复方电解质注射液预充对合并肝功能不良体外循环心脏手术患者的影响
2015-04-01李京京肖春伟张思鑫张俊伟
程 吉,李京京,肖春伟,张思鑫,张俊伟
空军航空医学研究所附属医院 心胸外科,北京 100089
复方电解质注射液预充对合并肝功能不良体外循环心脏手术患者的影响
程 吉,李京京,肖春伟,张思鑫,张俊伟
空军航空医学研究所附属医院 心胸外科,北京 100089
目的探讨复方电解质注射液作为体外循环(cardiopulmonary bypass,CPB)预充液在肝功能不良患者心脏手术中的作用。方法回顾我院2003年7月- 2013年12月,因术前合并肝功能异常接受体外循环下心脏手术的患者41例,体外循环晶体预充液2009年10月前使用乳酸林格液,之后使复方电解质注射液。分为乳酸林格液组(A组)18例,复方电解质注射液组(B组)23例,检测两组术前(T1)、转流30 min (T2)、停机后/术后即刻(T3)、术后4 h (T4)、术后24 h (T5)的剩余碱(base excess,BE)、血乳酸(lactic acid,Lac)、电介质水平,术前、术后4 h、术后第1天、第3天、第7天肝功能酶的化变。结果两组天冬氨酸转氨酶(aspartate transaminase,AST)及丙氨酸氨基转移酶(glutamate-pyruvate transaminase,GPT)水平体外循环后进一步升高,B组术后7 d基本恢复到术前水平;Lac浓度、BE负值、氯离子浓度A组均明显高于B组(P<0.05),B组中钙离子浓度显著降低,两组血糖在CPB中均升高,组间无统计学差异。结论体外循环中使用复方电解质注射液作为预充液可减少对肝功能的损害,降低血乳酸水平,能快速有效地维持机体酸碱平衡。
心脏手术;体外循环;复方电解质注射液;肝功能不良
体外循环(cardiopulmonary bypass,CPB)使心脏手术乳酸(lactic acid,Lac)产生增加,外源性输入大量含乳酸的液体,严重干扰酸碱平衡,同时,会加重对肝的损害,影响术后恢复。最近几年,人们对体外循环中晶体预充液的选择越来越重视,本文回顾分析复方电解质注射液对合并肝功能不良患者体外循环围术期肝功能、乳酸代谢的影响。
资料和方法
1临床资料 我院2003年7月- 2013年12月,因术前合并肝功能异常接受体外循环下心脏手术的患者41例,体外循环晶体预充液2009年10月前使用乳酸林格液,之后使用复方电解质注射液。其中18例使用乳酸林格液(A组),23例使用复方电解质注射液(B组)。
