七氟烷-咪达唑仑-瑞芬太尼麻醉诱导用于短小手术患儿无肌松药气管插管的效果
2014-08-02尹彩星司小萌
尹彩星,司小萌
七氟烷-咪达唑仑-瑞芬太尼麻醉诱导用于短小手术患儿无肌松药气管插管的效果
尹彩星,司小萌
目的 分析七氟烷-咪达唑仑-瑞芬太尼麻醉诱导用于短小手术患儿无肌松药气管插管的效果。方法 40例择期手术全麻患儿,美国麻醉师协会(American Society of Anesthesiologists,ASA)评分Ⅰ~Ⅱ级。麻醉诱导:静脉注射咪达唑仑0.03 mg/kg,面罩吸入6%七氟烷,每15 s递减0.5%,直至3%,待患儿睫毛反射消失时,1 min内缓慢静脉注射瑞芬太尼2 μg/kg,30 s后停止吸入七氟烷,气管插管后行机械通气。于麻醉诱导前、气管插管后即刻和插管后3 min,记录平均动脉压(mean artery pressure,MAP)、心率(heart rate,HR)、脉搏血氧饱和度(pulse oxygen saturation,SpO2)和脑电双频指数(bispectral index,BIS),记录患者睫毛反射消失时间,评价气管插管条件。结果 所有患儿睫毛反射消失时间为(58±10)s,气管插管条件优良率94%。与麻醉诱导前比较,气管插管后3 min MAP降低(P=0.045),气管插管后即刻、气管插管后3 min HR(P=0.038,P=0.030),BIS(P=0.012,P=0.009)明显降低。结论 七氟烷-咪达唑仑-瑞芬太尼麻醉诱导迅速而平稳,可提供良好的气管插管条件,对于短小手术患儿无肌松药气管插管,安全可行。
七氟烷;咪达唑仑;瑞芬太尼;气管插管;小儿短小手术
小儿短小手术主要包括急性阑尾炎、斜疝、肠套叠、睾丸鞘膜积液、隐睾、唇腭裂修复术等,多因患儿年龄较小不能配合而在全麻下完成,具有手术量多、手术及麻醉时间较短、所需麻醉药品剂量较小、呼吸道梗阻发生率高等特点,因此需要对患儿实施气管插管,且要求患儿术后快速苏醒,较少麻醉药残余,以降低呼吸道梗阻的发生率。因此,对于小儿短小手术要选择起效快和恢复快的麻醉药物,而建立无肌松药的麻醉诱导有重要意义。七氟烷血/气分配系数低,具有诱导迅速、苏醒快、可控性好及无刺激性气味等特点。本研究拟评价七氟烷-咪达唑仑-瑞芬太尼麻醉诱导用于短小手术患儿无肌松气管插管的效果。
1 对象与方法
1.1 对象 随机选取我院2013-08至2014-01小儿外科择期全麻手术患儿40例,其中男29例,女11例,年龄0.5~3岁,体重5~17 kg,ASAⅠ~Ⅱ级。
1.2 麻醉方法及观察指标 患儿入室后建立静脉通路,常规监测ECG、MAP、HR和SpO2,使用A-2000TM型脑电监测仪(美国Aspect公司)监测BIS。麻醉诱导:静脉注射咪达唑仑(江苏恩华药业,批号:20140405)0.03 mg/kg,面罩吸氧去氮,氧流量6 L/min,调节七氟烷挥发罐刻度至6%,预充呼吸环路30 s后,面罩吸入七氟烷(上海恒瑞医药,批号:65131204),每15 s递减0.5%,直至3%,密切观察患儿呼吸幅度和频率,如出现呼吸抑制(呼吸频率<10次/min)即行辅助通气。待患儿睫毛反射消失,1 min内静脉缓慢注射瑞芬太尼(湖北宜昌人福药业,批号:120807)2 μg/kg,30 s后停止吸入七氟烷,气管插管后进行机械通气,氧流量为1 L/min。所有操作均由一名熟练掌握气管插管技术的麻醉医师完成。于麻醉诱导前、气管插管后即刻和插管后3 min,记录MAP、HR、SpO2和BIS;记录从开始吸入七氟烷到睫毛反射消失的时间;记录一次气管插管成功情况,采用Viby-Mogensen评分法[1]评价气管插管条件(表1)。
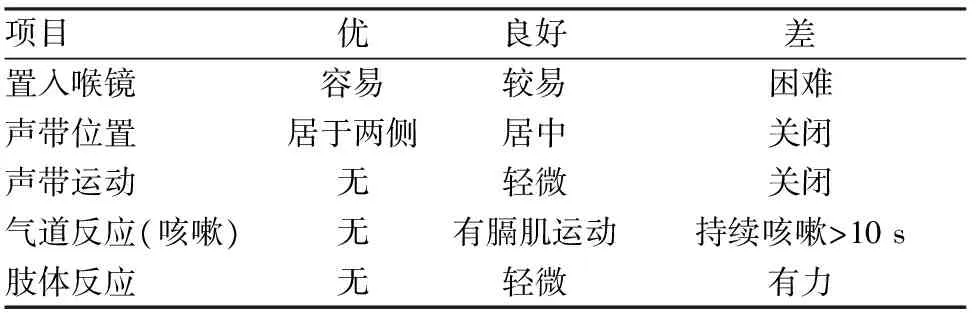
