HIV感染者围术期发生脓毒症的临床特点及乌司他丁治疗效果分析
2015-02-21黄朝刚刘保池
黄朝刚,李 垒,刘保池
·短篇论著·
HIV感染者围术期发生脓毒症的临床特点及乌司他丁治疗效果分析
黄朝刚,李 垒,刘保池

HIV;脓毒症;感染;乌司他丁
黄朝刚,李垒,刘保池.HIV感染者围术期发生脓毒症的临床特点及乌司他丁治疗效果分析[J].中国全科医学,2015,18(11):1330-1332,1336.[www.chinagp.net]
Huang CG,Li L,Liu BC.Clinical characteristics of sepsis of HIV-infected patients in perioperative period and treatment effect of ulinastatin[J].Chinese General Practice,2015,18(11):1330-1332,1336.
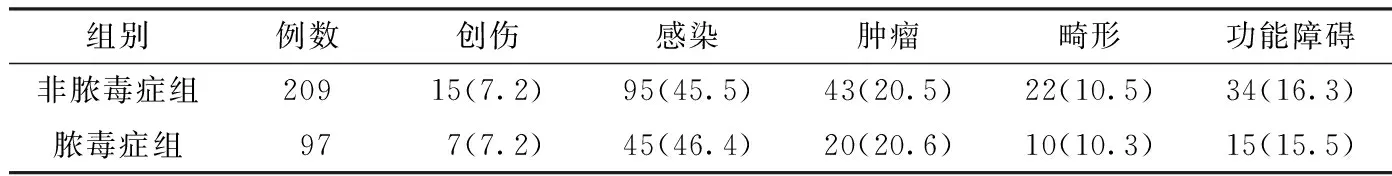
表1 脓毒症组和非脓毒症组患者外科疾病构成比较〔n(%)〕
表4 乌司他丁亚组与对照亚组术前、术后体温比较〔℃,M(P25,P75)〕
Table 4 Comparison of preoperative and postoperative body temperature between the ulinastatin group and the control group
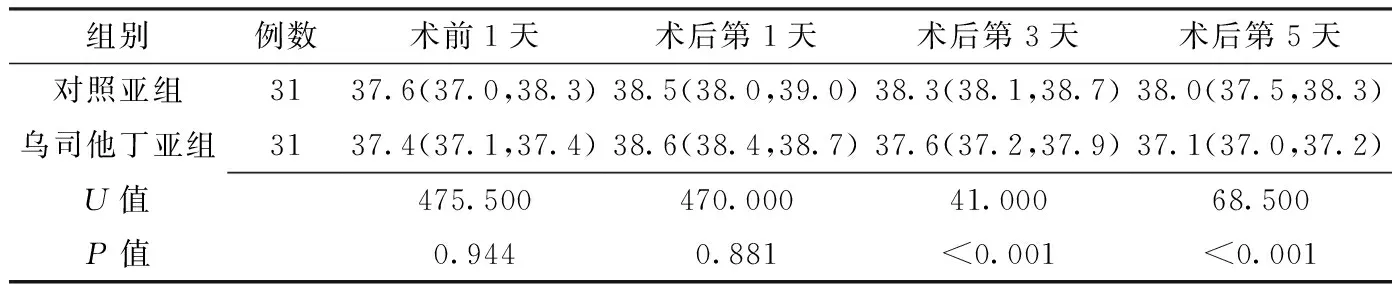
组别例数术前1天术后第1天术后第3天术后第5天对照亚组3137.6(37.0,38.3)38.5(38.0,39.0)38.3(38.1,38.7)38.0(37.5,38.3)乌司他丁亚组3137.4(37.1,37.4)38.6(38.4,38.7)37.6(37.2,37.9)37.1(37.0,37.2)U值475.500470.00041.00068.500P值0.9440.881<0.001<0.001
临床上已有较多关于乌司他丁治疗脓毒症的报道,但关于HIV感染者术后脓毒症治疗的研究较少。本研究对上海市公共卫生临床中心外科HIV感染者的围术期临床资料进行回顾性分析,探讨乌司他丁对HIV感染者术后脓毒症的治疗效果。
1 资料与方法
1.1 临床资料 对2012年1月—2013年12月上海市公共卫生临床中心外科诊治的306例HIV感染者围术期的临床资料进行分析。患者男263例、女43例,年龄17~74岁,平均(42.0±12.3)岁。患者均在当地疾病控制与预防中心(CDC)确诊为HIV感染,因合并不同的外科疾病需行手术治疗。
2 结果