2方法 两组均采用静脉吸入复合维持麻醉,监测心电图及脉搏血氧饱和度,桡动脉或股动脉穿刺连续监测动脉压,右侧颈内静脉穿刺监测中心静脉压。采用JOSTRA体外循环机,Turmo成人膜肺。预充液的胶体均用琥珀酰明胶(血定安,Fisenus) 1 000 ml,晶体液800 ~ 1 000 ml,A组乳酸林格液;B组为复方电解质注射液,浅低温体外循环,转中ACT维持在480 s以上。灌注流量为2.0 ~3.4 L/(min·m2),维持平均动脉压40 ~ 70 mmHg (1 mmHg=0.133 kPa),4∶1氧合血停搏液心肌保护,每例患者均在术前(T1)、转流30 min(T2)、停机后/术后即刻(T3)、术后4 h(T4)、术后24 h(T5)分别采集2 ml血液。测血气、酸碱平衡、电介质、Lac+。所有患者均在术前,术后4 h,术后第1天、第3天、第7天采中心静脉血分离血清后检测血清中天冬氨酸转氨酶(aspartate transaminase,AST)及丙氨酸氨基转移酶(glutamate-pyruvate transaminase,GPT)值,以了解患者的肝功能改变。
3统计学处理 采用SPSS13.0统计软件进行统计学处理。计量资料用表示,组间均数的比较应用两个独立样本t检验,组内资料应用配对t检验。P<0.05为差异有统计学意义。
结 果
1基本资料 两组患者年龄、体质量、性别构成比、手术种类、体外循环转流时间、升主动脉阻断时间组间均无统计学差异(P>0.05)。所有患者手术顺利完成无死亡,均痊愈出院。见表1。
2肝功能及血糖变化 两组患者GPT及AST水平术前均异常,体外循环后进一步升高,术后第1天达到最高水平,A组高于B组(P<0.05),术后第3天开始下降。A组术后第7天仍然高于术前。两组血糖水平在体外循环早期均显著升高,但组间差异无统计学意义。见表2。
3酸碱及离子变化 A组乳酸较术前明显升高(P<0.05),持续到术后24 h。B组较术前略有升高,但差异无统计学意义(P>0.05)。碱剩余(base excess,BE)值在A组中各时点都明显高于B组,差异有统计学意义,B组BE值很快在术后早期恢复到正常水平。氯离子(Cl-)A组水平显著上升,而B组变化不明显。B组体外循环中钙离子(Ca2+)浓度较术前明显下降。见表3。

表1 两组临床资料比较Tab.1 Clinical data about patients in two groups
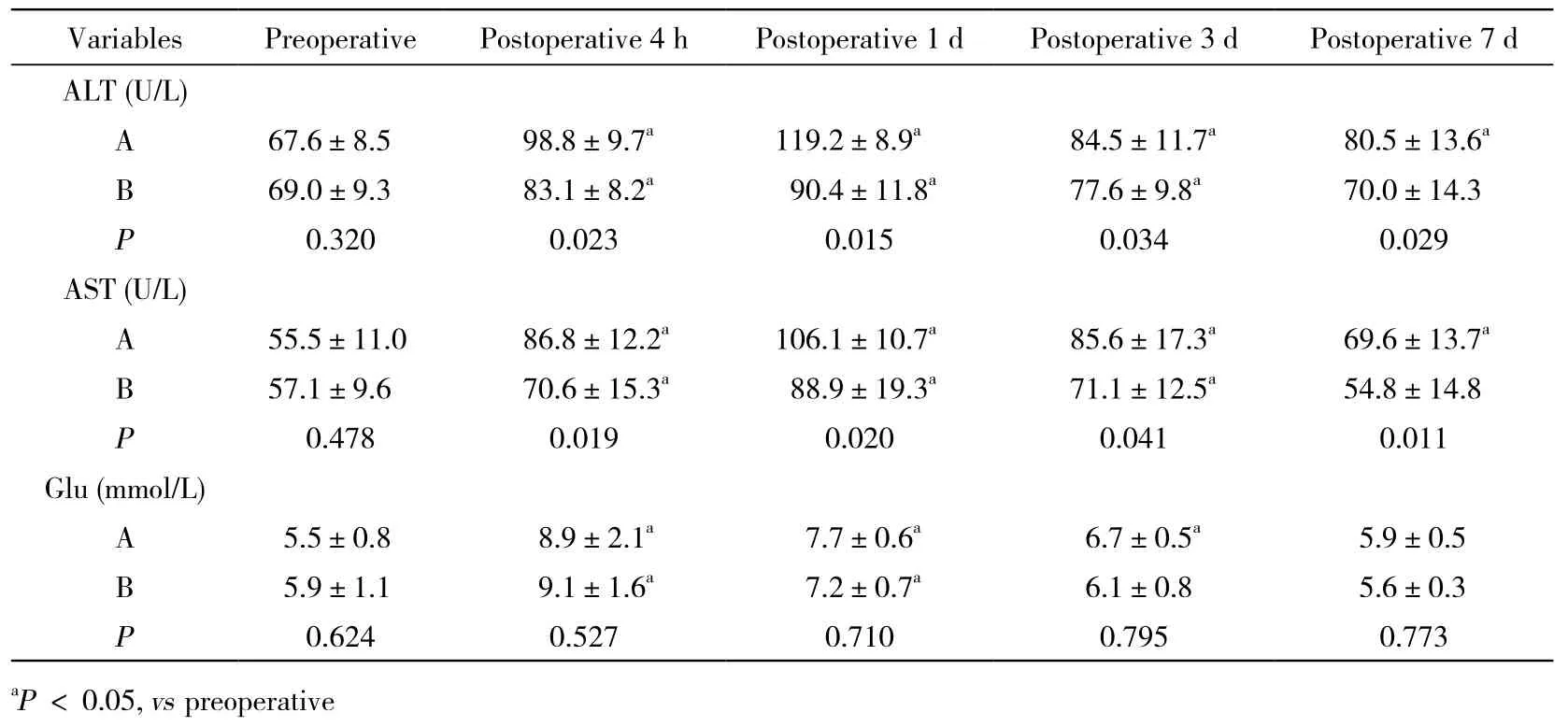
表2 两组肝功酶、血糖变化比较Tab. 2 Comparison of changes in hepatic enzyme and blood glucose
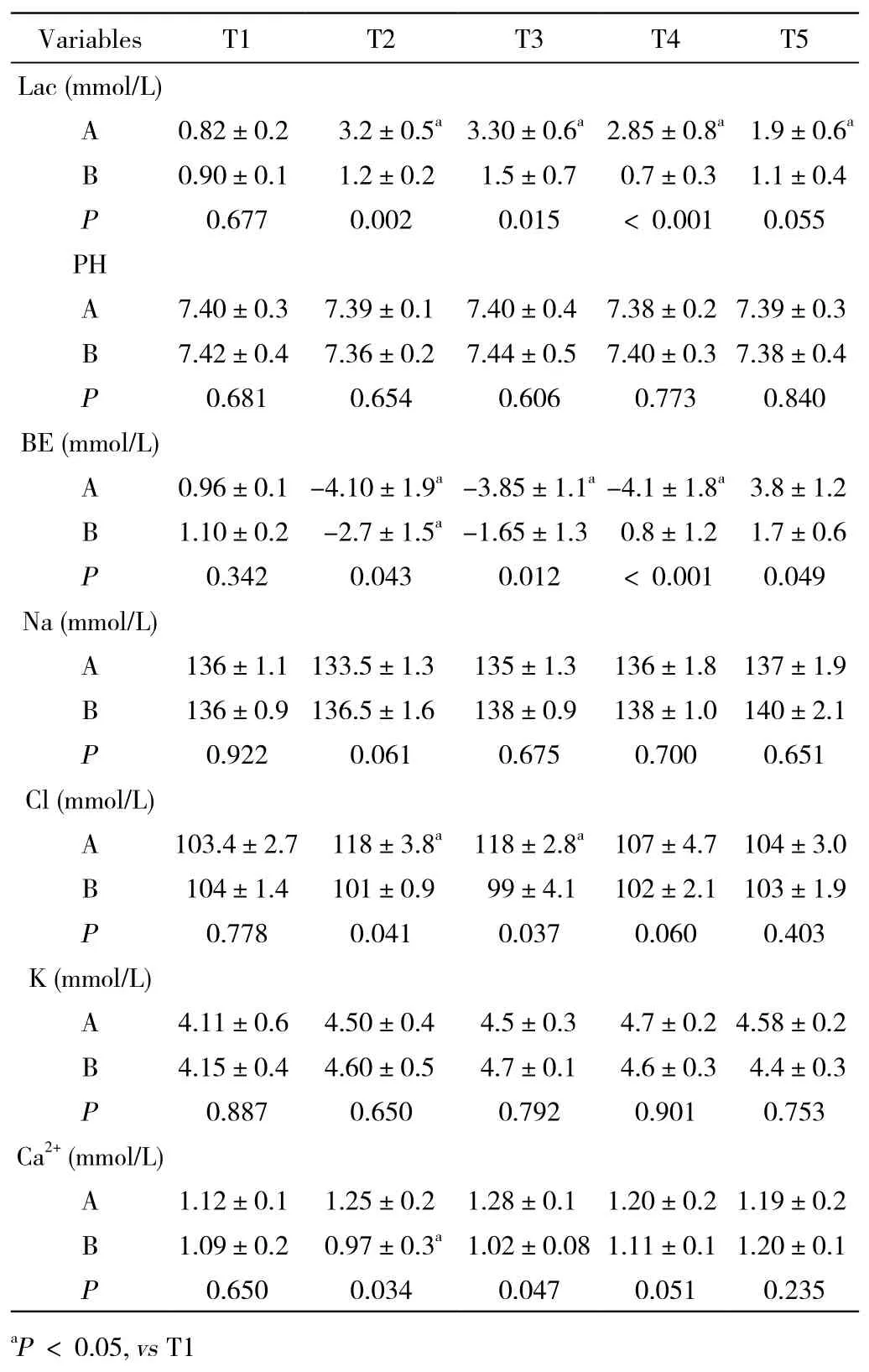
表3 两组酸碱平衡及电介质变化比较Tab. 3 Comparison of changes in acid-base and electrolytes
讨 论
