二尖瓣反流诊治进展
2015-03-16阚通综述秦永文审校
阚通综述秦永文审校
(第二军医大学附属长海医院心血管内科, 上海200433)
二尖瓣反流诊治进展
阚通 综述秦永文 审校
(第二军医大学附属长海医院心血管内科, 上海200433)
二尖瓣关闭功能取决于瓣叶、瓣环、腱索、乳头肌和左心室的结构完整和功能正常,影响到这些结构的疾病都可以导致严重的二尖瓣反流(mitral regurgitation,MR),降低患者的生存时间[1-3]。在西方国家,MR是常见的心脏瓣膜病[4]。
2014年3月,美国心脏协会与美国心脏病学会发表的心脏瓣膜病管理指南对慢性原发性(退行性)MR和慢性继发性(功能性)MR进行了明确区分[5]。慢性原发性MR由瓣叶、瓣环、腱索和乳头肌1项或以上发生病理学改变引起;慢性继发性MR继发于左心室功能异常,二尖瓣膜通常是正常的。左心室异常扩张引起乳头肌移位,致瓣叶腱索过度紧张,最终导致MR。原发性和继发性MR在病理生理学、预后、决策与管理上是完全不同的。在工业化国家,原发性MR最常见的病因是二尖瓣退行性变,不常见的病因是风湿性心脏病和先天性畸形,发展中国家风湿性心脏病较普遍[6]。继发性MR使扩张型心肌病患者的预后恶化[7],缺血性MR是功能性MR的一种,其左心室功能紊乱继发于心肌梗死。重度MR的自然病程不容乐观,可引起左心室衰竭、肺动脉高压、心房颤动、脑卒中和死亡[8]。
1 MR的分期
美国心脏协会与美国心脏病学会发表的心脏瓣膜病管理指南对MR进行了分期。原发性MR和继发性MR都可依据瓣膜的解剖学改变、瓣膜的血流动力学及其结局和相关症状等分为4个渐进阶段。A期:危险期;B期:进展期;C期:无症状重度病变期;D期:有症状重度病变期(见表1、表2)。

表1 原发性MR分期
*许多评估瓣膜血流动力学的标准被用以评估MR的严重程度,但并非所有标准都能在每个级别患者身上呈现。MR的严重程度通常分为轻、中、重度,取决于数据的质量以及其他临床证据。
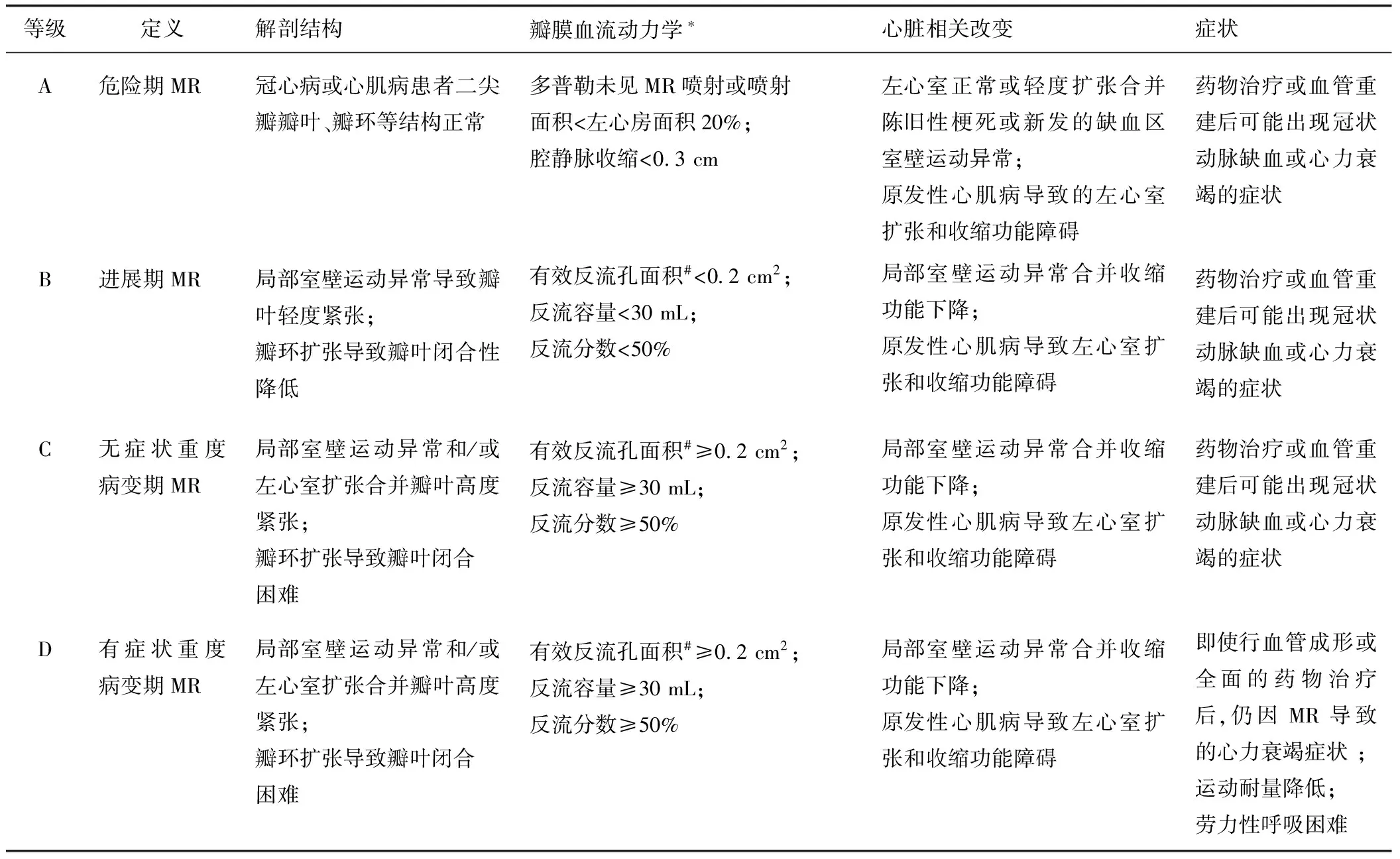
表2 继发性MR分期
*许多评估瓣膜血流动力学的标准被用以评估MR的严重程度,但并非所有标准都能在每个级别患者身上呈现。MR的严重程度通常分为轻、中、重度,取决于数据的质量以及其他临床证据。
#可通过二维经胸心脏超声进行等速表面积法计算继发性MR患者的有效反流口面积,但由于该孔常为新月形,测得值常低于真实值。
2 MR的诊断
2.1 慢性原发性MR
