17] Govinda R, Kasuya Y, Bala E,. Early postoperative subcutaneous tissue oxygen predicts surgical site infection[J]. Anesth Analg, 2010, 111(4): 946−952.
[18] Mayer J, Boldt J, Mengistu AM,. Goal-directed intraoperative therapy based on autocalibrated arterial pressure waveform analysis reduces hospital stay in high-risk surgical patients: a randomized, controlled trial[J]. Crit care, 2010, 14(1): R18.
[19] Van der Linden PJ, Dierick A, Wilmin S,. A randomized controlled trial comparing an intraoperative goal-directed strategy with routine clinical practice in patients undergoing peripheral arterial surgery[J]. Eur J Anaesthesiol, 2010, 27(9): 788−793.
[20] Cecconi M, Corredor C, Arulkumaran N,. Clinical review: goal-directed therapy—what is the evidence in surgical patients? The effect on different risk groups[J]. Crit Care, 2013, 17(2): 209.
(编辑: 周宇红)
Effects of intraoperative goal-directed fluid therapy by using arterial wave analysis on outcome of high-risk elderly patients
XU Jing1, ZHANG Dan-Feng1, ZHU Sai-Nan2, WANG Dong-Xin1*
(1Department of Anesthesiology,2Division of Medical Statistics, Peking University First Hospital, Beijing 100034, China)
To investigate whether the intraoperative fluid therapy based on the parameters of arterial pressure wave analysis (FloTrac) could reduce the incidence of postoperative complications in the elderly patients after major surgery.This was a prospective, open-labeled, randomized controlled trial. One hundred thirty-eight patients at an age of ≥65 years who were scheduled for major abdominal surgeries in our department from October 2013 to November 2014 were randomized into 2 groups. In the control group, routine monitoring was performed and intraoperative fluid therapy was administered according to conventional practice. In the goal-directed therapy (GDT) group, hemodynamic monitoring was performed using the FloTrac/Vigileo system, and the intraoperative goals were to maintain stroke volume variation (SVV)<13%, cardiac index (CI) ≥2.5 L/(min·m2), and mean arterial pressure (MAP) ≥65mmHg.The incidence of postoperative cardiovascular complications was significantly lower in the GDT group than in the control group[2.9%(2/69)11.6%(8/69),=0.049]. The incidence of postoperative infectious complications was slightly lower in the GDT group than in the control group, but the difference was not statistically significant [13.0%(9/69)26.1%(18/69),=0.053]. There was no significant difference between the 2 groups with regard to the overall incidence of postoperative complications.For the elderly patients undergoing major abdominal surgery, intraoperative GDT based on arterial pressure wave analysis decreases the incidence of postoperative cardiovascular complications, and also tends to decrease the incidence of postoperative infectious complications after surgery. However, its effects on the outcomes of the elderly need further study on larger samples.
fluid therapy; hemodynamics; monitoring, intraoperative; postoperative complications; randomized controlled trial
R614.2; R592
A
10.11915/j.issn.1671-5403.2015.04.067
2014−12−24;
2015−02−02
王东信, E-mail: wangdongxin@hotmail.com
