老年女性代谢综合征患者血清25-羟维生素D水平变化及临床意义研究
2015-02-21陈陵霞苗懿德
褚 琳,孙 芳,刘 杰,陈陵霞,苗懿德
·论著·
老年女性代谢综合征患者血清25-羟维生素D水平变化及临床意义研究
褚 琳,孙 芳,刘 杰,陈陵霞,苗懿德
目的 探讨老年女性患者25-羟维生素D〔25-(OH)VD〕水平与代谢综合征(MS)发生发展的相关性。方法 收集2011年9月—2013年11月于北京大学人民医院老年科住院的老年女性患者188例,年龄60~94岁,均为绝经后。按照有无MS将患者分为MS组(79例)和非MS组(109例);按照血清25-(OH)VD中位数(31.5 nmol/L)将患者分为<31.5 nmol/L组(94例)和≥31.5 nmol/L组(94例)。测量血压、身高、体质量、计算体质指数(BMI),并检测空腹血糖(FPG)、总胆固醇(TC)、三酰甘油(TG)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)、糖化血红蛋白(HbA1c)、空腹胰岛素(FINS)、血钙(Ca)、血磷(P)、血清25-(OH)VD、骨特异性碱性磷酸酶(BAP)和抗酒石酸酸性磷酸酶(TRAP)水平,计算胰岛素抵抗指数(HOMA-IR);比较MS组与非MS组血清25-(OH)VD缺乏程度;分析血清25-(OH)VD与观察指标的相关性。结果 MS组高血压病程、糖尿病病程、TG、HDL-C、FPG、HbA1c、FINS、HOMA-IR与非MS组比较,差异有统计学意义(P<0.05)。MS组患者血清25-(OH)VD水平低于非MS组(P<0.05)。<31.5 nmol/L组高血脂病程、TG、HDL-C、FPG、HbA1c、FINS、HOMA-IR与≥31.5 nmol/L组比较,差异有统计学意义(P<0.05)。≥31.5 nmol/L组患者血清25-(OH)VD水平高于<31.5 nmol/L组(P<0.05)。MS组与非MS组血清25-(OH)VD缺乏程度比较,差异有统计学意义(P<0.05)。血清25-(OH)VD水平与TG、FPG、HOMA-IR呈负相关,与HDL-C呈正相关(P<0.05)。结论 老年女性患者血清25-(OH)VD水平较低,且与血脂、血糖相关,为临床进一步研究提供了参考依据。
代谢综合征X;老年女性;维生素D
褚琳,孙芳,刘杰,等.老年女性代谢综合征患者血清25-羟维生素D水平变化及临床意义研究[J].中国全科医学,2015,18(12):1376-1381.[www.chinagp.net]
Chu L,Sun F,Liu J,et al.Changes of serum 25-hydrocyvitamin D level in elderly women with metabolic syndrome and its clinical significance[J].Chinese General Practice,2015,18(12):1376-1381.
中国一项大型研究发现,心血管疾病(cardiovascular disease,CVD)已成为女性死亡的首位原因[1]。有资料显示,绝经后女性CVD发生率较绝经前显著上升[2]。代谢综合征(metabolic syndrome,MS)是评价CVD高风险的重要指标。在亚洲,由于西化饮食的增加和活动减少,MS患者的数量正在显著增加[3-4]。MS的发生率在中青年人群中男性普遍高于女性,而这种性别差异在50岁以上人群中则不存在。研究表明,绝经后女性是MS的高危人群,绝经是MS的危险因素[5]。
近年来发现,维生素D缺乏可能与MS的发病风险升高相关[6-9]。有韩国研究表明,绝经后女性维生素D水平与血压、三酰甘油(TG)和高密度脂蛋白胆固醇(HDL-C)等MS组成部分相关[10]。目前国内尚无有关MS与绝经后妇女的血清维生素D缺乏的相关研究,为此笔者拟通过检测绝经后女性MS患者血清25-羟维生素D〔25-(OH)VD〕水平的变化,探讨其与MS的关系。
1 对象与方法