心脏手术时,体外循环可直接损害肝功能,这是由于CPB中血液与异物表面接触,激活血液细胞释放大量的炎性介质、非搏动灌注及可能的低灌注血压、库血输入、低温等引起[1-3]。对于术前合并肝功能不良的患者,CPB可进一步加重对肝的损伤[4-5],本实验的结果再次证明了这一点。研究表明,不同的晶体预充液直接影响体外循环术中肝功能及酸碱平衡代谢的变化[6],预充液应尽量选用合乎生理的不经过肝代谢或对肝损伤小的液体。研究开发“理想的生理平衡液”,成为近几年液体平衡治疗的热点话题。
乳酸林格液从20世纪30年代开始应用至今,广泛应用于体外循环晶体预充液,不足之处逐渐显露,特别是对于危重患者,由于其高乳酸及高氯离子含量,临床中极易发生高乳酸血症和高氯血症性酸中毒[7-8],甚至有增加肾损害的风险[9]。在本研究中,乳酸林格组血浆氯离子水平明显升高,这也是代谢性酸中毒的原因之一。事实上,无论是外源性乳酸还是内生性乳酸,它们的代谢都依赖肝的功能,乳酸有D-乳酸和L-乳酸两种旋光异构体,内生性乳酸为L型,外源输入或由肠道内吸收的D-乳酸在体内几乎不被代谢,且对肝细胞、肺上皮细胞及神经元有直接毒性作用[10-11]。机体内葡萄糖经丙酮酸途径生成的L-乳酸,其代谢主要在肝,20% ~ 30%在肾,代谢生成等分子的HCO3-发挥其缓冲作用[12]。因生产L-乳酸林格液工艺复杂,目前市售乳酸林格液中的乳酸盐几乎多为D-乳酸盐与L-乳酸盐等量混合的消旋体,所以大量输注容易导致乳酸体内堆积[13]。
基于上述问题,美国推出一种不含钙的复方电解质溶液[14],其优点是pH值为7.4,渗透压接近血浆(308 mOsm/L);CI-和Na+浓度接近血浆,不会引起高氯血症性酸中毒;K+和Mg2+浓度接近细胞外液,有利维护细胞膜的功能;不含乳酸,含有碳酸氢盐前体物质醋酸根和葡萄糖酸根,采用醋酸盐作为酸碱缓冲体系,具有更大的酸碱缓冲能力,且不额外升高血糖,在体内代谢不依赖肝,不加重肝负担,其代谢速率为乳酸的2倍以上,能快速缓冲体外循环中产生的酸性产物[15]。国内已用于婴幼儿体外循环中,并取得了良好的效果[16]。本研究结果显示,复方电解质注射液用于术前合并肝功能不良的患者,CPB中不增加乳酸的浓度,具有良好的酸碱缓冲性能力,维持术中BE值在正常范围水平,该结果与Liskaser等[17]及Noritomi等[18]的研究一致。其次,其对肝功能的影响明显低于传统的乳酸林格液,肝功能酶在术后能快速恢复到术前水平,证明复方电解质溶液不额外增加肝损害。同时我们注意到,由于复方电解质注射液不含钙,在体外循环中大量应用会导致稀释性血浆钙浓度的降低,应根据检测结果及时予以补充,避免影响凝血功能和心脏收缩功能。