表1 气管插管条件的Viby-Mogensen评分法

2 结 果
睫毛反射消失时间为(58±10) s,一次气管插管成功率为98%。喉镜置入顺利,声门暴露基本良好,气管插管条件优良率为94%。与麻醉诱导前比较,气管插管后3 min MAP降低(P=0.045);气管插管后即刻、气管插管后3 min HR明显降低,差异有统计学意义(P=0.038,P=0.030);气管插管后即刻、气管插管后3 min SpO2无明显变化;气管插管后即刻、气管插管后3 min BIS明显降低,差异有统计学意义(P=0.012,P=0.009),见表2。麻醉诱导期所有患儿未见喉痉挛、支气管痉挛、恶心呕吐及胸壁肌肉强直等现象发生。

表2 短小手术患儿MAP、HR、SpO2和BIS不同时间点的比较 (n=40;
注:与麻醉诱导前比较,①P<0.05,1 mmHg=0.133 kPa
3 讨 论
咪达唑仑为苯二氮卓类镇静药,通过与苯二氮卓受体结合发挥抗焦虑、镇静、催眠甚至意识消失等作用[2]。七氟烷的血/气分配系数较低(0.63),起效快、可控性好,易于麻醉深度的调节,七氟烷诱导后插管期间引起的血流动力学变化较小,不良反应少[3]。瑞芬太尼为μ型阿片受体激动药,在人体内1 min左右迅速达到血-脑平衡,在组织和血液中被迅速水解,故起效快,维持时间短,与催眠药、吸入性麻醉药和苯二氮卓类药物合用有协同作用[4]。本研究参照文献[5]介绍的方法调节七氟烷挥发罐刻度为6%,预充呼吸环路30 s后,每15 s递减0.5%,直至3%。咪达唑仑和瑞芬太尼的剂量选择参照文献[6,7]。
患儿在实施手术前常常焦虑、恐惧、哭闹,对麻醉和手术不配合,本研究中,在面罩吸氧去氮前静脉注射咪达唑仑可消除患儿紧张情绪。有研究表明,七氟烷复合2 μg/kg瑞芬太尼可用于无肌松条件下行快速诱导气管插管[8]。BIS值可反映镇静深度,40~60时可满足气管插管条件。本研究结果表明,所有患儿均顺利完成气管插管,气管插管条件达优率为94%,气管插管期间血液动力学波动小,提示小剂量咪达唑仑、七氟烷复合瑞芬太尼麻醉诱导平稳,提供了较好的气管插管条件,且各时间点SpO2均>92%,气管插管后即刻至3 min BIS值维持46~58,气管插管诱发的心血管反应较小。
咪达唑仑的分布半衰期为5~10 min,对血液动力学影响小,可降低心率变异性[7],七氟烷起效快,呼吸抑制及对呼吸道的刺激作用均较弱,瑞芬太尼的分布半衰期为1 min,起效快,清除也快(仅10 min),不论静脉输注时间多长,体内无蓄积,可有效抑制气管插管和手术刺激引起的神经内分泌应激反应[9]。七氟烷复合瑞芬太尼不仅可加强镇静效果,还可抑制气管插管反应[6]。本研究依次应用咪达唑仑、七氟烷联合瑞芬太尼麻醉诱导,在三者的药物作用达到高峰时进行气管插管,患儿的血压与心率相对下降,且维持平稳,可以维持血液动力学的相对稳定。说明七氟烷、咪达唑仑、瑞芬太尼麻醉诱导用于短小手术患儿无肌松药气管插管时,气管插管条件良好。因此,三种药物复合应用可提供较好的气管插管条件。另外,本研究未出现喉痉挛、支气管痉挛、恶心呕吐及胸壁肌肉强直等现象,可能与三者的用药顺序及时间有关,这尚待进一步研究。
综上所述,七氟烷-咪达唑仑-瑞芬太尼麻醉诱导迅速而平稳,可提供良好的气管插管条件,对于短小手术患儿无肌松药气管插管,安全可行。
[1] Viby-Mogensen J, Engbaek J, Eriksson L I,etal. Good clinical research practice(GCRP) in pharmacodynamic studies of neuromuscular blocking agents [J]. Acta Anaesthesiol Scand, 1996,40(1):59-74.