1.1 研究对象 收集2011年9月—2013年11月在北京大学人民医院老年科住院的老年女性患者188例,年龄60~94岁,平均(77.1±7.6)岁,均为绝经后。纳入标准:因2型糖尿病、高血压、冠状动脉粥样硬化性心脏病、慢性消化系统疾病、脑供血不足、腔隙性脑梗死等疾病入院的女性患者。排除标准:严重器质性内分泌疾病者,如甲状腺疾病、甲状旁腺功能亢进等;继发性高血压、恶性高血压者;严重肝、肾功能异常者;心脏瓣膜病、心肌疾病者;重度贫血、骨髓瘤等影响骨代谢疾病者;急性感染、恶性肿瘤者;肾切除或维持透析患者;服用活性维生素D药物,长期服用激素、免疫抑制剂,使用胰岛素等药物者。
1.2 方法
1.2.1 一般情况 详细询问患者病史,入院后检查血压〔收缩压(SBP),舒张压(DBP)〕、身高、体质量,计算体质指数(BMI)。
本文要点:
本研究表明在绝经后女性中,血清25-(OH)VD水平与MS具有一定相关性,提示维生素D缺乏可能在绝经后人群相关代谢异常以及CVD发病过程中起重要作用。这为指导绝经后女性合理补充维生素D提供了参考依据。
1.2.2 血液学指标检测 患者均清晨空腹采取静脉血2 ml,检测总胆固醇(TC)、TG、低密度脂蛋白胆固醇(LDL-C)、HDL-C、空腹血糖(FPG)、糖化血红蛋白(HbA1c)、血钙(Ca)、血磷(P)和空腹胰岛素(FINS)水平。测定血清25-(OH)VD、骨特异性碱性磷酸酶(BAP)、抗酒石酸酸性磷酸酶(TRAP)水平等骨转换生化指标,采用英国IDS公司试剂盒。血清25-(OH)VD的批内变异为5.6%,批间变异为7.3%。计算胰岛素抵抗指数(HOMA-IR)=FINS×FPG/22.5。
1.2.3 诊断标准及分组 MS诊断依照中华医学会糖尿病学分会2004年建议适合中国人群的诊断,具备以下4项中的3项及以上者:(1)超重和/或肥胖:BMI≥25.0 kg/m2;(2)高血糖:FPG≥6.1 mmol/L和/或餐后2 h血糖(2 hPG)≥7.8 mmol/L,和/或已确诊为糖尿病并治疗者;(3)高血压:SBP/DBP≥140/90 mm Hg(1 mm Hg =0.133 kPa),和/或已确诊为高血压并治疗者;(4)血脂紊乱:TG≥1.7 mmol/L和/或HDL-C<1.0 mmol/L(女)。血清25-(OH)VD水平分级标准:(1)缺乏〔25-(OH)VD≤50 nmol/L〕;(2)不足〔50 nmol/L<25-(OH)VD <75 nmol/L〕;(3)充足〔25-(OH)VD≥75 nmol/L〕[11]。按照有无MS将患者分为MS组(79例)和非MS组(109例);按照血清25-(OH)VD中位数(31.5 nmol/L)将患者分为<31.5 nmol/L组(94例)和≥31.5 nmol/L组(94例)。

2 结果
2.1 MS组与非MS组一般资料比较 MS组高血压病程、糖尿病病程、TG、HDL-C、FPG、HbA1c、FINS、HOMA-IR与非MS组比较,差异有统计学意义(P<0.05);其余各项指标比较,差异无统计学意义(P>0.05,见表1)。
2.2 MS组与非MS组骨生化指标比较 MS组患者血清25-(OH)VD水平低于非MS组,差异有统计学意义(P<0.05);其余指标比较,差异无统计学意义(P>0.05,见表2)。
2.3 <31.5 nmol/L组和≥31.5 nmol/L组一般资料比较 <31.5 nmol/L组高血脂病程、TG、HDL-C、FPG、HbA1c、FINS、HOMA-IR与≥31.5 nmol/L组比较,差异有统计学意义(P<0.05);其余指标比较,差异无统计学意义(P>0.05,见表3)。
2.4 <31.5 nmol/L组和≥31.5 nmol/L组骨生化指标比较 ≥31.5 nmol/L组患者血清25-(OH)VD水平高于<31.5 nmol/L组,差异有统计学意义(P<0.05);其余指标比较,差异无统计学意义(P>0.05,见表4)。

Table 2 Comparison of biomechanics index between the MS group and non-MS group