2.2 乌司他丁亚组和对照亚组资料比较 从脓毒症组患者中随机抽取62例,分为乌司他丁亚组(31例)和对照亚组(31例)。乌司他丁亚组患者在综合性抗感染治疗的基础上加用乌司他丁治疗,20万U,2次/d,静脉滴注,连用5 d;对照亚组31例行综合性抗感染治疗。两亚组患者术前临床资料间差异无统计学意义(P>0.05,见表3)。

3 讨论
3.1 HIV感染者脓毒症发生率 HIV感染者可能合并各种外科疾病需行手术治疗。本研究回顾性分析了2012年1月—2013年12月在上海市公共卫生临床中心行外科治疗的HIV感染患者的临床资料。HIV感染患者由于免疫功能低下,术后容易发生脓毒症[3-4]。Deneve等[5]报道了11年中对77例HIV感染者行腹部手术,术后感染发生率为55%,术后30 d内病死率为30%。本研究在2年中306例HIV感染者行手术治疗,术后脓毒症发生率为31.7%;2例术后30 d内死亡,病死率为0.65%;手术并发症和病死率明显低于有关报道[5-7]。


表2 脓毒症组和非脓毒症组临床资料比较〔M(P25,P75)〕

表3 乌司他丁亚组与对照亚组术前临床资料比较〔M(P25,P75)〕
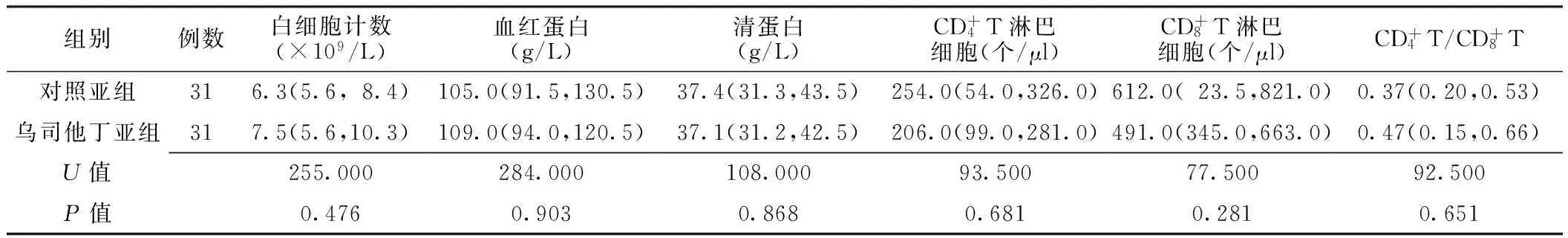
表5 乌司他丁亚组与对照亚组出院前临床指标比较〔M(P25,P75)〕