推荐使用经胸心脏超声对任何怀疑患有慢性原发性MR的患者(A~D期)进行如左心室大小和功能、右心室功能、左心房大小、肺动脉压力,以及MR的程度及可能原因的基本评估(Ⅰ,证据B)[9-13];若经胸心脏超声无法确定原发性MR患者的左右心室容量、功能及反流的程度时,推荐使用心脏核磁共振帮助评估上述指标(Ⅰ,证据B)[14-15];推荐手术中使用经食管超声心动图以评估慢性原发性MR(C、D期)的解剖结构,指导修复方案的制定(Ⅰ,证据B)[16];当非创伤性影像检查提供的诊断信息不足时,推荐使用经胸心脏超声以判断慢性原发性MR的严重程度(B~D期)、发病机制及左心室功能状态(Ⅰ,证据C)。
2.2 慢性继发性MR
通过经胸心脏超声可评估慢性继发性MR(B~D期)的严重程度和病因、瓣膜运动异常的程度和位置、左心室功能及肺动脉高压等级(Ⅰ,证据C)。无创的影像学检查(如压力原子/电子断层扫描、心脏核磁共振、负荷超声心动图),心脏增强CT,心导管检查(包括冠状动脉造影术)等,有助于明确慢性继发性MR(B~D期)的病因及评估心肌活性,进而为制定MR的治疗方案提供决策参考(Ⅰ,证据C)。
3 MR的治疗
3.1 药物治疗
对有症状的慢性原发性MR(D期)患者,若其射血分数<60%,但无手术指征时,可用药物治疗以改善左心室的收缩功能(Ⅱa,证据B)[17-18];不推荐对无症状和左心室收缩功能正常的慢性原发性MR(B和C1期)患者使用血管舒张剂(Ⅲ,证据B)[19-20]。
对慢性继发性MR(B~D期)患者,若其伴有左心室射血分数降低的心力衰竭,则需要给予指南推荐的药物治疗方案,以改善其心功能。常见的药物有:血管紧张素转换酶抑制剂、血管紧张素受体拮抗剂、β受体阻滞剂和醛固酮拮抗剂等(Ⅱ,证据A)[21-22]。
3.2 起搏器治疗
对有症状的慢性继发性MR(B~D期)患者,若满足安置起搏器的指征,则推荐采用左右双起搏疗法(Ⅱ,证据A)[23]。
3.3 手术治疗
及时适当的纠正退行性MR可显著改善患者预后,甚至可使患者获得同普通人群相似的预期寿命和生活质量[24]。目前指南推荐有症状的重度原发性MR患者接受手术治疗(推荐类型:Ⅰ级),伴有左心室功能衰竭无症状患者接受手术治疗(推荐类型:Ⅰ级),左心室功能正常的无症状患者如果成功修复可能性大接受手术治疗(推荐类型:Ⅱa级)[5, 25]。有症状的继发性MR患者接受最佳药物治疗后也可考虑手术治疗(推荐类型:Ⅱb级)。欧洲心脏病协会和美国心脏病学会颁布的指南在左心室功能障碍和几项推荐的证据等级上稍有不同。
虽然有症状的重度MR患者没有手术治疗和药物治疗的随机对照研究,观测到的数据已表明手术治疗可提高生存率[26]。
3.4 经导管途径治疗
手术治疗伴随着1%~5%的病死率和10%~20%包括脑卒中、再次手术、肾功能衰竭和吸氧时间延长的发生率[27]。在合并左心室功能障碍的老年患者中更是如此;80~89岁的患者手术后病死率达17%,超过1/3的患者发生术后并发症[28]。由左心室功能障碍引起的继发性MR患者,无论是否接受手术治疗生存率较原发性患者低。通过外科二尖瓣成形术未提高继发性MR患者的生存率。无论是缺血性和不缺血性的功能性MR,年龄和并发症对患者生存率影响最大。创伤小、并发症少、费用少的经导管途径治疗MR的方法将更加适合老年、高风险患者。