组别例数25-(OH)VD(nmol/L)TRAP(U/L)BAP(μg/L)Ca(mmol/L)P(mmol/L)非MS组10936.2±14.63.6±1.215.1±8.42.2±0.11.2±0.2MS组7932.8±12.03.6±1.415.5±6.12.2±0.11.2±0.2t值4.1200.2810.5261.5500.023P值0.0320.5970.4690.1190.881
注:25-(OH)VD=25-羟维生素D,TRAP=抗酒石酸酸性磷酸酶,BAP=骨特异性碱性磷酸酶,Ca=血钙,P=血磷

表1 MS组与非MS组一般资料比较
注:BMI=体质指数,TC=总胆固醇,LDL-C=低密度脂蛋白胆固醇,TG=三酰甘油,HDL-C=高密度脂蛋白胆固醇,FPG=空腹血糖,SBP=收缩压,DBP=舒张压,HbA1c=糖化血红蛋白,FINS=空腹胰岛素,HOMA-IR=胰岛素抵抗指数,MS=代谢综合征

表3 25-(OH)VD<31.5 nmol/L组和≥31.5 nmol/L组一般资料比较
2.5 MS组与非MS组血清25-(OH)VD缺乏程度比较 MS组与非MS组血清25-(OH)VD缺乏程度比较,差异有统计学意义(P<0.05,见表5)。
2.6 血清25-(OH)VD水平与观察指标的相关性分析 血清25-(OH)VD水平与TG、FPG、HOMA-IR呈负相关,与HDL-C呈正相关(P<0.05),与其余指标无相关关系(P>0.05,见表6)。

Table 4 Comparison of biomechanics index between the 25-(OH)VD <31.5 nmol/L group and ≥31.5 nmol/L group
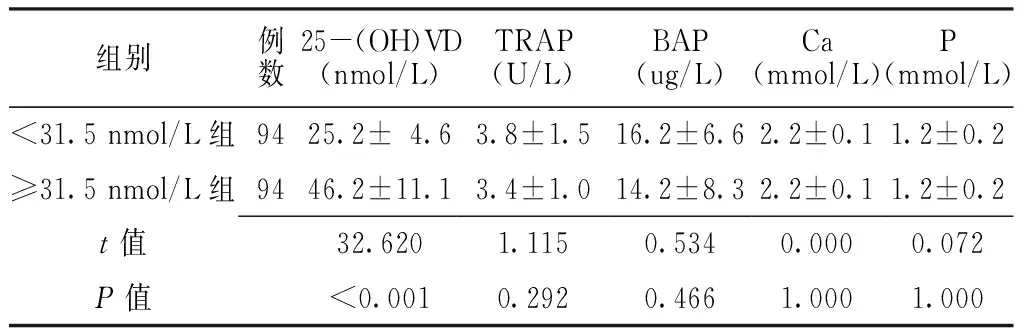
组别例数25-(OH)VD(nmol/L)TRAP(U/L)BAP(ug/L)Ca(mmol/L)P(mmol/L)<31.5nmol/L组9425.2±4.63.8±1.516.2±6.62.2±0.11.2±0.2≥31.5nmol/L组9446.2±11.13.4±1.014.2±8.32.2±0.11.2±0.2t值32.6201.1150.5340.0000.072P值<0.0010.2920.4661.0001.000
表5 MS组与非MS组血清25-(OH)VD缺乏程度比较〔n(%)〕
Table 5 Comparison of 25-(OH)VD level between the MS group and non-MS group

组别例数缺乏不足充足非MS组10979(72.5)25(22.9)5(4.6)MS组 79 69(87.3)9(11.4)1(1.3)u值-2.481P值 0.013
表6 血清25-(OH)VD水平与观察指标的相关性分析
Table 6 Correlation between serum 25-(OH) VD level and observation index

指标r值P值年龄-0.1300.075BMI-0.0580.681高血脂病程-0.1250.315高血压病程-0.0920.217糖尿病病程-0.0270.711TC-0.1490.061LDL-C-0.1300.074TG-0.2500.015HDL-C0.2260.018FPG-0.1680.034SBP-0.0840.684DBP0.0590.354HbA1c0.1050.191FINS-0.0780.668HOMA-IR-0.1520.042
3 讨论
MS指一组由遗传和环境因素共同作用引起的多代谢异常性疾病,表现为肥胖、血压升高、血脂和血糖异常。围绝经期及绝经后血清性激素水平的变化,引起了围绝经期的一系列症状,也使得MS的患病率较绝经前明显增加。绝经后女性MS患病率高达32.6%~37.3%[12-13],且其CVD的发病风险明显增加[14]。绝经后肥胖导致日益加重的胰岛素抵抗,可能是绝经后女性MS发病风险增高的关键因素[15]。Kip等[16]研究发现,在女性人群中,MS而不是BMI预测了CVD的危险性。