综上所述,体外循环心脏手术中使用复方电解质注射液作为晶体预充液可减少对肝功能的损害,快速有效地维持机体酸碱平衡,减少乳酸的堆积,与乳酸林格液比,更适合于合并肝功能不良患者的体外循环心脏手术。
1 Gravlee GP, Davis RF, Stammers AH.体外循环原理与实践[M] . 3版.北京:人民卫生出版社,2009:273-275.
2 Shen Z, Wang Z, Zhang J, et al. Hepatic injury in a rat cardiopulmonary bypass model[J]. Interact Cardiovasc Thorac Surg, 2008, 7(1):18-22.
3 Modi A, Vohra HA, Barlow CW. Do patients with liver cirrhosis undergoing cardiac surgery have acceptable outcomes?[J]. Interact Cardiovasc Thorac Surg, 2010, 11(5): 630-634.
4 An Y, Xiao YB, Zhong QJ. Open-heart surgery in patients with liver cirrhosis: indications, risk factors, and clinical outcomes[J]. Eur Surg Res, 2007, 39(2): 67-74.
5 Murashita T, Komiya T, Tamura N, et al. Preoperative evaluation of patients with liver cirrhosis undergoing open heart surgery[J]. Gen Thorac Cardiovasc Surg, 2009, 57(6):293-297.
6 Shin WJ, Kim YK, Bang JY, et al. Lactate and liver function tests after living donor right hepatectomy: a comparison of solutions with and without lactate[J]. Acta Anaesthesiol Scand, 2011, 55(5):558-564.
7 Liskaser FJ, Bellomo R, Hayhoe M, et al. Role of pump prime in the etiology and pathogenesis of cardiopulmonary bypass-associated acidosis[J]. Anesthesiology, 2000, 93(5): 1170-1173.