目前只有美国雅培公司的Mitra Clip一种经导管途径装置被批准用于临床治疗继发性MR。此设备在2013年10月被批准应用是基于随机对照试验EVEREST Ⅱ的结果[29-31]。在EVEREST Ⅱ中来自37个中心的279例患者(73%为继发性MR)被随机分为接受经皮二尖瓣修复组(n=184)和开放手术二尖瓣修复组(n=95)。同开放手术组相比经皮二尖瓣修复组患者虽然疗效略差,但安全性较高。同开放手术组相比经皮二尖瓣修复组患者需要再次手术解决残留MR的患者较多,但1年随访后,两组患者需再次手术的很少,4年后病死率两组未见明显差别[31]。
几项研究表明,同开放手术相比,虽然经导管二尖瓣修复术在减少MR上效果较差,但提高了不能手术或者高危患者的生活质量和临床转归[32-37]。
4 总结
MR是常见的心脏瓣膜病,依据病因可将MR分为原发性MR和继发性MR,严重MR对患者危害极大。MR依据瓣膜的解剖学改变、瓣膜的血流动力学及其结局和相关症状等分为A期:危险期;B期:进展期;C期:无症状重度病变期;D期:有症状重度病变期4个渐进的阶段。MR诊断主要依据经胸心脏超声,无创的影像学检查(如压力原子/电子断层扫描、心脏核磁共振、负荷超声心动图),心脏增强CT,心导管检查(包括冠状动脉造影术)等。MR主要有药物治疗、起搏器治疗、手术治疗和经导管途经治疗。经导管二尖瓣修复术在减少MR上效果较差,但提高了不能手术或者高危患者的生活质量和临床转归,是治疗MR安全可靠的方法。
[1] Trichon BH, Felker GM, Shaw LK, et al. Relation of frequency and severity of mitral regurgitation to survival among patients with left ventricular systolic dysfunction and heart failure[J]. Am J Cardiol,2003,91(5):538-543.
[2] Bursi F, Enriquez-Sarano M, Nkomo VT, et al. Heart failure and death after myocardial infarction in the community:the emerging role of mitral regurgitation[J]. Circulation,2005,111(3):295-301.