维生素D是一种脂溶性维生素。由于25-(OH)VD在血中水平相对较高,t1/2较长,因此一般认为临床可以通过测定血清25-(OH)VD的水平来了解体内维生素D的营养状况[8]。近年来发现,维生素D缺乏可能增加MS的发病风险[6-9,17]。有研究表明,绝经后女性MS组维生素D水平与血压、TG和HDL-C等相关[10]。本研究结果显示,绝经后女性MS组患者25-(OH)VD水平低于非MS组,表明血清25-(OH)VD与MS具有一定相关性。
多项研究表明,血清维生素D水平与2型糖尿病的发病率呈负相关[18-21]。并有研究发现,短期补充维生素D能够改善胰岛β细胞功能,从而降低HbA1c的上升幅度[22-24]。同时,胰岛素抵抗在糖尿病发生、发展中起着重要作用。多项研究表明,当血清维生素D水平从缺乏补充至充足时,其胰岛素敏感性将会明显升高,甚至在提高胰岛素敏感性上明显优于曲格列酮及二甲双胍[23,25-26]。本研究发现,绝经后女性25-(OH)VD与FPG、HOMA-IR相关,与上述研究结论相似。
研究发现,绝经后女性TG水平较绝经前女性明显升高[27]。同时,绝经后HDL-C水平的下降被认为会降低其心血管保护作用[28]。虽然维生素D与血脂异常间的关系尚未完全阐明,但有动物研究报道,血清维生素D水平与HDL-C呈正相关,较低的维生素D与冠状动脉粥样硬化的主要危险因子相关[29]。本研究发现,绝经后女性血清25-(OH)VD与TG呈负相关,与HDL-C呈正相关,提示维生素D缺乏可能在绝经后人群相关代谢异常以及CVD发病过程中起重要作用。
有研究发现,血压控制水平与血清25-(OH)VD水平有关[30-32]。但本研究未发现血压水平与25-(OH)VD相关,可能由于本研究患者均为城市中离退休高级干部,良好的医疗保健水平使得其血压受到了较好的控制。
绝经被认为会增加中心性肥胖[27],同时,绝经后女性BMI、腰围也较绝经前明显增加[33]。欧美有研究发现,血清维生素D水平与体脂百分比、BMI、腰围等指标呈负相关[34-35],维生素D增加了肥胖的发病风险[36]。本研究尚未发现BMI与25-(OH)VD相关,与韩国研究结论相似[10]。考虑其可能与亚洲人体型较小、BMI波动区间较小有关。
老年人皮肤维生素D产生减少[37],因此常认为维生素D的减少与年龄相关。但是,本研究中并未发现血清25-(OH)VD水平与年龄相关。这一现象可能与年龄相关的肾功能降低有关。动物研究表明,随着鼠龄增加引起肾功能的下降,其代谢清除25-(OH)VD的能力也随之下降[38]。因此,随着年龄增加皮肤产生的维生素D减少,但同时肾脏对于25-(OH)VD的利用也减少;这些效应相互抵消,导致血清25-(OH)VD并未受到年龄的显著影响。
维生素D缺乏已成为全球性问题,并且日益严重[39]。当体内维生素D不足时,不仅会引起骨密度下降、骨折发生率明显增加[40],而且可导致微生物感染、代谢性疾病和CVD的发病率和病死率明显升高[41-42]。国内研究发现,我国老年人维生素D整体水平减低,维生素D缺乏者约占69.2%[8]。本研究发现,绝经后女性维生素D缺乏率为78.7%,明显高于我国普通老年人;在绝经后MS患者中,维生素D缺乏率甚至高达87.3%。VD缺乏普遍存在于老年女性患者中,考虑可能与其户外活动较少、受太阳照射时间减少、肝肾功能生理性减退及消化道对于营养吸收较差有关。此外,随年龄增加使肥胖者脂溶性维生素D分布容积增加,生物活性下降,也导致维生素D水平下降。提示对于绝经后女性特别是合并MS者,适当增加阳光照射或者补充维生素D类似物有益健康。
综上所述,本研究表明在绝经后女性中,血清25-(OH)VD与MS具有一定相关性,提示维生素D缺乏可能在绝经后人群相关代谢异常以及CVD发病过程中起重要作用。这为指导绝经后女性合理补充维生素D提供依据与参考。本研究样本量较少,其结论需要扩大样本量的重复研究来进一步证实。
[1]He J,Gu D,Wu X,et al.Major causes of death among men and women in China[J].N Engl J Med,2005,353(11):1124-1134.