[2] Isik B, Baygin O, Kapci E G,etal. The effects of temperament and behaviour problems on sedation failure in anxious children after midazolam premedication [J]. Eur J Anaesthesiol, 2010,27(4):336-340.
[3] Mgrtin-Larrauri R, Gilsanz F, Rodrigo J,etal. Conventional stepwise vs. vital capacity rapid inhalation induction at two concentrations of sevoflurane [J]. Eur J Anaesthesiol, 2004,21(4):265-271.
[4] Mohrien K M, Jones G M, Macdermott J R,etal. Remifentanil, ketamine, and fospropofol: a review of alterative continuous infusion agents for sedation in the critically Ⅲ [J]. Critical Care Nursing Quarterly, 2014,37(2):137-151.
[5] Calderon E, Torres L M, Calderon-Pla E. Comparative study of inhalation induction by vital capacity breath in adults using 6% sevoflurane with oxygen or 4.5% sevoflurane in 50% nitrous oxide [J]. Rev Esp Anestesiol Reanim, 1999,46(7):282-285.
[6] Munoz H R, Gonzalez J A, Concha M R,etal. Hemodynamic response to tracheal intubation after vital capacity rapid inhalation induction (VCRⅡ) with different concentrations of sevoflurane [J]. J Clin Anesth, 1999,11(7):567-571.
[7] Nishiyama T, Matsukawa T, Yokoyama T,etal. Rapid inhalation induction with 7%sevoflurane combined with intravenous midazolam [J]. J Clin Anesth, 2002,14(4):290-295.
[8] Hwan S J, William J P, Susan E B. Sevoflurane with remifentanil allows rapid tracheal intubation without neuromuscular blocking agents[J]. Can J Anaesth, 2001,48(7):646-650.
[9] 贾 杰,胡祖荣,邓 恋,等.瑞芬太尼复合七氟醚在新生儿全身麻醉中的应用[J]. 临床小儿外科杂志,2010,9(6):464-465.
(2014-10-13收稿 2014-10-24修回)
(责任编辑 付 辉)
Effect of anesthesia induction with sevoflurane-midazolam-remifentanil for tracheal intubation without muscle relaxants in children with short operation
YIN Caixing and SI Xiaomeng.
Department of Anesthesiology, Nanyang City Center Hospital, Nanyang 473000, China
Objective To analyze the effect of anesthesia induction with sevoflurane-midazolam-remifentanil for tracheal intubation without muscle relaxants in children with short operation. Methods Forty children patients, American Society of Anesthesiologists(ASA)score Ⅰ or Ⅱ, scheduled for surgery under general anesthesia. Anesthesia was induced with intravenous injection of midazolam 0.03 mg/kg . Sevoflurane was inhaled through a mask at the initial concentration of 6%,followed by decrement of 0.5% every 15 seconds until 3%.When the eyelash reflex disappeared,remifentanil 2 μg/kg was injected slowly through veins in 1 minute and 30 seconds later sevoflurane inhalation was stopped.The children patients were mechanically ventilated after tracheal intubation.The values of mean artery pressure(MAP), heart rate(HR), pluse oxygen saturation(SpO2), and bispectral index(BIS) at the time of before anesthesia induction, tracheal intubation immediately and 3 minutes after intubation were recorded. The time of disappearance of eyelash reflex was recorded. The intubation condition was evaluated. Results The time period from sevoflurane inhalation to disappearance of eyslash reflex of all children patients was (58±10) seconds.The satisfactory rate of tracheal intubation conditions was 94%. Compared with the time of before anesthesia induction, the value of MAP decreased (P=0.045) at the time of 3 minutes after intubation, the value of HR (P=0.038,P=0.030), BIS (P=0.012,P=0.009) were significantly reduced at the time of tracheal intubation immediately and 3 minutes after intubation. Conclusions Anesthesia induction with sevoflurane-midazolam-remifentanil was rapid and smooth,could provide good conditions for tracheal intubation, which was safe and feasible for tracheal intubation without mascle relaxants in children with short operation.
sevoflurane;midazolam;remifentanil;tracheal intubation;children with short operation
10.13919/j.issn.2095-6274.2014.10.004
尹彩星,硕士,住院医师,E-mail:yincx0408@163.com
473000,河南省南阳市中心医院麻醉科
R9;R614