[3] Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation[J]. N Engl J Med,2005,352(9):875-883.
[4] Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study[J]. Lancet,2006,368(9540):1005-1011.
[5] Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease:executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines[J]. J Am Coll Cardiol,2014,63(22):2438-2488.
[6] Iung B, Vahanian A. Epidemiology of valvular heart disease in the adult[J]. Nat Rev Cardiol,2011,8(3):162-172.
[7] Bursi F, Enriquez-Sarano M, Nkomo VT, et al. Heart failure and death after myocardial infarction in the community:the emerging role of mitral regurgitation[J]. Circulation,2005,111(3):295-301.
[8] Ling LH, Enriquez-Sarano M, Seward JB, et al. Clinical outcome of mitral regurgitation due to flail leaflet[J]. N Engl J Med,1996,335(19):1417-1423.
[9] Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography[J]. J Am Soc Echocardiogr,2003,16(7):777-802.
[10]Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation[J]. N Engl J Med,2005,352(9):875-883.
[11]Lang RM, Badano LP, Tsang W, et al. EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography[J]. J Am Soc Echocardiogr,2012,25(1):3-46.
[12]Magne J, Mahjoub H, Pierard LA, et al. Prognostic importance of brain natriuretic peptide and left ventricular longitudinal function in asymptomatic degenerative mitral regurgitation[J]. Heart,2012,98(7):584-591.
[13]Witkowski TG, Thomas JD, Debonnaire PJ, et al. Global longitudinal strain predicts left ventricular dysfunction after mitral valve repair[J]. Eur Heart J Cardiovasc Imaging,2013,14(1):69-76.
[14]Pflugfelder PW, Sechtem UP, White RD, et al. Noninvasive evaluation of mitral regurgitation by analysis of left atrial signal loss in cine magnetic resonance[J]. Am Heart J,1989,117(5):1113-1119.
[15]Myerson SG, Francis JM, Neubauer S. Direct and indirect quantification of mitral regurgitation with cardiovascular magnetic resonance, and the effect of heart rate variability[J]. MAGMA,2010,23(4):243-249.
[16]Saiki Y, Kasegawa H, Kawase M, et al. Intraoperative TEE during mitral valve repair: does it predict early and late postoperative mitral valve dysfunction?[J]. Ann Thorac Surg,1998,66(4):1277-1281.
[17]Nemoto S, Hamawaki M, de Freitas G, et al. Differential effects of the angiotensin-converting enzyme inhibitor lisinopril versus the beta-adrenergic receptor blocker atenolol on hemodynamics and left ventricular contractile function in experimental mitral regurgitation[J]. J Am Coll Cardiol, 2002,40(1):149-154.
[18]Ahmed MI, Aban I, Lloyd SG, et al. A randomized controlled phase Ⅱb trial of beta(1)-receptor blockade for chronic degenerative mitral regurgitation[J]. J Am Coll Cardiol,2012,60(9):833-838.
[19]Tischler MD, Rowan M, LeWinter MM. Effect of enalapril therapy on left ventricular mass and volumes in asymptomatic chronic, severe mitral regurgitation secondary to mitral valve prolapse[J]. Am J Cardiol, 1998,82(2):242-245.
[20]Harris KM, Aeppli DM, Carey CF. Effects of angiotensin-converting enzyme inhibition on mitral regurgitation severity, left ventricular size, and functional capacity[J]. Am Heart J,2005,150(5):1106.
[21]Rowe JC, Bland EF, Sprague HB, et al. The course of mitral stenosis without surgery:ten- and twenty-year perspectives[J]. Ann Intern Med, 1960,52:741-749.
[22]The SOLVD Investigators.Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions[J]. N Engl J Med,1992,327(10):685-691.
[23]van Bommel RJ, Marsan NA, Delgado V, et al. Cardiac resynchronization therapy as a therapeutic option in patients with moderate-severe functional mitral regurgitation and high operative risk[J]. Circulation, 2011,124(8):912-919.
[24]Detaint D, Sundt TM, Nkomo VT, et al. Surgical correction of mitral regurgitation in the elderly: outcomes and recent improvements[J]. Circulation, 2006,114(4):265-272.
[25]Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012)[J]. Eur Heart J,2012,33(19):2451-2496.