[2]Collins P,Rosano G,Casey C,et al.Management of cardiovascular risk in the peri-menopausal women:a consensus statement of European cardiologists and gynaecologists[J].Eur Heart J,2007,28(16):2028-2040.
[3]Freeman MS,Mansfield MW,Barrett JH,et al.Insulin resistance:an atherothrombotic syndrome.The Leeds family study[J].Thromb Haemost,2003,89(1):161-168.
[4]Lim S,Park KS,Lee HK,et al.Changes in the characteristics of metabolic syndrome in Korea over the period 1998—2001 as determined by Korean National Health and Nutrition Examination Surveys[J].Diabetes Care,2005,28(7):1810-1812.
[5]Lin KC,Tsai ST,Kuo SC,et al.Interrelationship between insulin resistance and menopause on the metabolic syndrome and its individual component among nondiabetic women in the kinmen study[J].Am J Med Sci,2007,333(4):208-214.
[6]Hyppönen E,Boucher BJ,Berry DJ,et al.25-hydroxyvitamin D,IGF-1,and metabolic syndrome at 45 years of age:a cross-sectional study in the 1958 British Birth Cohort[J].Diabetes,2008,57(2):298-305.
[7]Ford ES,Ajani UA,McGuire LC,et al.Concentrations of serum vitamin D and the metabolic syndrome among US adults[J].Diabetes Care,2005,28(5):1228-1230.
[8]Lu L,Yu Z,Pan A,et al.Plasma 25-hydroxyvitamin D concentration and metabolic syndrome among middle-aged and elderly Chinese individuals[J].Diabetes Care,2009,32(7):1278-1283.
[9]Kayaniyil S,Vieth R,Harris SB,et al.Association of 25(OH)D and PTH with metabolic syndrome and its traditional and nontraditional components[J].J Clin Endocrinol Metab,2011,96(1):168-175.
[10]Chon SJ,Yun BH,Jung YS,et al.Association between vitamin D status and risk of metabolic syndrome among Korean postmenopausal women[J].PLoS One,2014,9(2):e89721.
[11]Howe WR,Dellavalle R.Vitamin D deficiency[J].N Engl J Med,2007,357(19):1981.
[12]Ding QF,Hayashi T,Zhang XJ,et al.Risks of CHD identified by different criteria of metabolic syndrome and related changes of adipocytokines in elderly postmenopausal women[J].J Diabetes Complications,2007,21(5):315-319.
[13]Ponholzer A,Temml C,Rauchenwald M,et al.Is the metabolic syndrome a risk factor for female sexual dysfunction in sexually active women?[J].Int J Impot Res,2008,20(1):100-104.
[14]Rossi R,Nuzzo A,Origliani G,et al.Metabolic syndrome affects cardiovascular risk profile and response to treatment in hypertensive postmenopausal women[J].Hypertension,2008,52(5):865-872.
[15]Gaspard U.Hyperinsulinaemia,a key factor of the metabolic syndrome in postmenopausal women[J].Maturitas,2009,62(4):362-365.
[16]Kip KE,Marroquin OC,Kelley DE,et al.Clinical importance of obesity versus the metabolic syndrome in cardiovascular risk in women:a report from the Women′s Ischemia Syndrome Evaluation(WISE) study[J].Circulation,2004,109(6):706-713.
[17]Cheng S,Massaro JM,Fox CS,et al.Adiposity,cardiometabolic risk,and vitamin D status:the Framingham Heart Study[J].Diabetes,2010,59(1):242-248.
