Conjunctival Langerhans Cell Histiocytosis: a Case Report
2015-01-09
Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
Conjunctival Langerhans Cell Histiocytosis: a Case Report
Di Chen and Han-yi Min*
Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
Langerhans cell histiocytosis; conjunctiva; immunohistochemistry
Chin Med Sci J 2015; 30(1):63-64
L ANGERHANS cell histiocytosis (LCH) is a rare disease, mainly involving the bone, skin, lung, liver, spleen, and skin.1The heterogenenous nature of LCH makes it difficult to diagnose. Not only do the involved organs vary from case to case, but also its natural history. Herein, we describe a rare case of conjuctival LCH in an Asian woman.
CASE DESCRIPTION
A 47-year-old Asian female complained about conjunctival injection and red nodules of her both eyes for 4 months. On examination, the best-corrected visual acuity was 20/50 in the right eye and 20/30 in the left eye. Physical examination revealed diffuse conjunctival injection and smooth solid red nodules beneath the superior bulbar conjunctiva of her both eyes (Fig. 1A). The cornea was clear with medium-sized grey keratic precipitates (Fig. 1B). The erythrocyte sedimentation rate (ESR) and angiotensinconverting enzyme (ACE) value were all within normal limits. The rheumatoid factor (RF) and anti-nuclear antibody (ANA) were also negative. The nodule biopsy was performed to determine the diagnosis, which showed hyperplasia of histiocytes with massive plasma cells and lymphocytes infiltration (Fig. 1C). Polymorphic giant cells could be seen (Fig. 1D). Immunohistochemical study revealed CD34 (-), S-100 (+) (Fig. 1E), and CD68 (++) (Fig. 1F). These findings were consistent with Langerhans cell histiocytosis (LCH). And the final diagnosis of conjunctival LCH was made.
Systemic therapy of prednisone 1 mg/kg along with cyclosporine A and cyclophosphamide was initiated. After one month’s treatment, the conjunctival injection disappeared and the patient’s visual acuity returned to 20/20 in the right eye and 20/15 in the left eye. The prednisone was gradually tapered down. The patient had been followed up for two years and there was no sign of recurrence.
DISCUSSION