[26]Enriquez-Sarano M, Schaff HV, Orszulak TA, et al. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis[J]. Circulation,1995,91(4):1022-1028.
[27]Gammie JS, O’Brien SM, Griffith BP, et al. Influence of hospital procedural volume on care process and mortality for patients undergoing elective surgery for mitral regurgitation[J]. Circulation,2007,115(7):881-887.
[28]Mehta RH, Eagle KA, Coombs LP, et al. Influence of age on outcomes in patients undergoing mitral valve replacement[J]. Ann Thorac Surg, 2002,74(5):1459-1467.
[29]Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation[J]. N Engl J Med,2011,364(15):1395-1406.
[30]Glower D, Ailawadi G, Argenziano M, et al. EVEREST Ⅱ randomized clinical trial: predictors of mitral valve replacement in de novo surgery or after the MitraClip procedure[J]. J Thorac Cardiovasc Surg,2012,143(4 Suppl):S60- S63.
[31]Mauri L, Foster E, Glower DD, et al. 4-year results of a randomized controlled trial of percutaneous repair versus surgery for mitral regurgitation[J]. J Am Coll Cardiol,2013,62(4):317-328.
[32]Grasso C, Capodanno D, Scandura S, et al. One- and twelve-month safety and efficacy outcomes of patients undergoing edge-to-edge percutaneous mitral valve repair (from the GRASP Registry)[J]. Am J Cardiol, 2013,111(10):1482-1487.
[33]Maisano F, Franzen O, Baldus S, et al. Percutaneous mitral valve interventions in the real world: early and 1-year results from the ACCESS-EU, a prospective, multicenter, nonrandomized post-approval study of the MitraClip therapy in Europe[J]. J Am Coll Cardiol,2013,62(12):1052-1061.
[34]Rudolph V, Lubos E, Schluter M, et al. Aetiology of mitral regurgitation differentially affects 2-year adverse outcomes after MitraClip therapy in high-risk patients[J]. Eur J Heart Fail,2013,15(7):796-807.
[35]Schillinger W, Hunlich M, Baldus S, et al. Acute outcomes after MitraClip therapy in highly aged patients: results from the German TRAnscatheter Mitral valve Interventions (TRAMI) Registry[J]. EuroIntervention, 2013,9(1):84-90.
[36]Swaans MJ, Bakker AL, Alipour A, et al. Survival of transcatheter mitral valve repair compared with surgical and conservative treatment in high-surgical-risk patients[J]. JACC Cardiovasc Interv,2014,7(8):875-881.
[37]Taramasso M, Maisano F, Latib A, et al. Clinical outcomes of MitraClip for the treatment of functional mitral regurgitation[J]. EuroIntervention, 2014,10(6):746-752.
Recent Progress in Diagnosis and Treatment of Mitral Regurgitation
KAN Tong, QIN Yongwen
(DepartmentofCardiology,ChanghaiHospital,TheSecondMilitaryMedicalUniversity,Shanghai200433,China)
影响二尖瓣关闭功能的疾病都可以导致二尖瓣反流。轻度二尖瓣反流患者仅有轻微劳力性呼吸困难,重度二尖瓣反流症状严重,降低患者的生存时间。目前依据病因可将二尖瓣反流分为原发性二尖瓣反流和继发性二尖瓣反流,这两种二尖瓣反流有不同的诊断和治疗原则。现就二尖瓣反流的诊断治疗进展做一综述。
二尖瓣反流;二尖瓣;诊断;治疗结果
The diseases that affect the function of mitral valve can lead to mitral regurgitation (MR). The patients with mild MR can only feel mild exertional dyspnea and the patients with severe MR can feel severe symptoms, which reduces the patients’ survival time. Presently, MR is classified into primary and secondary entities based on the pathogen. The diagnosis and treatment of the primary and secondary MR are quite different. This paper aims to make a comprehensive review about the recent progress in diagnosis and treatment of MR.
mitral regurgitation; mitral valve; diagnosis; treatment outcome
阚通(1990—),在读硕士,主要从事心血管病介入治疗研究。Email: 871415868@qq.com
秦永文(1952—),主任医师,教授,博士,主要从事心血管病介入治疗研究。Email: chqinyw@163.com
1004-3934(2015)06-0686-05
R542.5
A
10.3969/j.issn.1004-3934.2015.06.008
2015-06-02
2015-07-21