[18]Hurskainen AR,Virtanen JK,Tuomainen TP,et al.Association of serum 25-hydroxyvitamin D with type 2 diabetes and markers of insulin resistance in a general older population in Finland[J].Diabetes Metab Res Rev,2012,28(5):418-423.
[19]Staeva-Vieira T,Peakman M,von Herrath M.Translational mini-review series on type 1 diabetes:Immune-based therapeutic approaches for type 1 diabetes[J].Clin Exp Immunol,2007,148(1):17-31.
[20]Liu S,Song Y,Ford ES,et al.Dietary caldum,vitamin D,and the prevalence of metabolic syndrome in middle-aged and older U.S.women[J].Diabetes Care,2005,28(12):2926-2932.
[21]González-Molero I,Rojo-Martínez G,Morcillo S,et al.Vitamin D and incidence of diabetes:a prospective cohort study[J].Clin Nutr,2012,31(4):571-573.
[22]Zittermann A,Frisch S,Berthold HK,et al.Vitamin D supple-mentation enhances the beneficial effects of weight 1088 on cardiovascular disease risk markers[J].Am J Clin Nutr,2009,89(5):1321-1327.
[23]von Hurst PR,Stonehouse W,Coad J.Vitamin D supplemen-ration reduces insulin resistance in South Asian women living in New Zealand who are insulin resistant and vitamin D defident-a randomised,placebo-controlled trial[J].Br J Nutr,2010,103(4):549-555.
[24]Shab-Bidar S,Neyestani TR,Djazayery A,et al.Regular consumption of vitamin D-fortified yogurt drink(Doogh) improved endothelial biomarkers in subjects with type 2 diabetes:a randomized double-blind clinical trial[J].BMC Med,2011(9):125.
[25]Aljabri KS,Bokhari SA,Khan MJ.Glycemic changes after vitamin D supplementation in patients with type 1 diabetes mellitus and vitamin D deficiency[J].Ann Saudi Med,2010,30(6):454-458.
[26]Inzucchi SE,Maggs DG,Spollett GR.Icacy and metabolic effects of metformin and troglitazone in type Ⅱ diabetes mellitus[J].N Engl J Med,1998,338(13):867-872.
[27]Dayspring TD.Understanding hypertriglyceridemia in women:clinical impact and management with prescription omega-3-acid ethyl esters[J].Int J Womens Health,2011(3):87-97.
[28]Mascarenhas-Melo F,Sereno J,Teixeira-Lemos E,et al.Markers of increased cardiovascular risk in postmenopausal women:focus on oxidized-LDL and HDL subpopulations[J].Dis Markers,2013,35(2):85-96.
[29]Schnatz PF,Nudy M,O′Sullivan DM,et al.Identification of a mechanism for increased cardiovascular risk among individuals with low vitamin D concentrations[J].Menopause,2011,18(9):994-1000.
[30]Snijder MB,Lips P,Seidell JC,et al.Vitamin D status and parathyroid hormone levels in relation to blood pressure:a population-based study in older men and women[J].J Intern Med,2007,261(6):558-565.
[31]Hintzpeter B,Mensink GB,Thierfelder W,et al.Vitamin D status and health correlates among German adults[J].Eur J Clin Nutr,2008,62(9):1079-1089.
[32]Scragg R,Sowers M,Bell C.Serum 25-hydroxyvitamin D,ethnicity,and blood pressure in the Third National Health and Nutrition Examination Survey[J].Am J Hypertens,2007,20(7):713-719.
[33]Stoney CM,Owens JF,Guzick DS,et al.A natural experiment on the effects of ovarian hormones on cardiovascular risk factors and stress reactivity:bilateral salpingo oophorectomy versus hysterectomy only[J].Health Psychol,1997,16(4):349-358.
[34]Arunabh S,Pollack S,Yeh J,et al.Body fat content and 25-hydroxyvitamin D levels in Healthy women[J].J Clin Endocrinol Metab,2003,88(1):157-161.
[35]Wortsman J,Matsuoka LY,Chen TC,et al.Decreased bioavailability of vitamin D in obesity[J].Am J Clin Nutr,2000,72(3):690-693.
[36]González-Molero I,Rojo-Martínez G,Morcillo S,et al.Hypovitaminosis D and incidence of obesity:a prospective study[J].Eur J Clin Nutr,2013,67(6):680-682.