8 Kim SY, Huh KH, Lee JR, et al. Comparison of the effects of normal saline versus plasmalyte on Acid-Base balance during living donor kidney transplantation using the stewart and base excess methods[J]. Transplant Proc, 2013, 45(6): 2191-2196.
9 Yunos NM, Bellomo R, Hegarty C, et al. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults[J]. JAMA, 2012, 308(15): 1566-1572.
10 Dahhak S, Uhlen S, Mention K, et al. D-lactic acidosis in a child with short bowel syndrome[J]. Arch Pediatr, 2008, 15(2):145-148.
11 Ayuste EC, Chen H, Koustova E, et al. Hepatic and pulmonary apoptosis after hemorrhagic shock in swine can be reduced through modifications of conventional Ringer’s solution[J]. J Trauma, 2006, 60(1):52-63.
12 Burdett E, Dushianthan A, Bennett-Guerrero E, et al. Perioperative buffered versus non-buffered fluid administration for surgery in adults[J/OL]. http://dx.doi.org/10.1002/14651858.CD004089.pub2.
13 Adeva-Andany M, López-Ojén M, Funcasta-Calderón R, et al. Comprehensive review on lactate metabolism in human health[J]. Mitochondrion, 2014, 17(17): 76-100.
14 Morgan TJ, Power G, Venkatesh B, et al. Acid-base effects of a bicarbonate-balanced priming fluid during cardiopulmonary bypass:comparison with Plasma-Lyte 148. A randomised single-blinded study[J]. Anaesth Intensive Care, 2008, 36(6):822-829.
15 Morgan TJ. The ideal crystalloid - what is `balanced’?[J]. Curr Opin Crit Care, 2013, 19(4): 299-307.
16 王伟, 朱德明, 张蔚, 等. 儿童心肺转流中不同预充基础液的应用比较[J]. 中国体外循环杂志, 2006, 4(2): 82-84.
17 Liskaser F, Story DA, Hayhoe M, et al. Effect of pump prime on acidosis, strong-ion-difference and unmeasured ions during cardiopulmonary bypass[J]. Anaesth Intensive Care, 2009, 37(5):767-772.
18 Noritomi DT, Pereira AJ, Gomes Bugano DD, et al. Impact of Plasma-Lyte pH 7.4 on acid-base status and hemodynamics in a model of controlled hemorrhagic shock[J]. Clinics, 2011, 66(11):1969-1974.
Effects of multiple electrolytes injection on patients with hepatic dysfunction undergoing cardiac surgery with cardiopulmonary bypass
CHENG Ji, LI Jingjing, XIAO Chunwei, ZHANG Sixin, ZHANG Junwei
Department of Cardiothoracic Surgery, Affiliated Hospital of Air Force Institute of Aeromedicine, Beijing 100089, China
ObjectiveTo explore the effects of multiple electrolytes injection as cardiopulmonary bypass (CPB) priming solution for patients with hepatic dysfunction undergoing open heart surgery.MethodsClinical data about 41 patients with hepatic dysfunction who underwent cardiac surgeries with CPB in our hospital from July 2003 to December 2013 were retrospectively analyzed. Lactate Ringer's solution was used as CPB priming fluid before October 2009 and then multiple electrolytes injection were used as priming fluid. They were divided into two groups: lactate ringer's group (group A, n=18) and multiple electrolytes injection group (group B, n=23). BE, Lac and electrolytes levels were detected at pre-CPB (T1), 30 minutes after CPB (T2), off-CPB (T3), postoperative 4 hours (T4) and 24 hours (T5), hepatic enzymes of AST, GPT and blood glucose were measured at preoperation, postoperative 4 hours, days 1, 3, and 7.ResultsThe levels of AST and GPT increased notably after CPB in two groups, but it returned to baseline on postoperative 7 d in group B; the concentrations of Lac, BE, Cl- were significantly higher in group A than those of group B (P<0.05), the plasma calcium level was lower than that of preoperation in group B. There was no difference in blood glucose between two groups.ConclusionMultiple electrolytes injection as CPB priming solution can decrease lactate levels and alleviate the harm to liver caused by CPB, and maintain acid-base balance effectively.
cardiac surgery; extracorporeal circulation; multiple electrolytes injection; hepatic dysfunction
R 654.1
A
2095-5227(2015)05-0470-04
10.3969/j.issn.2095-5227.2015.05.017
时间:2015-01-14 18:27
http://www.cnki.net/kcms/detail/11.3275.R.20150114.1827.007.html
2014-10-29
程吉,男,副主任医师,主任。研究方向:心血管外科、体外循环及ICU。Email: chengji725@sina.com
The first author: CHENG Ji. Email: chengji725@sina.com