HIV感染者合并的机会性感染,比普通感染更难控制[8,11-13]。针对HIV感染患者,在外科手术清除主要病灶的基础上,除抗病毒治疗、抗结核或抗真菌治疗外,还需一般的抗感染治疗(至少1种抗生素)、非特异性抗感染治疗及营养支持等。外科医生需要掌握手术及围术期治疗的技巧,缩短HIV感染者住院时间,减轻患者的病痛及经济负担。
[1]Levy MM,Fink MP,Marshall JC,et al.2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference[J].Crit Care Med,2003,31(4):1250-1256.
[2]Kedir M.Seroprevalence,pattern and outcome of HIV/AIDS among surgical patients at Gondar University Hospital[J].Ethiop Med J,2008,46(1):15-18.
[3]Jacob ST,Moore CC,Banura P,et al.Severe sepsis in two Ugandan hospitals: a prospective observational study of management and outcomes in a predominantly HIV-1 infected population[J].PLoS One,2009,4(11):e7782.
[4]Stock PG,Barin B,Murphy B,et al.Outcomes of kidney transplantation in HIV-infected recipients[J].N Engl J Med,2010,363(21):2004-2014.
[5]Deneve JL,Shantha JG,Page AJ,et al.CD4count is predictive of outcome in HIV-positive patients undergoing abdominal operations[J].Am J Surg,2010,200(6):694-699.
[6]Owens CD,Stoessel K.Surgical site infections: epidemiology,microbiology and prevention[J].J Hosp Infect,2008,70(Suppl 2):3-10.
[7]Moore CC,Jacob ST,Pinkerton R,et al.Point-of-care lactate testing predicts mortality of severe sepsis in a predominantly HIV type 1-infected patient population in Uganda[J].Clin Infect Dis,2008,46(2):215-222.
[8]Su J,Tsun A,Zhang L,et al.Preoperative risk factors influencing the incidence of postoperative sepsis in human immunodeficiency virus-infected patients: a retrospective cohort study[J].World J Surg,2013,37(4):774-779.
[9]Qin QQ,Wang L,Ding ZW,et al.Situation on HIV/AIDS epidemics among migrant population in China,2008—2011[J].Zhonghua Liu Xing Bing Xue Za Zhi,2013,34(1):41-43.
[10]Deziel DJ,Hyser MJ,Doolas A,et al.Major abdominal operations in acquired immunodeficiency syndrome[J].Am Surg,1990,56(7):445-450.
[11]Zhang L,Liu BC,Zhang XY,et al.Prevention and treatment of surgical site infection in HIV-infected patients[J].BMC Infect Dis,2012,12:115.
[12]Mestres CA,Chuquiure JE,Claramonte X,et al.Long-term results after cardiac surgery in patients infected with the human immunodeficiency virus type-1(HIV-1)[J].Eur J Cardiothorac Surg,2003,23(6):1007-1016.
[13]Okumu G,Makobore P,Kaggwa S,et al.Effect of emergency major abdominal surgery on CD4cell count among HIV positive patients in a sub-Saharan Africa tertiary hospital——a prospective study[J].BMC Surg,2013,13:4.
修回日期:2015-03-10)
(本文编辑:赵跃翠)
Clinical Characteristics of Sepsis of HIV-infected Patients in Perioperative Period and Treatment Effect of Ulinastatin
HUANGChao-gang,LILei,LIUBao-chi.
DepartmentofSurgery,ShanghaiPublicHealthClinicalClinicalClinicalCenter,Shanghai201508,China
Objective To analyse the clinical characteristics of sepsis in HIV-infected patients in the perioperative period and the effect of ulinastatin on the treatment of sepsis.Methods A retrospective study was conducted on the clinical data of 306 HIV-infected patients who received sugical treatment in the Department of Surgery of Shanghai Public Health Clinical Center from January 2012 to December 2013.According to the occurrence of perioperative sepsis,the patients were divided into sepsis group and non-sepsis group.A series of preoperative indicators were reviewed,including immunological indicators(T lymphocytes,T lymphocytes and),white blood cell,hemoglobin and albumin..In the sepsis group,31 patients who received comprehensive anti-infection treatment combined with ulinastatin were assigned into ulinastatin group and 31 patients who only received comprehensive anti-infection treatment were assigned into control group;the treatment effects of the two groups were compared.Results The incidence of postoperative sepsis was 31.7%(97/306).The sepsis group was lower(P<0.05)than non-sepsis group in preoperative indicators includingT lymphocytes,T lymphocytes,hemoglobin and albumin.The patients in the ulinastatin subgroup had lower (P<0.05) body temperature on day 3 and 5 after operation,compared with the control subgroup; the ulinastatin subgroup was significant different from the control subgroup in the average length of hospital stay 〔( 14.6 ± 2.6) dvs.( 16.2 ± 2.3) d,t = 2.566,P = 0.013〕; either subgroup had one case of death; the two subgroups had no sigficantly difference (P>0.05) in the results ofT lymphocytes,T lymphocytes,,and blood routine reexamination before discharge.Conclusion HIV-infected patients have high incidence of postoperative sepsis. Decrease in preoperative level ofT lymphocytes,,hemoglobin and albumin has correlation with the incidence of postoperative sepsis.Comprehensive anti-infection treatment combined with auxiliary application of ulinastatin may control the systemic inflammatory response and reduce the length of hospital stay.
HIV;Sepsis;Infection;Ulinastatin
201508上海市公共卫生临床中心外科
刘保池,201508上海市公共卫生临床中心外科;E-mail:liubaochi@shaphc.org
R 631
B
10.3969/j.issn.1007-9572.2015.11.025
2014-10-20;