[37]Holick MF.Vitamin D:importance in the prevention of cancers,type 1 diabetes,heart disease,and osteoporosis[J].Am J Clin Nutr,2004,79(3):362-371.
[38]Matsuura F,Wang N,Chen W,et al.HDL from CETP-deficient subjects shows enhanced ability to promote cholesterol efflux from macrophages in an apoE-and ABCG1-dependent pathway[J].J Clin Invest,2006,116(5):1435-1442.
[39]van Schoor NM,Lips P.Worldwide vitamin D status[J].Best Pract Res Clin Endocrinol Metab,2011,25(4):671-680.
[40]Melhus H,Snellman G,Gedeborg R,et al.Plasma 25-hydroxyvitamin D levels and fracture risk in a community-based cohort of elderly men in Sweden[J].J Clin Endocrinol Metab,2010,95(6):2637-2645.
[41]Pilz S,Dobnig H,Tomaschitz A,et al.Low 25-hydroxyvitamin D is associated with increased mortality in female nursing home residents[J].J Clin Endocrinol Metab,2012,97(4):E653-657.
[42]Joergensen C,Reinhard H,Schmedes A,et al.Vitamin D levels and asymptomatic coronary artery disease in type 2 diabetic patients with elevated urinary albumin excretion rate[J].Diabetes Care,2012,35(1):168-172.
(本文编辑:李婷婷)
Changes of Serum 25-hydrocyvitamin D Level in Elderly Women With Metabolic Syndrome and Its Clinical Significance
CHULin,SUNFang,LIUJie,etal.
DepartmentofGeriatrics,PekingUniversityPeople′sHospital,Beijing100044,China
Objective To investigate the relationship between serum 25-hydrocyvitamin D〔25-(OH)VD〕evel and occurrence of metabolic syndrome(MS) in elderly women.Methods 188 elderly post-menopausal female patients(60-94 years old) who were admitted to the department of geriatrics of Peking University People′s Hospital from September 2011 to November 2013,were selected as study subjects.79 cases with MS were included in MS group,109 without MS were included in non-MS group.According to the median serum 25-(OH)VD level(31.5 nmol/L),94 cases were included in <31.5 nmol/L group,94 cases were included in ≥31.5 nmol/L group.Blood pressure,body weight,body height,body mass index(BMI) were measured and calculated.Serum levels of fasting plasma glucose(FPG),total cholesterol(TC),triglycerides(TG),low-density lipoprotein cholesterol(LDL-C),high-density lipoprotein cholesterol(HDL-C),glycosylated hemoglobin(HbA1c),serum fasting insulin(FINS),calcium(Ca),phosphorus(P),25-(OH)VD,bone-specific alkaline phosphatase(BAP) and tartaric-resistant phosphatase(TRAP) were measured.The degree of 25-(OH)VD deficiency was compared between MS group and non-MS group,the correlation between serum level of 25-(OH)VD and observation indicators was analyzed.Results There were significant differences in duration of hypertension and diabetes,levels of TG,HDL-C,FPG,HbA1c,FINS and HOMA-IR between MS group and non-MS group(P<0.05).Serum level of 25-(OH)VD in MS group was significantly lower than that in non-MS group(P<0.05).There were significant differences in duration of hyperlipidemia,levels of TG,HDL-C,FPG,HbA1c,FINS and HOMA-IR between <31.5 nmol/L group and ≥31.5 nmol/L group(P<0.05).Serum level of 25-(OH)VD in ≥31.5 nmol/L group was significantly higher than that in <31.5 nmol/L group(P<0.05).There was significant difference in degree of 25-(OH)VD deficiency between MS group and non-MS group(P<0.05).Serum level of 25-(OH)VD was negatively correlated with level of TG,FPG and HOMA-IR,respectively,but was positively correlated with level of HDL-C(P<0.05).Conclusion Serum level of 25-(OH)VD is relatively low in elderly women and is related to levels of blood lipid and FPG.
Metabolic syndrome X;Elderly women;Vitamin D
100044 北京市,北京大学人民医院老年科
刘杰,100044 北京市,北京大学人民医院老年科;E-mail:doctortruly@163.com
R 589
A
10.3969/j.issn.1007-9572.2015.12.006
2014-07-21;
2014-11-21)