LCH is characterized by the infiltration of pathogenic Langerhans cells.1The etiology of the rare disease is unknown. The ocular LCH mainly involves the orbit.2It has been occasionally reported LCH could induce uveitis, retinal vasculitis, and choroidal tumor,3but the conjunctival LCH has never been reported before. The diagnosis of LCH is largely dependent upon immunohisto- chemical stains.4
The treatment of LCH remains controversial. The choice of treatment depends on the location of the lesions and the degree of local destruction.1As for this case, thedisease had affected the patient’s visual acuity, which made systemic therapy necessary. After correct diagnosis and effective treatment, the patient had recovered well.
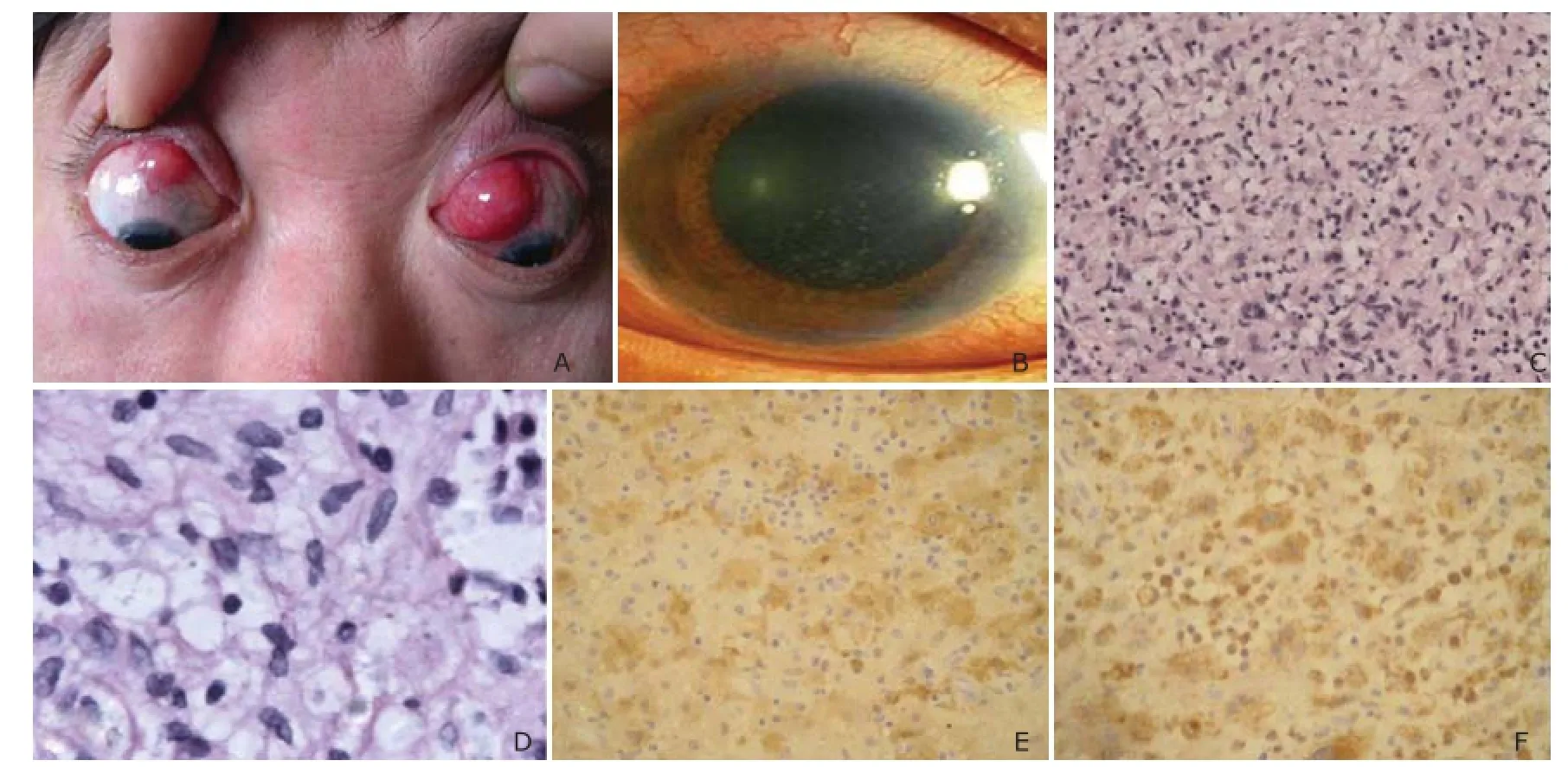
Figure 1.A 47-year-old woman with conjunctival Langerhans cell histiocytosis.
REFERENCES
1. Donadieu J, Chalard F, Jeziorski E, et al. Medical management of Langerhans cell histiocytosis from diagnosis to treatment. Expert Opin Pharmacother 2012; 106:1309-22.
2. Cheung N, Selva D, McNab AA, et al. Orbital Langerhans cell histiocytosis in adults. Ophthalmology 2007; 114:1569-73.
3. Kim IT, Lee SM. Choroidal Langerhans’ cell histiocytosis. Acta Ophthalmol Scand 2000; 78:97-100.
4. Crooks B, Grenier D. Langerhans cell histiocytosis: A complex recurrent disease. Paediatr Child Health 2010; 15:69-70.
for publication June 12, 2014.
Tel: 86-10-69156351, E-mail: wredge@sohu. com
杂志排行
Chinese Medical Sciences Journal的其它文章
- Use of Cataract Surgery in Urban Beijing: a Post Screening Follow-up of the Elderly with Visual Impairment due to Age-related Cataract
- Lipopolysaccharide Challenge Induces Long Pentraxin 3 Expression in Mice Independently from Acute Lung Injury△
- Reliability of a Novel Cobb Protractor for Measuring the Cobb Angle of Radiograph in Scoliosis
- Role of Removing Stasis and Reducing Heat Formula in Clearance of Proximal Ureteral Calculi after Ureteroscopic Ho:YAG Laser Lithotripsy: A Prospective Randomized Study
- Redo Coronary Artery Bypass Grafting: On-Pump and Off-Pump Coronary Artery Bypass Grafting Revascularization Techniques
- MRI Evaluation of Lateral Geniculate Body in Normal Aging Brain Using Quantitative Susceptibility Mapping.△
